2022 URBAN ARCH Annual Meeting
On May 10, 2022, URBAN ARCH held its annual meeting. A total of 87 attendees participated in the event, which marked the end of the URBAN ARCH Consortium and the launch of the three new 2nd generation URBAN ARCH HIV/Alcohol P01 Centers: International URBAN ARCH, ARCHER, and META HIV CVD. During the 2022 Annual Meeting, investigators from each of our three URBAN ARCH Consortium cohorts in Mbarara (Uganda), St. Petersburg (Russia, remotely), and Boston (USA) presented on key findings from their studies. We share a few of those findings with you below and encourage you to peruse our publications page to explore other topics and research questions examined over the past 10 years. The rich data (and samples) collected as part of the Consortium are available for interested investigators in our repository. If you are looking to lead an analysis with existing URBAN ARCH data, please read on for a list of potential analysis ideas.
What is the impact of alcohol on HIV disease progression and clinical outcomes?
The URBAN ARCH Consortium has investigated the impact of alcohol on HIV disease progression and clinical outcomes across the globe. In Mbarara, Uganda, among people with HIV (PWH) who were not on antiretroviral therapy (ART), unhealthy alcohol use was not found to be associated with pre-ART CD4 decline (Hahn et al., 2018) or with tryptophan metabolism (Pierre et al., 2022). However, unhealthy alcohol use was associated with monocyte activation (Carrico et al., 2015). Among PWH who were on ART, alcohol use was associated with liver enzyme elevations (Freiman et al., 2021), but unhealthy alcohol use was not associated with viral suppression (Foley et al., 2020). These effects of alcohol use on PWH are important, given the high prevalence of co-morbid liver disease among PWH.
Traveling north approximately 6,000 miles, in St. Petersburg, alcohol use among PWH was found to be associated with higher levels of inflammatory biomarkers including sCD14, IL-6, and D-dimer (So-Armah et al., 2019). Slower CD4 recovery after ART initiation was also observed among PWH with greater alcohol use (McLaughlin et al., 2022).
Finally, 4,000 miles west across Europe and the Atlantic Ocean, the URBAN ARCH Consortium’s Boston ARCH Cohort found that substance use disorder – but not substance use – was associated with detectable HIV viral load. This finding suggests that poor HIV virologic control is driven by the effect of substance use on one’s life rather than use itself, in this population (Nolan et al., 2017).
The Boston ARCH team also examined lifetime and recent alcohol use and bone mineral density (BMD) among people with HIV and SUD or a lifetime history of injection drug use. They found that when examined cross-sectionally, recent alcohol use – rather than lifetime alcohol consumption – was associated with low BMD (Ventura et al., 2017). However, when examining annual change in BMD, no significant associations were observed between past-year alcohol consumption and annual change in BMD (Saitz et al., 2018). Greater alcohol consumption was associated with lower levels of bone formation markers (Kim et al., 2020). In contrast to previous findings, there were no threshold effects. In other words, the risk was linear even with no alcohol use.
Other Key Findings

In Uganda, high risk alcohol use was associated with latent TB infection (Puryear et al., 2021), but not moderate risk alcohol use (Muyindike et al., 2020). Among individuals on INH (TB preventive therapy), unhealthy alcohol use was associated with poor INH adherence (Muyindike et al., 2022). PWH who were engaging in high risk drinking may be at higher risk for TB infection and poorer adherence to INH. A modeling study in Uganda showed more benefit than risk of INH among PWH who consume alcohol in high TB incidence settings (Freiman et al., 2018), therefore PWH should get INH in these settings, regardless of alcohol use.
Potential drawbacks of self-reported alcohol consumption are important to consider. Concern for under-reporting of alcohol use exists in HIV and alcohol research. Uganda ARCH investigators found that medium and higher (compared to low) levels of social desirability, defined as the tendency for people to present themselves in a generally favorable fashion, were associated with decreased AUDIT-C scores when adjusted for phosphatidylethanol, or PEth – a biomarker of alcohol use (Adong et al., 2019; Hahn et al., 2016; Muyindike et al., 2017). Social desirability was found to potentially be associated with lower odds of self-reported alcohol use among women (Adong et al., 2019).

In the ZINC HIV RCT, Dr. Freiberg and team found that daily zinc supplementation taken for 18 months did not reduce mortality risk, increase CD4 cell counts, lower cardiovascular disease risk, or reduce levels of inflammation and microbial translocation in PWH with heavy alcohol use who were ART-naïve at baseline when examined at the 18-month timepoint (Freiberg et al., 2020).
In Russia, stigma related to substance use and HIV was examined among people who inject drugs (PWID) living with HIV. Poor mental health and unhealthy alcohol use were correlated with high stigma (Lunze et al., 2018), while intersectional (HIV and substance use) stigma was associated with less care utilization (Vetrova et al., 2021). A hopeful finding was that a behavioral stigma coping intervention was found to increase ART initiation and substance use care engagement (Rossi et al., 2022).
The Boston 4F Study: Falls, Fractures, Frailty, Functioning examined associations between alcohol and illicit drug use, polypharmacy, and falls and acute healthcare utilization (which included emergency department use and hospitalization) for falls and fractures. Illicit opioids and sedatives were found to be associated with falls and acute health care utilization among HIV-positive adults with SUD. A cross-cohort study of Boston ARCH and Russia ARCH data found that each additional number of alcohol use disorder (AUD) criteria was associated with a fall. Homelessness was also associated with a fall in the Boston ARCH cohort. These findings suggest that addressing homelessness and addiction severity among PWH may reduce acute care utilization (Thakarar et al., 2020).
Remaining Questions
URBAN ARCH Consortium investigators worked diligently over the past 10 years to build robust cohorts of PWH in Uganda, Russia, and Boston. As the consortium draws to a close, unanswered questions remain. These are ripe opportunities for collaboration if you or someone on your team is looking to lead an analysis.
Uganda ARCH Cohort:
- How to avoid TB infection among PWH with high risk alcohol use?
- How to improve INH adherence among PWH who consume alcohol?
- Can financial incentives overcome social pressures to drink?
- How to reduce alcohol use and its impact on HIV and HIV co-morbidities – TB and liver diseases?
- Best ways to detect and account for social desirability?
- Ways to reduce socially desirable reporting in research and clinical care?
- How to factor in biologic variability in alcohol metabolism when using biomarkers?
- How best to use alcohol biomarkers and self-report in HIV research?
- Can biomarkers be integrated into clinical care?
- How to consider the context of the social pressures around alcohol use?
Boston ARCH Cohort:
- Examine the impact of alcohol (and other drugs, polypharmacy) use on frailty and physical functioning among PWH
- Identify associations between frailty (or poor functioning) and outcomes
- Do relationships differ by substance use/disorder or substance type?
- What are resiliency factors in whom frailty does not lead to falls, hospitalization, declining physical functioning?
Russia ARCH Cohort:
- What are the impacts of alcohol and tobacco use on pain and other HIV symptoms?
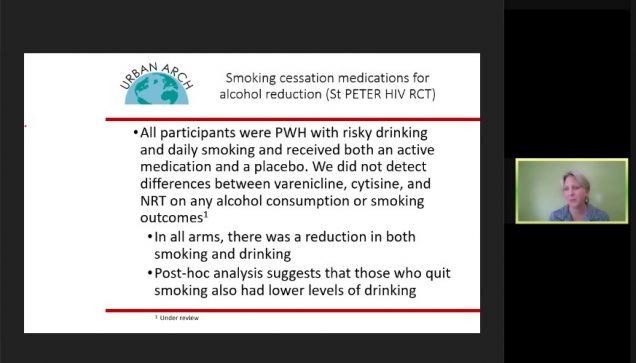
- Will changes in use of one substance prompt change in use of other substances among people who co-use substances?
- What are the impacts of social determinants of health among Russian PWH who inject drugs?
- The association between liver fibrosis and microbiome dependent metabolites e.g., trimethylamine N-oxide (TMAO)
- Examine oxidative stress, alcohol, smoking, and cardiac function
- Opioid exposure and cardiac structure and function with extensive cardiac echo data
If you were unable to attend the 2022 URBAN ARCH Annual Meeting, or would like to review the slides after attending, please visit our page linked here. If you are interested in collaborating with us in the future, please contact us!
Citations:
Adong J, Fatch R, Emenyonu NI, Cheng DM, Muyindike WR, Ngabirano C, Kekibiina A, Woolf-King SE, Samet JH, Hahn JA. Social desirability bias impacts self-reported alcohol use among persons with HIV in Uganda. Alcohol Clin Exp Res. 2019 Dec;43(12):2591–2598. PMCID: PMC7411366
Carrico AW, Hunt PW, Emenyonu NI, Muyindike W, Ngabirano C, Cheng DM, Winter MR, Samet JH, Hahn JA. Unhealthy alcohol use is associated with monocyte activation prior to starting antiretroviral therapy. Alcohol Clin Exp Res. 2015 Dec;39(12):2422–2426. PMCID: PMC4712082
Foley JD, Sheinfil A, Woolf-King SE, Fatch R, Emenyonu NI, Muyindike WR, Kekibiina A, Ngabirano C, Samet JH, Cheng DM, Hahn JA. Assessing the interaction between depressive symptoms and alcohol use prior to antiretroviral therapy on viral suppression among people living with HIV in rural Uganda. AIDS Care. 2020 Oct;32(10):1251–1257. PMCID: PMC7972246
Freiberg MS, Cheng DM, Gnatienko N, Blokhina E, Coleman SM, Doyle MF, Yaroslavtseva T, Bridden C, So-Armah K, Tracy R, Bryant K, Lioznov D, Krupitsky E, Samet JH. Effect of zinc supplementation vs placebo on mortality risk and HIV disease progression among HIV-positive adults with heavy alcohol use: A randomized clinical trial. JAMA Network Open. 2020 May 8;3(5):e204330.
Freiman JM, Fatch R, Cheng D, Emenyonu N, Ngabirano C, Geadas C, Adong J, Muyindike WR, Linas BP, Jacobson KR, Hahn JA. Prevalence of elevated liver transaminases and their relationship with alcohol use in people living with HIV on anti-retroviral therapy in Uganda. PLoS One. 2021;16(6):e0250368. PMCID: PMC8168875
Freiman JM, Jacobson KR, Muyindike WR, Horsburgh CR, Ellner JJ, Hahn JA, Linas BP. Isoniazid preventive therapy for people with HIV who are heavy alcohol drinkers in high TB-/HIV-burden countries: A risk–benefit analysis. J Acquir Immune Defic Syndr. 2018 Apr 1;77(4):405–412.
Hahn JA, Cheng DM, Emenyonu NI, Lloyd-Travaglini C, Fatch R, Shade SB, Ngabirano C, Adong J, Bryant K, Muyindike WR, Samet JH. Alcohol use and HIV disease progression in an antiretroviral naive cohort. J Acquir Immune Defic Syndr. 2018 Apr 15;77(5):492–501. PMCID: PMC5844835
Hahn JA, Emenyonu NI, Fatch R, Muyindike WR, Kekiibina A, Carrico AW, Woolf-King S, Shiboski S. Declining and rebounding unhealthy alcohol consumption during the first year of HIV care in rural Uganda, using phosphatidylethanol to augment self-report. Addiction. 2016 Feb;111(2):272–279. PMCID: PMC4715487
Kim TW, Ventura AS, Winter MR, Heeren TC, Holick MF, Walley AY, Bryant KJ, Saitz R. Alcohol and bone turnover markers among people living with HIV and substance use disorder. Alcohol Clin Exp Res. 2020 Apr;44(4):992–1000. PMCID: PMC7263383
Lunze K, Lodi S, Gnatienko N, Lloyd-Travaglini C, Bendiks S, Vetrova M, Toussova O, Bushara N, Blokhina E, Ekstrand ML, Luoma J, Krupitsky EM, Lioznov D, Samet JH. Determinants of HIV and substance use stigma among people with a history of substance use who are living with HIV in Russia. Poster Presentation presented at: 22nd International AIDS Conference; 2018; Amsterdam, Netherlands.
McLaughlin A, Lin N, Jiang W, Lodi S, Lioznov D, Patts G, Cheng DM, Gnatienko N, Blokhina E, Bendiks S, Freiberg M, Tindle HA, Krupitsky E, Samet JH, So-Armah K. Effect of alcohol consumption on CD4 recovery after antiretroviral therapy (ART) initiation in people living with HIV (PLWH). Poster Presentation presented at: URBAN ARCH Annual Meeting; 2022; Virtual.
Muyindike W, Fatch R, Cheng DM, Emenyonu NI, Forman L, Ngabirano C, Adong J, Linas B, Jacobson KR, Hahn JA. Alcohol use and suboptimal adherence to isoniazid in persons with HIV and latent TB. Poster Presentation presented at: Conference on Retroviruses and Opportunistic Infections; 2022; Virtual.
Muyindike W, Fatch R, Cheng DM, Emenyonu NI, Ngabirano C, Adong J, Linas BP, Jacobson KR, Hahn JA. Tuberculin skin test positivity among HIV-infected alcohol drinkers on antiretrovirals in south-western Uganda. PLoS One. 2020 Jul 2;15(7):e0235261. PMCID: PMC7332058
Muyindike W, Lloyd-Travaglini C, Fatch R, Emenyonu NI, Adong J, Ngabirano C, Cheng DM, Winter MR, Samet JH, Hahn JA. Phosphatidylethanol confirmed alcohol use among ART-naïve HIV-infected persons who denied consumption in rural Uganda. AIDS Care. 2017 Nov;29(11):1442–1447. PMCID: PMC5554736
Nolan S, Walley AY, Herren TC, Patts GJ, Ventura AS, Sullivan MM, Samet JH, Saitz R. HIV-infected individuals who use alcohol and other drugs, and virologic suppression. AIDS Care. 2017 Sep;29(9):1129–1136. PMCID: PMC5543330
Pierre F, Forman LS, Winter M, Cheng D, Ngabirano C, Emenyonu N, Hunt PW, Huang Y, Muyindike W, Samet J, Hahn JA, So-Armah K. Alcohol consumption and tryptophan metabolism among people with HIV prior to antiretroviral therapy initiation: The Uganda ARCH Cohort Study. Alcohol Alcohol. 2022 Mar 12;57(2):219–225. PMCID: PMC8919408
Puryear SB, Fatch R, Beesiga B, Kekibiina A, Lodi S, Marson K, Emenyonu NI, Muyindike WR, Kwarisiima D, Hahn JA, Chamie G. Higher levels of alcohol use are associated with latent tuberculosis infection in adults living with human immunodeficiency virus. Clin Infect Dis. 2020 May 6;72(5):865–868. PMCID: PMC7935375
Rossi SL, Luoma JB, Sereda Y, Pavlov N, Toussova O, Vetrova M, Bendiks S, Kiriazova T, Krupitsky E, Lioznov D, Blokhina E, Lodi S, Lunze K. Acceptance-based, intersectional stigma coping intervention for people with HIV who inject drugs – an RCT in St. Petersburg, Russia. Poster Presentation presented at: 24th International AIDS Conference; 2022; Montreal, Canada.
Saitz R, Mesic A, Ventura AS, Winter MR, Heeren TC, Sullivan MM, Walley AY, Patts GJ, Meli SM, Holick MF, Kim TW, Bryant KJ, Samet JH. Alcohol consumption and bone mineral density in people with HIV and substance use disorder: A prospective cohort study. Alcohol Clin Exp Res. 2018 Jun 6; PMCID: PMC6281811
So-Armah KA, Cheng DM, Freiberg MS, Gnatienko N, Patts G, Ma Y, White L, Blokhina E, Lioznov D, Doyle MF, Tracy RP, Chichetto N, Bridden C, Bryant K, Krupitsky E, Samet JH. Association between alcohol use and inflammatory biomarkers over time among younger adults with HIV—The Russia ARCH Observational Study. PLoS One. 2019 Aug 22;14(8):e0219710. PMCID: PMC6705834
Thakarar K, Walley AY, Heeren TC, Winter MR, Ventura AS, Sullivan M, Drainoni M, Saitz R. Medication for addiction treatment and acute care utilization in HIV-positive adults with substance use disorders. AIDS Care. 2020 Sep;32(9):1177–1181. PMCID: PMC7198361
Ventura AS, Winter MR, Heeren TC, Sullivan MM, Walley AY, Holick MF, Patts GJ, Meli SM, Samet JH, Saitz R. Lifetime and recent alcohol use and bone mineral density in adults with HIV infection and substance dependence. Medicine (Baltimore). 2017 Apr;96(17):e6759. PMCID: PMC5413268
Vetrova MV, Cheng DM, Bendiks S, Gnatienko N, Lloyd-Travaglini C, Jiang W, Luoma J, Blokhina E, Krupitsky E, Lioznov D, Ekstrand ML, Raj A, Samet JH, Lunze K. HIV and substance use stigma, intersectional stigma and healthcare among HIV-Positive PWID in Russia. AIDS Behav. 2021 Sep;25(9):2815–2826. PMCID: PMC8316484