URBAN ARCH P01 Submissions Overview
As the URBAN ARCH Consortium enters its 10th year, its investigators are looking ahead to the next round of important questions to be addressed in the realm of HIV/alcohol research. In November, URBAN ARCH investigators submitted three P01 applications in response to RFA-AA-20-009, to shed light on alcohol’s impact on key HIV comorbidities: tuberculosis, chronic pain, physical inactivity, and cardiovascular disease. Here is what the investigators hope to accomplish.
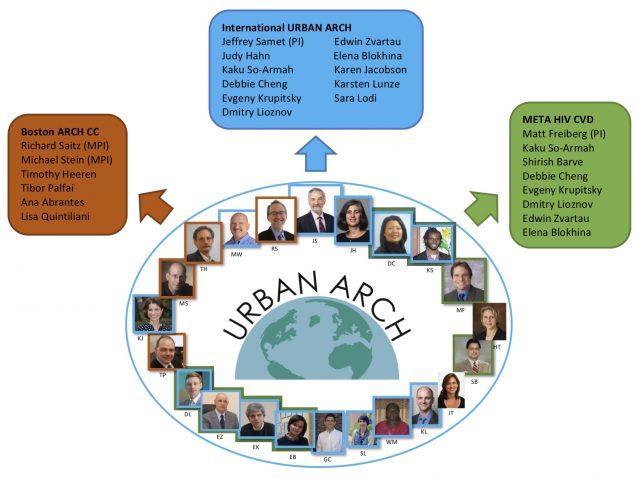
Boston Alcohol Research Collaboration on HIV/AIDS – Comorbidity Center (Boston ARCH CC)
PI and Project Leads: Richard Saitz (MPI); Michael Stein (MPI); Timothy Heeren (Project Lead); Tibor Palfai (Project Lead); Ana Abrantes (Project Co-Lead); Lisa Quintiliani (Project Co-Lead)
Overview: The primary objective of the Boston ARCH CC is to conduct state-of-the-art e-health clinical trials research to address chronic pain and physical inactivity, two HIV-associated conditions that have a critical impact on a variety of other HIV-related comorbidities, in people living with HIV (PLWH) with unhealthy alcohol use. Secondarily, the Boston ARCH CC will support secondary analyses of the existing Boston ARCH cohort data and provide support and mentoring to trainees and investigators interested in scientific questions related to pain, physical inactivity, and physical and mental functioning. The Boston ARCH CC contains 4 integrated components that will make unique contributions to the objectives: 1) Research Project Component – Pain (Project Lead: Tibor Palfai) tests the efficacy of an integrated behavioral e-health intervention for reducing heavy drinking and chronic pain among PLWH in a randomized controlled trial, 2) Research Project Component – Physical Activity (Project Co-Leads: Lisa Quintiliani/Ana Abrantes) tests the efficacy of a home-based lifestyle physical activity intervention for decreasing physical inactivity and unhealthy drinking, 3) an Administrative Core (Project Co-Leads: Richard Saitz/Michael Stein) which coordinates the P01, and 4) a Biostatistics and Data Management Core (Project Lead: Timothy Heeren) that supports the trials methodologically and continues secondary analyses using extant Boston ARCH data.
The International Uganda Russia Boston Alcohol Network for Alcohol Research Collaboration on HIV/AIDS (URBAN ARCH) Center
PI and Project Leads: Jeffrey Samet (PI); Debbie Cheng (Core Director); Judy Hahn (Project Lead); Kaku-So-Armah (Project Lead)
Overview: The central goal of the International URBAN ARCH Center is to examine the role of alcohol use on new tuberculosis (TB) acquisition, occurrence of active TB disease after TB preventative therapy (TPT), and post-TB lung disease among people living with HIV (PLWH). This new knowledge will enable future development of interventions that can reduce alcohol’s impact on TB-related morbidity and mortality among PLWH. The Center will be comprised of 4 components (Administrative Core, Biostatistics and Data Management [BDM] Core, Uganda Project, Russia Project) that will work synergistically to accomplish the following primary objectives: 1) Examine the role of alcohol use in driving the acquisition of new TB infection and the occurrence of active TB disease after TPT in PLWH in Uganda (Uganda Project led by Judy Hahn); 2) Determine the relationship between alcohol use and lung disease after treatment for active TB disease among PLWH in Russia (Russia Project led by Kaku So-Armah); 3) Conduct high quality data management and statistical analyses for HIV/alcohol research (BDM Core led by Debbie Cheng); 4) Foster multidisciplinary international collaborations to promote innovative and rigorous HIV/alcohol research (Administrative Core led by Jeffrey Samet); and 5) Provide ongoing training and mentoring to develop junior and mid-career investigators into future leaders in HIV/alcohol research.
Microbiome, mETabolites, and Alcohol in HIV to reduce CVD (META HIV CVD) Program Project Grant
PI and Project Leads: Matthew Freiberg (PI, Administrative Core Lead, Project Lead); Shirish Barve (Laboratory Core Director, Co-director Administrative Core); Kaku-So-Armah (Project Lead)
Overview: The overarching theme for this program project grant (PPG) is that alcohol associated gut dysbiosis and gut dysbiotic metabolites are cardiovascular disease (CVD) risk factors among people living with HIV infection (PLWH) who are heavy drinkers. The goals of this research are (1) to determine if a tailored probiotic (i.e., contains bacteria supporting butyrate synthesis) can mitigate alcohol associated gut dysbiosis and lower levels of microbial translocation, inflammation, and improve harmful dysbiotic metabolite profiles (e.g. trimethylamine N oxide, TMAO) and (2) to determine if these metabolites are associated with incident CVD and death among PLWH. We hypothesize that, among PLWH, a probiotic vs. placebo can mitigate alcohol associated gut dysbiosis and lower levels of microbial translocation, inflammation, and improve metabolite profiles and that harmful alterations of these metabolites will be associated with higher risk of incident CVD and death. Project 1 will be conducted at Pavlov State Medical University in St. Petersburg, Russia, the same site as our gut microbiome and metabolite studies (ACME HIV and TMAO HIV). Project 2 will leverage the Veterans Aging Cohort Study, an observational cohort of veterans living with and without HIV. The Projects will be supported by our Administrative Core at Vanderbilt University Medical Center and the Integrated Metagenomics and Metabolomics Core at the University of Louisville’s Alcohol Research Center (ULARC). Biospecimens from Project 1 will be used to validate significant findings in Project 2. Metabolites significantly associated with alcohol and CVD in Project 2, will be explored in Project 1 to see if probiotics favorably impact the levels of those metabolites. The META HIV CVD PPG will inform probiotics’ role as standard adjunctive therapy complementing alcohol interventions among PLWH who are heavy drinkers and advance the understanding of how alcohol associated gut dysbiosis and its metabolites contribute to CVD and death.
Please click on the figure above for a closer look!