Category: Uncategorized
Glutamate Excitotoxicity and Ischemic Stroke

Glutamate is the major excitatory neurotransmitter utilized by the human nervous system and is involved in many important neurological functions. Best known for its role in memory formation and Long Term Potentiation (LTP), glutamate signaling is crucial for healthy brain activity. Despite glutamate’s importance in our everyday lives, too much glutamate can actually kill neurons, leading to stroke and death. This phenomenon is known as glutamate excitotoxicity.
In the synapse, a gap between two neurons, the presynaptic neuron releases neurotransmitters such as glutamate onto the receptors of the postsynaptic neuron. Glutamate will bind to two types of receptors on the postsynaptic neuron: ionotropic glutamate receptors (iGluRs) and metabotropic glutamate receptors (mGluRs). iGluRs are the most well-known receptors through which glutamate exerts its effect. mGluRs can either upregulate or downregulate the effects of glutamate signaling based on their receptor type. The mGluRs deserve a separate blog post due to their complex mechanisms, and this post will focus exclusively on iGluRs in glutamate excitotoxicity.
Glutamate will activate two types of iGluRs: AMPA and NMDA receptors. In a healthy synapse, a regulated amount of glutamate is released from the presynaptic neuron with a concentration high enough to elicit a response in the postsynaptic neuron but low enough to not cause cytotoxicity. Activation of AMPA receptors allows sodium ions to flow into the postsynaptic neuron, depolarizing it. With enough depolarization, the intracellular positive charge forces a magnesium ion out of the pore of an activated NMDA receptor, allowing sodium ions and calcium ions to flow into the neuron. The calcium ion influx is involved in many signaling cascades including activating phosphorylating proteins, regulating gene transcription, recruiting more AMPA receptors to the postsynaptic density, and inducing dendritic spine growth. All of these changes strengthen the synaptic communication between the two neurons. This glutamate dependent mechanism is characteristic of a phenomenon known as long term potentiation (LTP) and is involved in the neurobiology of memory formation in the brain.
Glutamate excitotoxicity occurs when too much glutamate has been released into the synapse. A common mechanism through which this occurs is seen in ischemic stroke. In ischemic stroke, arteries supplying oxygen rich blood to the brain are blocked or narrowed, significantly reducing oxygen delivery. Without oxygen, ATP levels within neurons drop significantly. This is a crucial step in glutamate excitotoxicity due to ATP’s overall negative charge. With less ATP, the interior of the neuron becomes less negatively charged and more positively charged. This unwanted increase in positive charge forces open voltage gated calcium ion channels. An unnecessary influx of calcium ions into the presynaptic neuron causes the release of excess glutamate into the synapse. This excess glutamate overstimulates postsynaptic glutamate receptors, especially NMDA receptors. Abnormally high levels of calcium ions then flood the postsynaptic neuron, activating cytotoxic enzymes including proteases, nucleases, and caspases which proceed to destroy the neuron.
As if things could not get any worse, the damage does not stop with just one neuron. When the neuron dies it releases its own supplies of glutamate throughout the brain, in turn overstimulating and killing other neurons. Glutamate excitotoxicity has now extended its influence from a few neurons to many more neurons in the brain. This vicious cycle of excess glutamate release and neuronal death repeats itself over and over again in a matter of minutes, leading to the characteristic symptoms of stroke including facial drooping, distorted speech, and limb weakness. Without immediate medical intervention, the stroke patient will die within hours. Even with treatment the damage is already done; many stroke survivors are left permanently debilitated and can never return to a healthy, functioning life.
The intricate mechanism of ischemic stroke in all its lethal glory reverberates the old adage that too much of a good thing can be a bad thing. Understanding how glutamate excitotoxicity works is still under intense research, and many questions are still left unanswered. One thing is for sure: more knowledge about glutamate excitotoxicity has far reaching applications in medicine and neuroscience, with the potential to save countless lives.
Writer: Richard Kuang
Editor: Nathaniel Meshberg
Sources:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3985770/
http://www.ajnr.org/content/22/10/1813
https://www.ncbi.nlm.nih.gov/pubmed/14552898
https://www.ncbi.nlm.nih.gov/books/NBK6556/
https://www.mayoclinic.org/diseases-conditions/stroke/symptoms-causes/syc-20350113
The role of physical exercise in preservation of the memory function.

Sports are increasingly widespread in modern-day American Academia. Perhaps, it is the plethora of research on healthy lifestyle, or the anticipation of the beach season, with sentiment ranging from apprehension to excitement to flatout morose ignorance, which we have to thank for this. Alternatively, it may be an amalgamation of those factors (and many others) that brought a drastic improvement of physical vitality as far as college students are concerned. In any case, there is more to it than good looks and capabilities to walk to the fifth floor of, for example, STH, rather than taking an elevator. Participating in some form of consistent physical exercise brings with it an improvement to the quality of memory later on in life, at least as far as men are concerned.
A study by an interdisciplinary group of scientists from Spain showed that long term exercise (35±15 years) promotes the preservation of memory function in middle-aged (47-67) men, specifically concerning the free immediate recall test and cued immediate recall test. The training (athlete) test-group showed a statistically significant increase in performance on both tests compared to the middle-aged sedentary group. Moreover, the number of weekly hours of exercise also showed a positive correlation with test performance. In short, continuous and consistent sports participation goes a long way when it comes to memory.
Having established the benefits for the middle-aged, it would have been nice if there was something in it for the young as well and there is! The very same study, also measuring common biological markers associated with memory impairment, such as plasma lipid peroxidation levels (MDA) and resting serum levels of BDNF, made a number of promising conclusions. For instance, both the middle-aged and young-aged (17-25) sedentary groups scored higher on the blood MDA levels (plasma malondialdehyde, a biomarker that correlates with oxidative damage) - which inversely affects memory. Moreover, a similar pattern (inverse correlation) is observed with BDNF (Brain-derived neurotrophic factor), except here the difference between the young sedentary and athlete groups is significantly higher. While BDNF is considered to promote neuronal growth, the researchers found no significant correlation between BDNF levels and memory test(s) performance but found a positive correlation between BDNF and MDA levels (which is bad). Thus, exercise does not only work for the middle-aged men but also the younger ones.
The most important part of this study is not, in all due technicalities, the uniqueness of its ideas, but rather its scope. Some studies have already shown the beneficial effect of exercise on people's memory, provided they are already suffering from certain conditions, such as Alzheimer's or mild cognitive impairment. Moreover, another set of studies explored the effect of short-term aerobic exercises, mostly targeting attention, decision-making and speed processing. Thus, this study is the first of its kind - exploring the connection between long-term exercise (not acute burst of activity) and memory in healthy men.
Finally, for the sake of objectiveness, limitations of the study should also be discussed. The most obvious drawback is the exclusion of women from the test groups, which subsequently makes this study only relevant for men (until proven otherwise). Moreover, the study itself is of a cross-sectional kind and hence is not impervious to various biases, such as cohort effects (in all due fairness, not many studies ever are).
So, guys, have you been hitting gym lately?
Writer: Ivan Kondratyev
Editor: Audrey Kim
Sources:
Baker, L. D., Frank, L. L., Foster-Schubert, K., Green, P. S., Wilkinson, C. W., Mctiernan, A., . . . Craft, S. (2010). Aerobic Exercise Improves Cognition for Older Adults with Glucose Intolerance, A Risk Factor for Alzheimer's Disease. Journal of Alzheimer's Disease, 22(2), 569-579. doi:10.3233/jad-2010-100768
Ferris, L. T., Williams, J. S., & Shen, C. (2007). The Effect of Acute Exercise on Serum Brain-Derived Neurotrophic Factor Levels and Cognitive Function. Medicine & Science in Sports & Exercise, 39(4), 728-734. doi:10.1249/mss.0b013e31802f04c7
Griffin, É W., Mullally, S., Foley, C., Warmington, S. A., O'mara, S. M., & Kelly, Á M. (2011). Aerobic exercise improves hippocampal function and increases BDNF in the serum of young adult males. Physiology & Behavior, 104(5), 934-941. doi:10.1016/j.physbeh.2011.06.005
Mueller-Steiner, S., Zhou, Y., Arai, H., Roberson, E. D., Sun, B., Chen, J., . . . Gan, L. (2006). Antiamyloidogenic and Neuroprotective Functions of Cathepsin B: Implications for Alzheimer's Disease. Neuron, 51(6), 703-714. doi:10.1016/j.neuron.2006.07.027
Rosa, A. D., Solana, E., Corpas, R., Bartrés-Faz, D., Pallàs, M., Vina, J., . . . Gomez-Cabrera, M. C. (2019). Long-term exercise training improves memory in middle-aged men and modulates peripheral levels of BDNF and Cathepsin B. Scientific Reports, 9(1). doi:10.1038/s41598-019-40040-8
It’s All in Your Gut
People have not placed enough importance on the functions of our microbiome and its effects on our personal health, since it is early in research and not well understood yet. The microbiome is the collection of microorganisms, including bacteria, fungi, and viruses, in our human body. Microbiome means all the genomes of microbes in an environment, while microbiota is supposed to mean the actual organism. Today many are using the term microbiome to mean multiple things, the microbiome, microbiota, and the activities of the microbiome in animals and humans. Microbiome having a broader definition, though not the correct usage of the word. The microbiome in the human gut has shown to have effects on the immune system, overall health, and metabolism in animals and humans. Celiac disease, obesity, type 1 diabetes, and many more diseases are observed in humans with a low diversity microbiome. One observation that is surprising is the effects of different types of gut bacteria on neurobehavior, specifically related to depression, anxiety, and a lower quality of life.
An experiment led by Professor Premysl Bercik with three groups of mice at McMaster University was able to correlate certain gut bacteria with symptoms of depression and anxiety. Two groups of mice, one with no bacteria in their gut in a sterile environment and one with a range of bacteria, were put under stress for 3-21 days. The control group had no bacteria and had not been put under stress. Both groups of no bacteria had no symptoms of depression, while the mice with the normal gut microbiomes showed symptoms of depression and anxiety. Both groups that were under stress had increased levels of corticosterone, a stress hormone, but only the group of mice with normal gut microbiomes showed symptoms. Proving the effects of microbes on neural behavior. Multiple cases have proven microbes affecting mental health in animal models, though little research has been done on humans. Professor Jeroen Raes, professor Sara Vieira-Silva, and their team compared the gut microbiome of 1,054 individuals diagnosed with depression in the Flemish Gut Flora Project at the University of Leuven in Belgium. They found certain bacterial genera depleted or abundant in these individuals. Two that stood out to be the most commonly depleted in these individuals were Coprococcus and Dialister. Raes and his team studied the genomes of bacteria from the human gastrointestinal tract and found that some had the ability to produce neuroactive compounds. They are currently creating a toolbox with computational techniques of what bacteria in the gut can affect neuroactive compounds and the mechanism behind it. An interesting one they found is the ability of the microbiome to produce DOPAC led to better mental health as its function is growing the neurotransmitter dopamine.
Scientists are studying the effects of the environment, food, processed foods, and medications on our microbiome and how the microbiome affects our health. Research of the effects of mental health in human models has now launched. This creates the possibility of treating depression and anxiety by changing people's microbiome in the future. Further research needs to be done in order to understand the mechanisms of how our microbiome affects our health and studying the microbiome of healthy populations too. For now, eat your probiotics and stay away from sugar and processed foods to diversify your microbiome for better mental health.
Writer: Lauren Renehan
Editor: Nathaniel Meshberg
Sources:
https://www.genengnews.com/news/depression-and-gut-bacteria-link-strengthened/ https://neurosciencenews.com/depression-gut-bacteria-10685/ https://www.iflscience.com/plants-and-animals/link- found-between-gut-bacteria-and-depression/ https://www.bmj.com/content/361/bmj.k2179
Less Sleep, Less Friends

Interestingly enough, in today’s society, it seems like depriving oneself of sleep is almost like a trophy to jokingly brag as people attempt to see who slept the least number of hours yesterday or who pulled the most number of all-nighters last week. In addition, with finals season approaching, it becomes tempting for most students to sacrifice their sleep to score a few more points on the exam, although one can’t help but to ask if it was really worth it. Sleep deprivation seems like a necessary part of life that many college students must go through to succeed academically. There is even a joke that college students can only choose two of the following: good grades, social life and enough sleep. However, one of the choices, social life, seems unlikely as a sustained pattern of sleep deprivation can have an impact on the social aspect of our lives.
A study conducted in UC Berkley showed that people who suffer from sleep deprivation tend to become recluse; instead of seeking protection from society, sleep deprived individuals withdraw from social situation in the hopes of obtaining rest. In this experiment, they showed participants a stranger with a neutral facial expression walking towards them, and they asked them to hit the panic button when they felt that the stranger was getting too close. They found that sleep deprived participants hit the button significantly earlier than those who did get sleep. Through fMRI scans, they tried to see what regions of the brain were responsible for this behavior. One region, called the near space network, was very active compared to the control group. This region allows one to orient oneself in space and get out of threatening situations that involve spatial elements. In addition, the theory of mind network, which allows people to interpret others’ intention, was less active in sleep deprived participants than the control group. Thus, sleep deprivation may lead to a more antisocial attitude and an inability to fully detect social cues.
Yet another study also shows increased anxiety and fear levels in people who suffer from sleep deprivation. Sleep deprivation can increase sensitivity in the amygdala, leading to stronger fear responses to a stimulus. As a result of the activation of the amygdala, the ventromedial prefrontal cortex (vmPFC) begins to regulate emotion and inhibit activity in the amygdala. Another area of the brain, the insula, does the opposite of vmPFC and increases the activity in amygdala which then leads to fear acquisition. In a study by Feng et al. (2017), participants’ brains were tracked with an fMRI while they were shown series of different shapes in which a certain consecutive pattern of shapes would indicate an electric shock. In sleep deprived participants, higher activity was seen in the connections between the amygdala and the insula, while for the control group a higher activity was seen between amygdala and vmPFC.
When comparing the results of the two studies, both makes sense; sleep deprived individuals have increased levels of anxiety and fear which could have led to earlier responses in pushing the panic button. Both studies also demonstrate that the lack of sleep can affect one’s mood and thus their ability to socially interact with others. Although it is difficult for college students to find time to get quality sleep, getting sleep can possibly improve the social aspects of one’s life.
Writer: Audrey Kim
Editor: Lauren Renehan
Sources:
https://www.inverse.com/article/48046-sleep-deprivation-leads-to-social-isolation-in-new-study https://psychcentral.com/blog/how-being-sleep-deprived-alters-a-brain-connection-that-causesfear-and-anxiety/
Deep Brain Stimulation
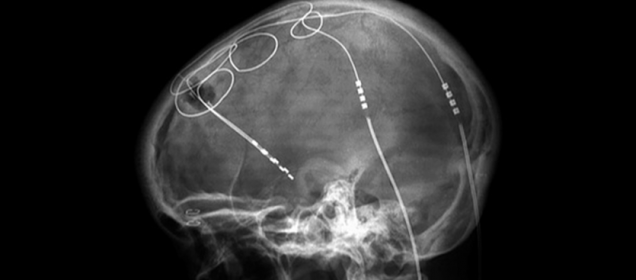
Over the past two decades, a neurosurgical technique known as Deep Brain Stimulation (DBS) has revolutionized the fields of both medicine and neuroscience. DBS has been able to accomplish incredible feats once deemed impossible, one of these being the extremely effective treatment of Parkinson’s Disease symptoms. DBS has also opened many doors to a bright future where debilitating neurological disorders and diseases may be eradicated.
So what exactly is Deep Brain Stimulation? Deep Brain Stimulation essentially consists of sending electrical impulses to certain brain areas via surgically implanted electrodes, resulting in the removal of adverse neurological symptoms. The exact mechanism by which DBS exerts its effect on neurons is still not fully understood, although many theories have been presented. One popular explanation for the mechanism behind DBS is that electrode stimulation of certain brain areas induces changes in neuronal activity in the respective neural circuits that would ultimately change physiological and cognitive behavior.
An example of DBS in action can be seen through one of its most common applications, Parkinson’s Disease treatment. Parkinson’s Disease is characterized by voluntary motor deficits and symptoms including resting tremor, bradykinesia, postural instability, extreme difficulty initiating voluntary movement, and more. These symptoms are caused by the loss of dopamine producing neurons in an area called the substantia nigra, which is a constituent of a much more complex brain circuit within the basal ganglia that controls the initiation of voluntary movement. Needless to say, this neurodegenerative disease is very debilitating for the patient. When medications such as L-DOPA fail to alleviate Parkinson’s Disease symptoms, DBS steps in to save the day. Electrodes are surgically inserted into brain areas such as the internal Globus Pallidus or the Subthalamic Nucleus and are connected to an internal pulse generator (IPG) located in the patient’s chest or abdominal cavity. Upon the initiation of electrical impulses to those certain brain areas via the implanted electrodes, the patient’s symptoms disappear immediately and the patient is able to execute normal voluntary motor function without difficulty.
DBS holds vast potential and unending applications in the fields of medicine and neuroscience. DBS research is currently being done to investigate its effect in treating a plethora of neurological disorders including major depressive disorder, OCD, PTSD, addictions, Alzheimer’s Disease dementia, chronic pain, schizophrenia, eating disorders, and more. As mentioned, DBS has opened the doors to a new and hopeful future in which neuroscience research and medicine can eradicate the most debilitating of neurological disorders. Ironically, although DBS was created to provide an answer to the many questions plaguing neuroscientists and doctors today, it has instead prompted us to ask infinitely more questions and has further shown how little we know about our own brains. I will end our short discussion of Deep Brain Stimulation with a quote by Santiago Ramon y Cajal, the father of modern neuroscience himself, which sums up what DBS, and neuroscience itself, is all about: “To know the brain...is equivalent to ascertaining the material course of thought and will, to discovering the intimate history of life in its perpetual duel with external forces.”
Writer: Richard Kuang
Editor: Audrey Kim
Sources:
https://www.sciencedaily.com/
https://www.ncbi.nlm.nih.gov/
Klotho and the Aging Brain

Why does the brain deteriorate with age? Researchers might finally have found a potential cause. The klotho protein has been found to be associated with the aging brain. Specifically, higher levels of klotho have been associated with longevity of the brain. As you grow older, however, your brain’s klotho levels decrease, and researchers believe that this decrease may be related to age-related impairments.
Experiments conducted at the Gladstone Institute of Neurological Disease measuring klotho levels in mice show decreasing levels of klotho with age in the choroid plexus, a brain structure whose cells are responsible for producing cerebrospinal fluid and forming a barrier between the central nervous system and the bloodstream. In addition, experimentally reduced klotho levels in mice resulted in increased inflammation in the brain. The researchers thus found that klotho plays a role in maintaining the integrity of the blood brain barrier – a gatekeeper for protecting the brain from the peripheral immune system. This observation is particularly important because brain inflammation is a prominent feature of neurodegenerative diseases such as Alzheimer’s disease and multiple sclerosis.
Klotho has also been shown to be therapeutic and saves cognitive functions such as spatial learning and memory that were impaired as a result of aging or dementias. Researchers at UCSF injected a small fragment of the klotho protein into 18-month-old mice (about the same stage in the mouse lifespan as a 65-year-old human). What they observed was that a single injection of klotho significantly improved the ability of the mice to navigate and learn new tasks. The researchers then injected the protein into mice that were engineered to produce abundant levels of alpha-synuclein in order to induce Parkinson’s disease-like symptoms, namely movement disturbances. As a result of klotho administration, these mice displayed improvement in motor function as well as improvement in learning to navigate and explore new territories. All of these improvements were shown in spite of the mice brains still containing the toxic alpha-synuclein, indicating that the klotho protein appears to play a protective role against toxicity in the brain.
So, given this potential protective role for klotho, a next step for researchers could possibly be to develop a potential klotho-related treatment for individuals suffering from neurodegenerative diseases.
Writer: Nathaniel Meshberg
Editor: Audrey Kim
Sources:
https://neurosciencenews.com/aging-brain-10179/
https://www.sciencedaily.com/releases/2017/08/170808150006.htm
BU Study Finds First Evidence of Genetic Link to CTE

A new study out of the Boston University School of Medicine shows the first evidence of a genetic link to developing chronic traumatic encephalopathy (CTE). CTE is a neurodegenerative disease that may be diagnosed in patients with repeated head trauma. These patients typically exhibit cognitive and emotional issues including difficulty planning, emotional instability, substance abuse, impulsivity, and short-term memory loss. However, CTE can only be diagnosed postmortem, and there is currently no reliable way to predict who will develop this disorder.
This study, published in Acta Neuropathologica, is the first to show that there may be a genetic predisposition to developing CTE. Eighty-six brain samples from deceased American football players were examined for the presence of a missense mutation (rs3173615) in the TMEM106B gene. These players had all been diagnosed with CTE after their deaths. The mutation has been identified as playing a role in neuroinflammation and TDP-43 neurodegenerative diseases (such as ALS and Alzheimer’s). Thus, this specific mutation was of interest to researchers, who have been trying to find a possible genetic basis for the development of CTE.
Researchers identified that those diagnosed with CTE were more likely to have the missense mutation (rs3173615) on the TMEM106B gene than those without the disease. They also found that those with this gene variant were 2.5 more likely to have developed dementia. Researchers found that the presence of rs3173615 was associated with synaptic loss, dementia, and density of abnormal tau protein. However, these results were only seen when analyzing the brains of those diagnosed with CTE.
When compared to case-controls, the same associations were not observed. This study is the first to identify a possible genetic link to the development of CTE. The actual applicability of this study is limited, but it does provide possible paths for future research into the causes of CTE. There are likely to be many genes that contribute to the development of CTE, and as such, further research is needed. It is possible that this research could lead to preventative measures, diagnostic methods, and treatment of CTE; all of which are extremely limited as of now. CTE has been a popular topic in the news recently, with evidence accumulating that links head trauma from contact sports to CTE-like symptoms. A Boston University study in 2017 found that 99% of former NFL players’ brains that were studied showed signs of CTE. Evidence has also been produced to show that playing contact sports as a minor may contribute to cognitive deficits later in life. Studies like these have led to some arguing that contact sports (especially football) need to be altered to mitigate the risk of head trauma. Such alterations may include better helmets or rule changes. Some have even argued that children should not play football because of the risk of future brain trauma may be too great. More studies like this one are needed to assess the validity of these arguments, but in the meantime, these studies have ignited the debate around contact sports.
Writer: Jayden Font
Editor: Lauren Renehan
Sources:
https://www.bostonglobe.com/metro/2018/11/03/study-hints-that-certain-gene-may-worsen-cte/ QORz6GjMsKCjqGvAOBblxN/story.html https://actaneurocomms.biomedcentral.com/articles/10.1186/s40478-018-0619-9 https://www.mayoclinic.org/diseases-conditions/chronic-traumatic-encephalopathy/symptoms-ca uses/syc-20370921 https://www.cell.com/trends/molecular-medicine/pdf/S1471-4914(08)00186-X.pdf http://www.bu.edu/cte/2017/07/25/bu-researchers-find-cte-in-99-of-former-nfl-players-studied/ http://www.bu.edu/cte/2017/09/19/study-suggests-link-between-youth-football-and-later-life-emo tional-behavioral-and-cognitive-impairments/
A Value in Old-Fashioned Memorization

With a computer or telephone in hand, it seems pointless to memorize simple facts, lists of things, poems, directions, dates or formulas. From an evolutionary standpoint before modern day technology, people would constantly have to exercise their mind and memorize what we currently leave the task for our computer or telephone in hand to remember. But schools are now switching their structures to provide students the skills to apply knowledge instead of reciting information, which seems logical. Except there may be a huge positive to memorizing what seems to be pointless information.
Memorizing information is the equivalent to lifting weights in the gym, but instead of building more muscle, the levels of acetylcholine increase in the brain. Acetylcholine is a neurotransmitter has been identified by scientists to keep the mind sharp; it is critical in creating and strengthening connections between neurons. People blame the lack in memory as a consequence of aging, but scientists are finding out it has more to do with how much the person is exercising the mind. More specifically, the brain produces acetylcholine when the person is exercising the mind, such as when a person is trying to pay attention1. Although many people's memories increasingly start to fail after their mid-40’s, elderly people who constantly exercise their minds show high levels of acetylcholine, and their memory, as a result, does not deteriorate as rapidly. High levels of acetylcholine also reduce the risk of dementia; for example, cholinesterase inhibitors, which inhibit proteins that degrade acetylcholine and consequently lead to higher acetylcholine levels, have been used to slow down the effects of Alzheimer’s1.
In response to this trend of memory loss, researchers in New York discovered five compounds that naturally reinstate optimal levels of acetylcholine: Alpha GPC, Huperzine A, Bacopa Monnieri, Lion's Mane Mushroom, and Ginkgo Biloba2. This formula was named RediMind. RediMind was created in order for people to use modern day technology without the consequence of drastically losing their memory through aging. After a placebo-controlled clinical trial by Princeton Consumer Reseach, the results showed that the group who took the RediMind drug had scored 45% better than the placebo group2. Another positive of RediMind is that it gives the brain a long-term boost for energy compared to short-term boosts of drugs like caffeine.
RediMind is now for sale but has not been reviewed by the FDA. This could one step closer to creating enhancers for superpower memorization, but this drug has not been tested enough to prove consistent improvement of memory and to be safe for the brain. So, for now, I would stick to memorizing directions, grocery lists, and more vocabulary words to work out my brain.
Writer: Lauren Renehan
Editor: Audrey Kim
Source:
- https://globenewswire.com/news-release/2018/07/24/1541146/0/en/Alzheimer-s-related-Study-B rain-Training-Upregulates-Acetylcholine.html
- https://www.nutreance.com/articles/redimind?utm_medium=google_display&utm_campaign=redimind_us_content&utm_source=neurosciencenews.com&utm_term=long%20term%20memory &gclid=EAIaIQobChMIg8z664a33gIVAhLTCh3CIg5VEAEYASAAEgJz_vD_BwE
The Role of Music in Neurodegeneration: How it Can Help
Music is all around us. It’s in our ears as we walk to class with our earbuds in. It’s in the cars we drive and the ubers we take. It’s in malls and grocery stores. It’s even infiltrated the smallest of spaces, like elevators in hotel lobbies. This ubiquity of music may make it lose its significance in our eyes, however, this is not the case for people suffering from neurogenerative diseases such as Alzheimer’s and Parkinson’s. Music plays an important role in the lives of these people. While they may find themselves lost in their own minds, music can help guide them to lucidity, even for a little bit. Clinicians and researchers are utilizing music therapy as a supplemental treatment for people who suffer from neurodegenerative diseases. This approach has been found to be extraordinarily beneficial in such patients. In fact, in his book Musicophilia, Oliver Sacks writes: “ music therapy with such patients is possible because musical perception, musical sensibility, musical emotion, and musical memory can survive long after other forms of memory have disappeared. Music of the right kind can serve to orient and anchor a patient when almost nothing else can.”1
One of the most prevalent neurodegenerative diseases is Alzheimer’s disease with 5.7 million Americans suffering from it in 20182. So far there is no absolute ‘cure’ for AD. It is caused by an accumulation of p-tau and neurofilaments in the brain which cause cell death and neurodegeneration in the hippocampus. Music therapy has been found to be an effective non-pharmacological approach to manage AD. A study by Arroyo-Anlló EM et al was conducted on self-consciousness in people suffering from mild to moderate AD where they played familiar music for one group of people and unfamiliar music for another group. They found that familiar music intervention resulted in improvement in some aspects of self-consciousness such as personal identity, affective state, moral judgements and body representation. The researchers suggested that the improvement in self-consciousness may be due to the enhancement of general cognitive state by familiar music3.
Another study investigated the effects of background music on autobiographical memory of those with mild AD and also found encouraging results. The investigators conducted Autobiographical Memory Interviews (AMI) in which they asked questions related to major events in the individual’s lives that spanned over childhood, early adulthood and recent life. They found that subjects that had music ‘Spring’ movement from Vivaldi’s ‘Four Seasons’ in the background during the interview had higher AMI recall scores especially for recent personal semantic memories. Subjects in the music condition had reduced state anxiety levels and therefore the researchers attribute the enhanced autobiographical recall to an anxiety reduction mechanism brought on by music4.
Music seems to have interesting effects on people who suffer from Parkinson’s disease as well. Parkinson’s is the second most common neurodegenerative disorder with approximately 60,000 Americans diagnosed with it every year5. It usually caused by cell death in the substantia nigra in the basal ganglia. This causes a depletion of dopamine in the brain which is responsible for the symptoms present in Parkinson’s such as gait abnormalities. Oliver Sacks makes another interesting observation in his book where he states, “The patient can regain a fluent flow with music, but once the music stops, so too does the flow. There can, however be longer-term effects of music for people with dementia – improvements of mood, behavior, even cognitive function – which can persist for hours or days after they have been set off by music.”6 Researchers have found some encouraging results in line with Sack’s conclusion. In a study conducted by Benoit et al, it was found that musically cued gait training showed improvement in gait, motor timing, and perceptual timing. They trained patients with Parkinson’s to walk to the beats of German folk music on their own but giving them exact instructions on how to do so. They found that not only did these patients show improvements in gait velocity and stride length, but this effect outlasted the duration of the training for up to one month7.
In the same study, they also found that music therapy has the ability to enhance perceptual timing. They assessed this using a tone duration detection task and found that the patients that had undergone musical intervention improved their performance in these tasks. The researchers state that both these effects may be attributed to a cerebello-thalamo-cortical tract which is activated by auditory cues and compensates for the dysfunction in the basal ganglia as the enhancement in perceptual timing is responsible for the improvements in the subjects’ gait 8.
While we may take music for granted, it can play a very important part in people’s lives – particularly those that have to live with neurodegenerative disorders like Alzheimer’s and Parkinson’s. Unfortunately, there’s no exact ‘cure’ for these diseases, but interventions such as music therapy can still help provide a unique approach to alleviate many of the debilitating symptoms presented by these disorders.
Writer: Farwa Faheem
Editor: Kawtar Bennani
Sources:
- Musicophilia by Oliver Sacks
- https://www.alz.org/media/HomeOffice/Facts%20and%20Figures/facts-and-figures.pdf
- https://www.hindawi.com/journals/bmri/2013/752965/
- https://search-proquest-com.ezproxy.bu.edu/docview/232495436?accountid=9676&rfr_id=info%3Axri%2Fsid%3Aprimo
- https://parkinsonsdisease.net/basics/statistics/
- https://www.frontiersin.org/articles/10.3389/fnhum.2014.00494/full
Unique Folding Patterns in Autism Brains

Recent studies have shown that the brains of children with Autism Spectrum Disorder (ASD) fold differently than a normal brain—either being unusually smoother or unusually convoluted depending on location and age. Researchers measure the development of neural tissue folds in the cortex as changes in the local gyrification index; a ratio which compares the area of the smooth outer surface with that of the inside the sulci. Using this information, researchers can understand the link between autism and the folds of a brain.
In a study at San Diego State University, it was found that school-age children and adolescents with autism had more intricately folded regions. The left temporal and parietal lobes, which are responsible for processing sound and spatial information, were shown to have these intricate folds in children with autism. Research also found increased gyrification in the right temporal and frontal lobes, which are responsible for decision making and motor skills. In contrast, a second study found that preschoolers with autism do not show this degree of intricate folding unless they had enlarged brains. Preschoolers with autism were also found to have an unusually smooth region in the occipital lobe (specifically in the region dedicated to recognizing faces). These studies, in juxtaposition, demonstrate that brain folding hints at the different developmental path that autism brains follow when compared to normal brains. According to Ruth Carper, a researcher at San Diego State, “many of the brain areas with exaggerated folding are among the earliest to develop folds during gestation.” Thus, the folding will increase in intricacy and convolution over time due to this developmental disruption. In another study at the University of California, Davis, researchers found that children with enlarged brains actually have a specific subtype of autism due to the fact that only children with enlarged brains exhibited this degree of increased and atypical folding. This study adds to the evidence that folding patterns depends on the development of the individual and where that individual lies within the autism spectrum.
It’s clear that ASD is a very complex subset of conditions and traits that are influenced by various genetic and environmental factors. A great deal of research is focused on identifying physical differences, such as brain folding patterns, which are present in the autistic brain. In doing so, resources may be found to aid and benefit a developing brain with ASD. Lastly, such research will only further our understanding of how all of our brains grow and evolve over time.
Writer: Ava Genovese
Editor: Farwa Faheem
Sources: