US Insurer Spending on Ivermectin Prescriptions for COVID-19
By Kao-Ping Chua, MD, PhD, Rena M. Conti, PhD, and Nora V. Becker, MD, PhD
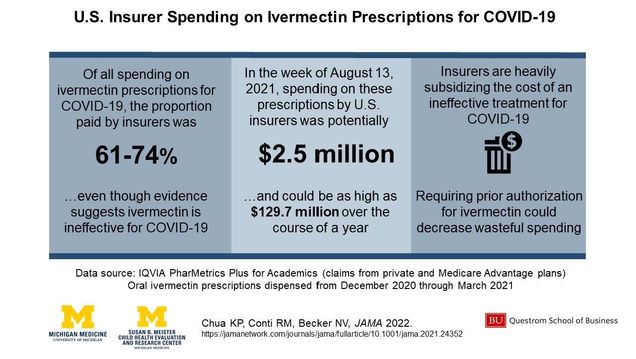
Insurers heavily subsidize the cost of ivermectin prescriptions for COVID, despite the lack of evidence that ivermectin is effective for COVID.
In a new paper, published in JAMA, Questrom professor and TPRI co-lead Rena Conti with colleagues Kao-Ping Chua and Nora Becker (both University of Michigan) estimate that U.S. insurers may have wasted $2.5 million on these drugs in the week of August 13, 2021 alone.
The authors find that before COVID, 3,600 ivermectin prescriptions were dispensed in the U.S per week. Weekly dispensing spiked in December 2020 and reached 88,000 in the week of August 13, 2021.
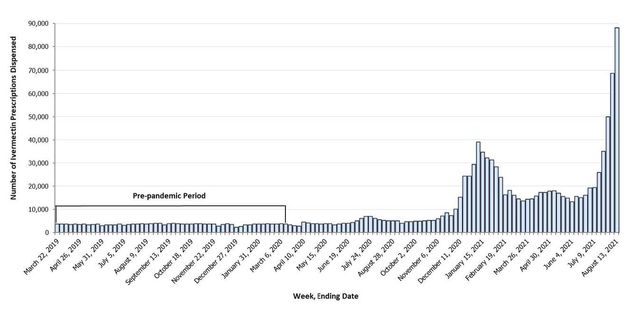
This surge in ivermectin dispensed prescriptions occurred even though the efficacy of ivermectin for COVID treatment or prevention has not been established in randomized clinical trials, nor FDA approved as safe and efficacious for COVID. Normally, insurers don’t cover treatments without evidence of efficacy. The authors wanted to know whether insurers are treating ivermectin for COVID in the usual way.
Conti and colleagues data suggest insurers are not following the usual protocol. Based on their analysis of private insurance and Medicare Advantage claims from Dec 2020-Mar 2021, they estimate that insurers paid 61-74% of the cost of ivermectin Rx for COVID-19 ($36-39 per Rx), with the remainder paid by patients. Based on insurer reimbursement per dispensed prescription, the authors estimated how much U.S. private and Medicare plans might have paid for ivermectin in the week of August 13, 2021, the last week in which national dispensing data were available. To do this, they assumed that all but 3,600 (the pre-pandemic mean) of the 88,000 ivermectin dispensed prescriptions in this week were for COVID-19, that the distribution of payer type for ivermectin Rx mirrored that of drugs more broadly, and that their estimates generalized to all insurance plans.
Under these (strong) assumptions, Conti and colleagues estimate U.S. private and Medicare plans spent $2.5 million in that week alone. This extrapolates to $129.7 million over the course of a year. For comparison, this amount could exceed annual Medicare spending for unnecessary imaging for low-back pain ($82 million), a low-value service that receives considerable attention from policymakers and clinicians.
The authors believe the true amount of wasted spending on ivermectin may be higher because 1) they didn’t consider Medicaid spending, and 2) by reducing barriers to an ineffective drug that some use as a substitute for COVID vaccination, insurers may raise their spending on COVID complications. Also, if ivermectin dispensing follows COVID case counts, then it’s quite possible that there are more ivermectin prescriptions per week now in the middle of the Omicron wave where the U.S. currently has > 700k cases/daily.
One solution would be for insurers to require prior authorization for ivermectin. While this could impede ivermectin use for evidence-based indications, the number of people affected would likely be small, as suggested by the very low levels of ivermectin dispensing before COVID. For that reason, imposing prior authorization for ivermectin may be one of the rare policy solutions with a lot of potential benefits and few potential costs.
To be clear, clinicians can prescribe ivermectin for COVID if they want. In these situations, the authors are arguing that patients should pay for ivermectin out-of-pocket. If insurers pay, they force others to subsidize the cost of ineffective care via higher premiums/taxes.
Finally, paying for ineffective COVID treatments makes little sense given that insurers are trying to lower their COVID-related costs by abandoning cost-sharing waivers for COVID hospitalizations, leaving patients with huge bills.
Twitter: @NoraBeckerMD @contirena1 @UMchear @UM_IHPI @UM_VBID @sarahkliff.
References
Chua K, Conti RM, Becker NV. US Insurer Spending on Ivermectin Prescriptions for COVID-19. JAMA. Published online January 13, 2022. doi:10.1001/jama.2021.24352