Home
PTSD/Depression
It's imperative to highlight the often overlooked struggles of individuals facing conditions like PTSD and depression in the realm of mental health. These challenges bring unique and profound experiences that require empathy and support. Understanding the impact of conditions such as Post-Traumatic Stress Disorder (PTSD), stemming from traumatic events and characterized by distressing symptoms like flashbacks and anxiety, is crucial. Creating safe environments, recognizing signs of distress, and providing support are essential in aiding those on the path to healing. Depression, a prevalent mental health issue affecting millions globally, necessitates breaking the silence, fostering open dialogue, and reducing stigma for effective support. Connecting individuals with appropriate mental health resources contributes to creating a world that prioritizes and supports the mental well-being of all its members.
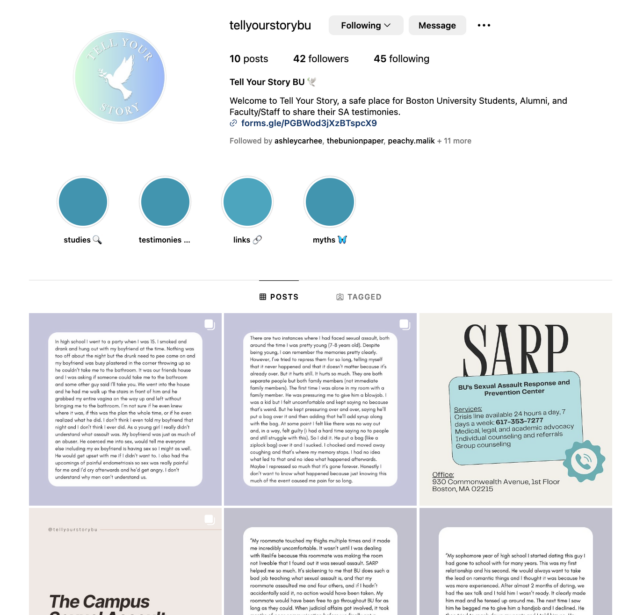
Tell Your Story: A Support Hub for Victim-Survivors and Community Members at Boston University
Instagram: https://www.instagram.com/tellyourstorybu/
@TellYourStoryBU, established in October 2023, was born out of a dedication to providing a secure space for victim-survivors to share their experiences with sexual assault, harassment, and any other impactful incidents. My vision was to create a space accessible to students regardless of when, where, or by whom their experiences occurred. The primary focus remained on the victim-survivor's well-being; I wanted an anonymous resource on campus where individuals could express themselves without pressure. These goals soon developed beyond support for victim-survivors, extending to encompass a more comprehensive approach. I wanted to offer resources, educational content, and information tailored to anyone within the Boston University community. This initiative sought to be a hub where students, faculty, staff members, and more could find valuable information on all aspects of sexual violence.
I grew up in the United Kingdom, and my inspiration for this project stemmed from Soma Sara's creation of an anonymous submission site named 'Everyone’s Invited' in June 2020. What began as a platform for testimonies has since grown into an invaluable resource, including not only testimonies but also a wealth of resources for individuals dealing with sexual assault and harassment. As a survivor who found empowerment in similar resources, I founded @TellYourStoryBU to offer that same supportive space to others.
The research process for this account is ongoing and likely to continue indefinitely. Each time I receive a new testimony, I am prompted to read, reflect, and research specific topics related to the shared experience. This allows me to curate resources and links, support hotlines, and more for the individual sharing their story and others who may have undergone similar experiences. Moreover, I aim to eventually use the information collected on sexuality, race, gender, age, and more to provide pertinent insights to SARP and BU SHS. The goal being to facilitate culturally competent and tailored support for all students.
As with anything surrounding this type of topic, there are obviously challenges that I am presented with. One of these challenges is frustration; I find myself becoming frustrated that I am not doing enough, that I could be doing more, and that the work I am trying to do will not be enough until every single individual is being helped. However, when I gave my presentation in my final MET CJ 512 class with Dr. Rousseau, a student reminded me not to try to place stress on the number of people I had helped. Instead to acknowledge that I have been able to provide a resource that is enough for someone, regardless of the number of individuals submitting testimonies or engaging with the account.
Looking ahead, there is ample room for growth and innovation. I aspire to continue creating informative infographics and providing resources through the account. With 42 followers gained and 214 accounts reached in the last two months, I hope the numbers continue to grow, reaching every corner of the Boston University community. Even if only one person finds the needed support or information, I would be content. @TellYourStoryBU has become a personal passion project, and I hope it becomes a valuable resource for individuals.
Finally, I would like to express my heartfelt gratitude to Dr. Rousseau for her unwavering support throughout the semester. Her expertise, exceptional teaching approach, and dedication to every student in our class empowered me to undertake this initiative. It is primarily thanks to her that @TellYourStoryBU exists as a resource for the Boston University community.
The Effect of Trauma on the Brain
The experience of trauma is a complex and arduous challenge that can have long-lasting consequences for individuals. Recent research has uncovered that trauma can significantly modify both the physical structure and function of the brain. These alterations can manifest in changes to critical brain regions, the prefrontal cortex, amygdala, and hippocampus, all of which play essential roles in regulating behavior, emotion, and memory.
The amygdala, a nucleus located in the posterior region of the brain, plays a pivotal role in the processing of feelings, particularly fear and anxiety. Traumatic events often trigger heightened activation of this structure. Consequently, individuals who have been exposed to such traumatic events may present significant emotions such as anxiety or fearful reactions in situations that would not typically elicit such a response. The amygdala functions as the brain's alarm system and, when activated, triggers the fight-or-flight response, which is also known as the fight-flight or freeze mode (Rousseau, 2023). As a result, individuals may otherwise be started and suddenly experience anxiety or fear in situations where these emotions would not typically arise (Rousseau, 2023).
The hippocampus, an integral component of the brain, plays a pivotal task in configuring and retrieving memories. However, traumatic events can lead to this region's shrinking, resulting in memory recall difficulties. Such challenges can impede individuals' ability to remember essential details or events, which can exacerbate feelings of anxiety and stress. The hippocampus is responsible for the development of new connections between neurons and storing memories, and it has a role in regulating stress hormones. Any damage to this brain area can lead to a decrease in the ability to form new memories and can cause higher levels of stress hormones that, in turn, interfere with memory recall (Rousseau, 2023).
The prefrontal cortex is another fundamental region of the brain and is in control of regulating emotions, decision-making, and behavior. When an individual experiences trauma, it can cause a notable reduction in activity within this area of the brain. As a result, individuals who have undergone trauma may experience difficulties with impulse control, decision-making, and emotional regulation. Additionally, they may display a propensity for engaging in risky behavior, exhibiting intense mood swings, and developing addiction issues (Rousseau, 2023).
It is essential to recognize the impact that emotional trauma can have on cognitive functioning and behavior, particularly within vulnerable populations. By understanding the relationship between trauma and the prefrontal cortex's functioning, healthcare providers and mental health professionals can develop more effective interventions and treatment plans (Dr. T Barthelemy).
Acknowledging that changes may manifest in the brain even without physical injury is imperative. Traumatic emotional events may result in the rewiring of the brain, thereby impacting our perceptions of the world, relationships with others, and a person’s decision-making abilities (Dr. T Barthelemy). This rewiring is enabled by neuroplasticity, which is the brain's capacity to restructure itself in response to new experiences. Consequently, our modes of thinking, feeling, and responding to the world may undergo alterations. Trauma may also pave the way for the development of mental health behavioral systems such as anxiety, depression, and PTSD. All of which may exacerbate the challenges confronting individuals who have undergone trauma (UR Medicine).
Extensive research has been conducted recently on how individuals who have experienced trauma can distinguish between safe and unsafe situations. The study published in Communications Biology highlights the impact of trauma on the salience network, a critical part of the brain responsible for learning and survival. The research found that people who have experienced trauma, whether they have psychological disorders including depression, anxiety, or PTSD, have different functioning of the salience network in their brains. This research is crucial by helping these individuals manage their feelings and cope with the traumatic experiences. By recognizing the difference between what is safe and what is dangerous, victims of trauma can take proper actions to protect themselves from further harm and develop healthier coping mechanisms to deal with their trauma (UR Medicine).
Dr. Suarez-Jimenez, a postdoctoral fellow at Columbia University Irving Medical Center, conducted a study to gain insight into how exposure to trauma affects emotions and the brain. The study involved measuring the brain activity of trauma victims using functional magnetic resonance imaging (fMRI) while they were exposed to emotional stimuli. To gain a more in-depth understanding of how trauma affects the brain, he contrasted the brain activity of trauma victims with that of non-trauma victims. As part of his research, he examined the biological mechanisms that affect trauma survivors to gain a greater understanding of how their brains respond to trauma and how their emotional regulation is affected (UR Medicine).
Dr. Suarez-Jimenez's research shows significant importance in supporting individuals who have experienced trauma by facilitating the development of healthier coping mechanisms for their emotions. Through careful examination of the biological mechanisms of trauma, this study aimed to provide valuable insights into how different brain regions respond to such experiences and how these reactions can impact one's emotional regulation. Such insights are critical in formulating effective treatment strategies that can aid trauma victims in managing their emotions and promoting a healthy recovery (UR Medicine).
In a study, individuals were subjected to circles of varying sizes, while their brain activity was observed using functional magnetic resonance imaging (fMRI). Only one side of the circle was associated with a minor shock. The researchers discovered that individuals exposed to trauma without psychopathologies compensated for the changes by engaging the executive control network, one of the brain's most prominent networks. The study also found that individuals exposed to trauma but resilient to its adverse effects had another difference in the salience network. They compensated for these changes by engaging the executive control network, which helped them maintain cognitive flexibility and adaptability, two crucial skills for coping with stress and trauma (UR Medicine).
This insightful study illuminates how the brain reacts to trauma and underscores the importance of the salience network in areas such as learning, survival, and resilience. It offers a deeper comprehension of the complicated nature of trauma and its impact on individuals. The research yields an invaluable understanding of the mechanisms by which trauma affects the brain and emotions, which can lead to more effective treatment methods and improved outcomes for those who have undergone traumatic experiences (UR Medicine).
References
Bartelemy, T. (n.d.). Mental Health. (12.05.2023.)
Rousseau, D. (2023). Module 5: Trauma, Genocide, and the Holocaust. Boston University.
Your home for world-class care. University of Rochester Medical Center | UR Medicine. (n.d.). http://www.urmc.rochester.edu/
Animal-Assisted Intervention and Trauma
There are several different therapeutic approaches available to trauma victims. One of which is called animal-assisted intervention (AAI). AAI is defined as “the utilization of various species of animals in diverse manners beneficial to humans” (American Veterinary Medical Association, 2023). The most common form of this approach seen in everyday life is through the use of service dogs. Psychiatric service dogs are specially trained to assist their handlers in the areas where assistance is needed, especially if the handler is incapacitated (Rousseau, 2023). However, service dogs go far beyond providing physical assistance. They also provide mental and emotional assistance as well. Studies prove that the use of AAI has proved to be beneficial in a number of populations such as trauma victims suffering from post-traumatic stress disorder (PTSD), individuals with dementia and children diagnosed with autism spectrum disorder (O'Haire, et al., 2015).
In regards to individuals suffering from PTSD, researchers found that emotional numbness and isolation are common symptoms. AAI has proven to be beneficial to individuals with PTSD because the presence of an animal such as a dog encourages positive emotions and warmth (O'Haire, et al., 2015). Further, animals have been demonstrated to be social facilitators, which connect and unite people thus reducing loneliness and ultimately isolation (O'Haire, et al., 2015). Animals also require routine care, which can mean daily walks, a trip to the store for food, and bathroom breaks. All of which encourages an individual with PTSD to get out of the house and socialize with the world.
As such, animal-assisted intervention is an effective therapeutic approach worth considering for trauma victims.
References
American Veterinary Medical Association. (2023). Animal-assisted interventions: Guidelines. American Veterinary Medical Association. https://www.avma.org/resources-tools/animal-health-and-welfare/service-emotional-support-and-therapy-animals/animal-assisted-interventions-guidelines#:~:text=Animal%2Dassisted%20intervention%20(AAI),types%20of%20animal%2Dassisted%20intervention.
O'Haire, M. E., Guérin, N. A., & Kirkham, A. C. (2015). Animal-Assisted Intervention for trauma: a systematic literature review. Frontiers in psychology, 6, 1121. https://doi.org/10.3389/fpsyg.2015.01121
Rousseau, D. 2023. Module 4: Pathways to Recovery: Understanding approaches to trauma treatment. Boston University.
The Adverse Childhood Experience (ACE) Study
The Adverse Childhood Experience (ACE) was the biggest study of its kind ever created (Rousseau, 2023). In 1958, Dr. Vincent Felitti and his colleague Dr. Robert Anda of Kaiser Permenente studied more than 50,000 patients, finding clear characteristics or commonalities (Rousseau, 2023). It is highlighted that the most damaging statistic found is how the trauma could later manifest into adults (Rousseau, 2023). Furthermore, as the number of ACE categories higher, the number of conditions also increases (Rousseau, 2023). When there is exposure to one category, there is an 80% likelihood of exposure to another category (Rousseau, 2023). These ACE categories include, alcoholism and alcohol abuse, chronic obstructive pulmonary disease, depression, drug use, heart and liver disease, risk of partner violence, smoking, suicide, and overall decline in quality of life (Rousseau, 2023).
Expanding more about the ACE study, Felitti and Anda spent more than a year creating ten new questions that involved defined categories of adverse childhood experiences which included, physical and sexual abuse, physical and emotional neglect, and family dysfunction like having parents who were divorced, mentally ill, addicted, or in prison (van der Kolk, 2014). Ultimately, the ACE study showed that traumatic life experiences during childhood and adolescence are a lot more common than previously expected (van der Kolk, 2014). It is stated that the study respondents were mainly White, middle class, middle aged, well educated, and financially secure enough to have good medical insurance, highlighting that only one-third of the respondents stated no adverse childhood experiences (van der Kolk, 2014). Additionally, the study revealed that the effects of trauma permeated these patients’ adult lives (van der Kolk, 2014). An example mentioned is that high ACE scores turned out to correlate with higher workplace absenteeism, financial issues, and less lifetime income (van der Kolk, 2014).
Furthermore, Felitti and his team discovered that adverse experiences are interrelated, even though they are usually studied individually (van der Kolk, 2014). For example, people do not usually grow up in a household where one brother is in prison, but everything else is okay (van der Kolk, 2014). Incidents of abuse are never ‘standalone’ events, and for each additional adverse experience reported, the toll in later damages rises (van der Kolk, 2014). Felittti and his team also discovered that the impact of childhood trauma initially became noticeable in school (van der Kolk, 2014). Referring to the ACE study results, more than half of those with ACE scores of four or higher reported having learning or behavioral issues, which was compared with three percent of individuals with a score of zero (van der Kolk, 2014). It is expressed that as the children matured, they did not ‘outgrow’ the impact of their early experiences (van der Kolk, 2014). Felitti highlights, ‘“Traumatic experiences are often lost in time and concealed by shame, secrecy, and social taboo”’ (van der Kolk, 2014). However, the ACE study revealed how the effects of trauma permeated these patients’ adult lives (van der Kolk, 2014).
Moreover, after Robert Anda presented the results of the ACE study, he realized that they had found the gravest and most expensive public health issue in the United States, which is child abuse (van der Kolk, 2014). Anda’s calculations entailed that the overall costs surpassed those of cancer or heart disease (van der Kolk, 2014). In addition, eliminating child abuse in America would lessen the overall rate of depression by more than half, alcoholism by two-thirds, and suicide, IV drug use, and domestic violence by three-quarters (van der Kolk, 2014). Eradicating child abuse in America would also have a huge impact on workplace performance, and greatly lessen the need for incarceration (van der Kolk, 2014). Furthermore, follow up studies and papers are still showing up around the world regarding the ACE study. However, the day to day reality of those who suffered child abuse, as well as children in outpatient clinics and residential treatment centers around the country remains the same (van der Kolk, 2014). The only difference now, is that they receive high doses of psychotropic agents, which makes them more manageable, but will also affect their ability to feel pleasure and curiosity, to grow and develop emotionally and intellectually, and to ultimately become contributing members of society (van der Kolk, 2014).
Expanding more on psychotropic agents, the reason why taking medications could be effective, is because it could be used to lessen extreme or debilitating symptoms as an initial step in trauma recovery (Rousseau, 2023). A few of the symptoms that could be lessened with medication include, sleep disorders, hyperarousal, emotional reactivity, depression, and intrusive or recurring thoughts and images (Rousseau, 2023). However, it is highlighted that an approach that may work for one person, may not work for another, potentially even increasing the other person’s experience of trauma symptoms (Rousseau, 2023). Nonetheless, pharmacotherapy, or the use of medication, is one approach to addressing the impact of trauma, specifically in situations where people will experience symptoms like anxiety, depression, or other mental health problems associated with traumatic experiences. Pharmacotherapy would be a very effective approach, especially in tandem with other therapeutic approaches, like psychotherapy in order to provide a comprehensive treatment plan (Alcohol and Drug Foundation, 2021).
Elaborating more on pharmacotherapy, from a neurology perspective, there are many different neurotransmitters in one’s brain (Rousseau, 2023). All in all, pharmacotherapy works by manipulating neurons and neurotransmitters to gain the desired effect (Rousseau, 2023). In addition, medications can be effective in reducing specific symptoms associated with trauma such as, intrusive thoughts, nightmares, or panic attacks. Furthermore, medicines that target the autonomic nervous system, like propranolol or clonidine, could help in lessening hyperarousal and reactivity to stress (van der Kolk, 2014). This group of drugs works by blocking the physical effectiveness of adrenaline and the fuel of arousal, therefore lessening nightmares, insomnia, and reactivity to trauma triggers (van der Kolk, 2014). Additionally, blocking adrenaline can help to keep the rational brain online and make choices possible (van der Kolk, 2014). Ultimately, a detailed approach by a mental health professional is crucial to identify the most appropriate treatment approach, whether it involves medication, psychotherapy, or a combination of both.
Lastly, referring back to the importance of the ACE study, the implementation of this research could be very beneficial if integrated in one’s workplace. For example, providing training among professionals to recognize and respond to people affected by adverse childhood experiences. This could provide more awareness into one’s potential trauma history, guiding more efficient and sensitive methods. Another implementation could be developing support systems that consider the findings of the ACE study in order to help those affected by childhood trauma. Overall, the goal is to use the ACE study’s findings to apply more informed, understanding, and efficient approaches when dealing with people who have experienced childhood traumatic events.
Resources:
Australian Drug Foundation. (2021). Pharmacotherapy for young people. Alcohol and Drug Foundation. https://adf.org.au/talking-about-drugs/seeking-help/pharmacotherapy-young-people/what-is-pharmacotherapy/#:~:text=Pharmacotherapy%20is%20the%20treatment%20of,with%20a%20legally%20prescribed%20substitute.
Rousseau, D. (2023). BU Learn. Retrieved from https://learn.bu.edu/bbcswebdav/pid-12438217-dt-content-rid-91014393_1/courses/23fallmetcj720_o2/course/module1/allpages.htm
Van, K. B. A. (2014). The body keeps the score: Brain, mind, and body in the healing of trauma.
Existential Crisis Online: Where is the Trauma Hidden?
Contemporary literature defines racism and ethnoviolence as one of the main catalysts for causing traumas in individuals, where racism is a system of oppression based on racial categories and domination considering one group to be superior while the others inferior, and ethnoviolence is violence and intimidation of members of particular ethnic groups who are stigmatized by the dominant culture to maintain their status in society (Helms & Nicolas, 2010: 54). Undoubtedly, a continuous exposure to violent oppression regarding a person’s inherent cultural or racial self- integrity may shape PTSD symptoms. This is happening mainly because both racial and ethnic features are innate, and individuals are victimized due to their identity that under pressure leads to denial of their self-identity and self-hatred or constant fear to be judged and blocked from opportunities. In other words, on a regular basis individuals receive a reminder from a society that they belong to a marginalized group, and this fact shapes a cycle of oppression so the brain stays in the state of constant alert, developing symptoms such as aggression, anxiety, depression, panic attacks, etc.
Now, the dilemma of trauma targeting minority groups is that mostly it involves psychological abuse rather than the physical one, and for this reason, it is easy to overlook the problem since it may be a victim's subjective interpretation of events. Thus, the scholarship has identified that it is important to distinguish the difference between harassment and discrimination. If, indeed, the harassment includes the active person-level discrimination that is more straightforward, the discrimination itself is more passive and may be emotionally avoidant. Helms and Nicolas (2010) revealed the findings that “people’s psychological and emotional reactions to racial harassment were more intense and lasted longer than their reactions to racial discrimination” (Helms & Nicolas, 2010: 56). What’s more, another investigation shows a high correlation between identity-based violence and symptoms as well: the higher levels of such racism-related experiences, the higher levels of general stress, suicidal ideation, state and trait anxiety, and clinical depression are being produced (Helms & Nicolas, 2010: 58). Hence, it is possible to conclude that the more racism or ethnoviolence takes the harassment approach, the more interpersonal it becomes, and receives more adverse impact on an individual's self-reflection and self-recognition in society. Despite the missing traces of physical abuse, psychological abuse involves verbal and non-verbal communication: with racism and ethnoviolence it includes the negative treatment that a victim cannot change (gender, race, ethnicity, religion) causing existential crisis. This is crucial to highlight because it is massive and being characterized with inner conflicts due to confusion of personal identity. Consequently, it destroys an individual’s vision of the world, making him/her vulnerable in every single aspect: self-development, personal relationships, career, etc.
That being said, writing this blog post, I would like to state that even though identity-based traumas are silent, they cause alienation that deeply affects emotional, cognitive as well as behavioral elements of an individual. The revealed fact that passive discrimination does not contribute as much as the individual harassment, does not mean that it does not add to each person individually as a global tendency shaping the overall climate of alienation. Discrimination cannot receive a full acceptance as a matter of fact, rather it is manifested through unreported PTSD symptoms that these individuals tend to deny as a priori position themselves as a failure due to both overall discrimination and individual harassment. However, previously each representative of minority groups could experience discrimination in particular dimensions of life such as job applications, healthcare, criminal justice system, education that are more systemic at this point, while returning to communities they could have regained support from each other to maintain positive attitudes that contribute to the personal growth and reduction of stress. It reminds me of Jane McGonigal’s performance regarding the post-traumatic growth where she has developed a game approach called “Superbetter” with the stages of recruiting allies, battling the bad guys and activating the power-ups (Rousseau, Module 1, 2023: 8). This is why the past is full of motivational stories of success among African Americans starting from sports, music/entertainment industry and finishing with politics. Conversely, today the world has shifted towards the implementation of advanced technology and spread of social media that made us accessible and visible wherever we are, unless we are connected to the Internet. The space without time and territorial boundaries established the new reality where it has become possible to freely express your opinion on everything, while reaching everyone with a distance of one click. While we are at home, in our workplace or in the restaurant with our friends, we are exposed to people’s judgments online via their posted comments. Thus, I claim that racism and ethnoviolence has received a new form of manifestation in the cyber environment: this is the hateful speech online against minority groups or particular ethnic groups that tends to tremendously contribute to the alienation of individuals, developing an existential crisis followed by PTSD symptoms.
The controversy of the given issue is that minority groups are being targeted by users online being exposed to traumatic non-stop experiences without proper protection by law enforcement. This occurs due to the First Amendment in the US Constitution where basically oppressive comments are being covered by the freedom of speech: “Congress shall make no law respecting an establishment of religion, or prohibiting the free exercise thereof; or abridging the freedom of speech, or of the press; or the right of the people peaceably to assemble, and to petition the Government for a redress of grievances”. This fact makes victimized people accept their struggles on a daily basis, while entering a cycle of psychological abuse and accumulating all possible post traumatic symptoms. Now, hateful speech can be considered as “words that wound”, even though as it was stated there is no direct physical violence applied. The amount of hate exposure measures the extent of trauma that we eventually get. Thus, it is necessary to know how this procedure works. First, what provokes the danger to happen is the fact that Internet forums / social media shape a digital relationship between anonymous or pseudo-anonymous users, suitable targets for hateful or defamatory messages and the ISP (the Internet Service Provider) that serves as a gateway (Nel, 2007: 193-195). Interestingly, anonymity in this relationship is a variable that enables one’s identity to be concealed for enjoying the social benefit of privacy and free speech (according to the First Amendment in the US jurisdiction) but simultaneously creates a hole in the protection of an individual’s inalienable rights, in particular, the freedom from discrimination and degrading treatment. Meanwhile, a suitable target as a variable falls into the received gap, precisely, focusing on the category of minority groups. The interaction online starts as a regular comment/post, then grows into a hateful message and finally reaches its climax at subsequent hate speech. This leads to a research question: can we balance the rights of free speech belonging to a user and the rights of equal treatment and personal security that are inherently owned by a targeted victim online (Universal Declaration of Human Rights, 1948: Articles 1-5)? The lack of this balance currently results in the deprivation of individual dignity with a subsequent increase in dehumanizing victims since what exactly is targeted in minorities is their personal profile (sexual identity, race, religion, etc), leading to damage of their psychological state, brain or other irreversible outcomes such as alienation, loneliness, despair and finally, suicidal thoughts.
In the settings of the current unstable political climate, I would like to illustrate how this phenomenon affects not only racial minorities but also larger populations of ethnic groups. Once the Russian-Ukrainian conflict started, a lot of social media such as mainly Facebook and Instagram exploded with the amount of hateful comments regarding Russians being all killers and aggressors, even though from the ongoing events not all the country’s population supported the invasive actions of the government. Comments by users contained violence and threats where the main message was that “Russian nation should be eradicated”. For this reason, the Russian authorities took a decision to prohibit Instagram in the Russian jurisdiction, claiming that it is violence-oriented platform trespassing on the individual dignity of citizens. Personally being of Russian origin, even though I was not directly affected by hateful comments (since I limit my participation in the digital daily routine), I received vicarious trauma from reading the hate from thousands of users. As a regular civilian, I couldn’t understand why they wanted me to die just for being ethnically who I am, while I am not even closely related to the ongoing military actions. My trauma started growing from the fact that I did not want to answer questions regarding my descent because I did not want to be judged and finished with self-blaming why I happened to be born as Russian. This journey of trauma demonstrates that I entered the existential crisis, started being confused about who I am since my ethnic background was questioned. Consequently, racism and ethnoviolence tend to break mentally individuals, and if this experience is uniquely new for them, they may not be familiar with how to handle their feelings and opt for silence.
To conclude, I chose racism and ethnoviolence as an overlooked type of accelerators for trauma among racial minorities and ethnic groups. Even though the scholarship is cautious with these issues due to subjective interpretations, the research revealed that harassment may exacerbate PTSD symptoms compared to passive discrimination. However, I claim that today we experience a new catalyst of traumas which is hateful speech online due to the advent of advanced technology and the Internet. I find the given event anti-spatial and diffusing, meaning that it can contribute to people’s exposure to oppression and trauma anywhere anytime, without any right to escape. I have also commented on the contentious lack of legal protection that makes racial minorities and ethnic groups vulnerable and thus more swiftly exposed to the gain of traumatic experiences and development of PTSD symptoms since they enter an existential crisis that is characterized as the confusion of identity. Thus, identity is the main targeted asset that perpetrators aim for to humiliate victims. With assistance of the personal example of online ethnoviolence, I demonstrated how the given relationship operates and which directions trauma may take if being overlooked. To combat the given issue, I think we should find the balance in how to ensure “digital security” on a legal level by avoiding excuses such as freedom of speech since this phenomenon cannot cross somebody else's boundaries, otherwise it takes the form of injustice. Furthermore, I believe that we should invest more resources in educating people’s digital literacy because sometimes the reason why individuals do not report their PTSD symptoms is because they do not realize that they have them just because of constant exposure to stress, violence and discrimination online. The more awareness is being shaped on this problem, the more people or their relatives, community members may recognise the need for help to prevent the development of the given symptoms in advance.
References
- Helms, J., Nicolas, G., & Green, C. (2010, January 01). Racism and Ethnoviolence as Trauma: Enhancing Professional Training. Traumatology, 16(4) 53-62.
- Nel, S. (2007). Online Defamation: The Problem of Unmasking Anonymous Online Critics. The Comparative and International Law Journal of Southern Africa, 40(2), 193–214. http://www.jstor.org/stable/23252662
- Rousseau, D. (2023). Trauma and Crisis Intervention. Module 1. Introduction to Trauma. MET CJ 720. Boston University.
- U.S. Constitution - First Amendment | Resources | Constitution ... (n.d.). https://constitution.congress.gov/constitution/amendment-1/
- United Nations. (n.d.). Universal Declaration of Human Rights. United Nations. https://www.un.org/en/about-us/universal-declaration-of-human-rights
Community Trauma
As this course, along with the rest of the courses for this term close to an end, I’m often thinking about how my courses relate to each other and the real world. One thing that I have been left thinking of is trauma, and how traumatic events affect the community. In one of my other courses, I am looking at aggravated assault incidents, drug related crimes and poverty within a city. Looking at all of this data has left me wondering how communities that are constantly experiencing traumatic events cope, or if they just view it as their new normal. Communities who experience traumatic events once, whether that be neighborhoods that are experiencing an act of violence such as a homicide, or on the larger scale such as the events of 9/11 or the Boston Marathon, seem to be shocked to their core after the events that have happened, and these are usually broadcasted all throughout the media. What about communities who constantly, or on a more continuous basis, experience trauma? Do they build their own subculture around this trauma, and have it become their new normal? Or is it still traumatic every time an event happens, even though they happen frequently?
If you look at this on an individual basis, everyone reacts to trauma differently. With constant exposure to traumatic events, some people continue to view these events as traumatic, while others become desensitized to them. When looking at the community level, how do we support them as a whole? If a whole community is desensitized from all of the trauma they have experienced, how do we treat that at the community level, especially if that is the only normal that the community has ever known? Some responses to this might be to maybe open a neighborhood center where the kids within the community have somewhere to go, or to work on lowering the crime rates in the area.
Going Hand in Hand: Homelessness and Trauma
The subject of trauma is one that can have a significant impact on an individual no matter what point or chapter they are at in their life. Whether a person is living their best life in a LA penthouse, traveling the world and visiting Europe, or sitting on the corner of a street begging for spare change or a bottle of water- we all experience trauma on a daily basis. Homelessness is defined under several factors of having no place to call home- thus resulting in being on the streets seeking assistance from others. Many people feel trapped once they are out on the streets, as it is considered a chronic stressor that cannot be escaped due to a lack of motivation and assistance (Rousseau, 2023). There is a negative stigma brought along with this, as many individuals think that homelessness is a result from drug abuse, not searching hard enough to find a job, overwhelming financial burdens, or simply doing it to themselves and not caring about their future. This is in fact not accurate for every individual, as we see this with veterans struggling to find an income when back from war, a traumatic event that left them in a state of shock, losing or getting fired from a job, and much more. Being homeless in itself is more than traumatizing, and advocating for more awareness and opportunities to reduce the rate of people sleeping on streets under cardboard boxes is something that should be prioritized.
The first step of implementing more programs and resources starts with individuals grouping together and brainstorming ideas in which we would see a positive difference in the percentage of homeless people. Homeless shelters are a great place to bring in additional help from volunteers, psychiatrists, and therapists. There tends to be a common variable of PTSD in homeless people- in which this goes along with anxiety and depression from how impactful their trauma was (Rousseau, 2023). We see an example of this with a case study spotlighting “Ms. Harris”, a “middle-aged woman with a history of PTSD and alcohol use disorders who is currently receiving substance use treatment at a local homeless shelter” (Williams, 2022). With an extremely challenging time growing up, along with a rough adulthood and getting divorced, which resulted in a big loss of financial savings, she had nowhere to turn to besides a medical unit for treatment because she was not helping herself in any shape or form. Like herself, “some studies show the prevalence of alcohol dependence of homeless patients to be upwards of 55%, and similar rates of drug dependency” (Williams, 2022). She had gotten prescribed for PTSD and her alcohol use disorder, and as time goes on there has been a remarkable change in her life due to having all these resources at the shelter. Psychiatrists who have the opportunity to be that one person for these struggling individuals is not only rewarding for both of them, but allows outsiders in society to see that these programs are worth it and are beneficial to whoever utilizes them.
Ways in which there has been improvement in the mental health and trauma concentration for homeless people can be shown throughout multiple examples in society. Focusing on trauma and how an individual can perform their daily routine while coping with it is important, especially when trying to get back on your feet and find a place to work/live. The Treatment for Individuals Experiencing Homelessness helps those who are homeless and struggling with mental and substance abuse disorders, as the “goal of the program is to increase access to evidence-based treatment services, peer support, services that support recovery, and connections to permanent housing” (Substance Abuse and Mental Health Services Administration, 2023). The program excelled so much in helping individuals that the SAMHSA announced 31 awards with the total contributions adding up to $15.8 million dollars (SAMHSA, 2023). Another rewarding program was the National Child Traumatic Stress Network, founded in 2001 with a “network of more than 150 centers nationwide” (Van der Kolk, 2014). The different projects were placed in shelters, group housing units, juvenile justice systems, correctional facilities, and any place where an individual might be fighting trauma on a daily basis on top of the hardships stemming from homelessness. The constant use and dedication of these two programs alone has made such an impact on homeless people and their constant trauma, making for a brighter future and a place to call home.
References:
Rousseau, D. (2023). Trauma and Crisis Intervention. Module 1. Introduction to Trauma. Metropolitan College Boston University.
Substance Abuse and Mental Health Services Administration. (2023, December 5). Homelessness Programs and Resources. SAMHSA. https://www.samhsa.gov/homelessness-programs-resources
Van Der Kolk, B. A. (2014). The Body Keeps the Score: Brain, Mind and Body in the Healing of Trauma. Viking.
Williams, J. (2022, September 1). “I have no one”: Understanding homelessness and trauma. Psychiatric Times. https://www.psychiatrictimes.com/view/i-have-no-one-understanding-homelessness-and-trauma
Bounce Back Program
Children can suffer severe psychological distress when they have experienced adversity, and it is crucial that we make programming to treat child PTSD. To begin treating child PTSD in school settings, “Bounce Back” was created by the UCLA Semel Institute for Neuroscience and Human Behavior (Blueprints, 2023). The “Bounce Back” Program is a cognitive-behavioral group intervention meant to assist in relieving symptoms of childhood PTSD, anxiety, depression, and functional impairment for elementary school children ages 5-11 (CEBC, 2015). The program serves children who are affected by community, family, or school violence, natural disasters, or traumatic separation from a loved one due to death, incarceration, deportation, or child welfare detainment (CEBC, 2015).
The goals of Bounce Back are to reduce symptoms of PTSD, depression, and anxiety, build skills to enhance resilience to stress, enhance students coping and problem-solving strategies, impact students’ academic performance by improving their attendance and ability to concentrate, and build peer and caregiver support (CEBC, 2015). The program is made up of 10 one-hour group sessions, three individual sessions, and one to three parent education sessions over the course of three months. Group sessions are held during school hours and focus on topics like relaxation training, cognitive restructuring, social problem solving, positive activities, trauma focused intervention strategies, emotional regulation and coping skills (Blueprints, 2023). Many of the topics are tailored for the age group that receives them, utilizing storybooks, and games in engagement activities.
The outcomes of the program were very positive, with the Bounce Back program posttest treatment yielding results of significantly improved PTSD symptoms (parent and child reported), anxiety symptoms (child reported), emotion regulation (parent reported), and emotional and behavioral problems (parent reported) (Blueprints, 2023).
Cited limitations for the initial study were a small sample size, lack of control group at three month follow up, and length of follow up (CEBC, 2015). Something that could be added to this program is assessment of ACE scores for the children who are receiving treatment, to identify what kind of care plan they may need. High ACE scores leave children more at risk for PTSD and other conditions, so it may be beneficial to assess risk by administering the ACE test to the elementary school participants. However, from a round table view, “Bounce Back” could be what school systems need to treat childhood trauma and support at risk students who face adversity.
References:
Blueprints. (2023). Bounce Back. Blueprints for Healthy Youth Development. https://www.blueprintsprograms.org/programs/1074999999/bounce-back/
CEBC. (2015). Bounce Back. CEBC " Bounce Back ’ Program ’ Detailed. https://www.cebc4cw.org/program/bounce-back/detailed#:~:text=Bounce%20Back%20directly%20provides%20services,attendance%20and%20inability%20to%20concentrate
The Trauma of Incarceration
One of the readings I found to be most interesting this semester was The Trauma of the Incarceration Experience as it discusses a topic I had previously written about in my documentary review. This reading describes the trauma inmates face in the prison system. With over 10 million individuals being incarcerated at any given time world wide, the rates of traumatic experiences and mental health issues that prisoners face are quite high (Piper & Berle, 2019, pg. 1). It is common for people who have been incarcerated to describe unimaginable violence and horrors that they have witnessed during their time in jail. Both DeVaux and Browder described witnessing violence, and both had experiences where defending themselves from violence led to them facing solitary confinement. These experiences that inmates face can lead to things such as PTSD, as an article from 2019 found that “Research examining PTSD in incarcerated populations reported estimates at a staggering 48%, compared to lifetime prevalence rates of 8.7% in the general US population” (Piper & Berle, 2019, pg. 2). These rates emphasize the need for trauma informed care in the carceral system in the United States. Providing trauma informed care to people who are incarcerated could be incredibly beneficial to their mental health, and decreasing recidivism rates.
For the documentary review I watched Time: The Kalief Browder Story. It’s a documentary about Kalief Browder who was 16 years old when he was falsely accused and arrested for stealing a backpack. He was sent to Rikers Island where he was frequently beaten and put in solitary confinement for a majority of the 3 years he spent in jail. He struggled immensely after being released due to the trauma he faced while being incarcerated, and at the age of 22 he committed suicide. His story highlighted the trauma inmates face in prison, and this article also describes a first hand experience of trauma in the carceral system. A quote that I found incredibly important from The Trauma of the Incarceration Experience was that “The experience of being locked in a cage has a psychological effect upon everyone made to endure it. No one leaves unscarred.” (DeVaux, 2013). Kalief also described the impact that incarceration has on everyone that faces it, and the lack of support given to him while he was incarcerated during his as an activist. This article by DeVaux explains how “people in prison may be diagnosed with posttraumatic stress disorders, as well as other psychiatric disorders, such as panic attacks, depression, and paranoia; subsequently, these prisoners find social adjustment and social integration difficult upon release” (DeVaux, 2013). Prison can cause long lasting mental health issues, and oftentimes these issues are not treated while in prison, making the adjustment back into the community more difficult.
During Browders time at Rikers Island, he experienced a severe mental health decline, and despite begging prison officials for help and treatment, his pleas were ignored. Despite the fact that treatment for him could have been life saving, he was denied help multiple times, causing his suffering to worsen. Kalief spent 700 days in solitary confinement, which accelerated the rapid decline of his mental health. According to Chadick et al, those in solitary confinement “typically spend 22–24 hrs of isolation with approximately 1 hr allotted for exercise or shower each day; some facilities only allow shower time three to 4 days a week” (Chadick et al, 2018, pg. 2). As social creatures, this isolation can have severely detrimental impacts on inmates and their mental health. A study from 2001 looking at the impact that solitary confinement (SC) has on mental health found that the “Incidence of psychiatric disorders developed in the prison was significantly higher in SC prisoners (28%) than in non-SC prisoners (15%). Most disorders were adjustment disorders, with depressive disorders coming next” (Anderson et al., 2001). They found stress to be a major contributing factor, which oftentimes prisoners in solitary confinement experience extreme levels of stress in isolation. Chadick et. al stated that prisoners in solitary confinement often “experience a myriad of mental health concerns and symptoms, including appetite and sleep disturbance, anxiety (including panic), depression and hopelessness, irritability, anger and rage, lethargy, psychosis, cognitive rumination, cognitive impairment, social withdrawal, and suicidal ideation and self-injurious behaviours” (Chadick et al, 2018, pg. 2). Implementing trauma informed care in our prison systems could be beneficial because “ all staff can play a major role in minimizing triggers, stabilizing offenders, reducing critical incidents, de-escalating situations, and avoiding restraint, seclusion or other measures that may repeat aspects of past abuse” as the prison setting is full triggers that could be impacting the mental health of inmates (Miller & Najavits, 2012).
Kalief also described post-release how difficult it was for him to adjust and integrate back into society. He was enrolled in college before his passing, but it was something he really struggled to adjust to due to the trauma that he faced. With trauma-informed care and better support during his transition from jail back into the community, Kalief could have had the support he needed in order to adjust smoothly and thrive post release. He struggled for the remainder of his life due to the trauma and lack of support he faced during his time in jail, but spent the remaining time after his release advocating for better treatment of those who are incarcerated. The trauma that both of these men faced during their time in jail is something that impacted them for the rest of their lives. I had watched the Kalief Browder documentary when it first came out in 2016, and it was just as impactful to watch now as it was the first time I saw it. Devaux’s experience in the system is incredibly similar to Browder’s, and unfortunately many others have had similar experiences. Kalief described the same paranoia that Devaux had, and both also described witnessing and experiencing unimaginable violence. Kalief’s story was one of the first times I had realized the trauma inmates face in the system, and this article gave me an even better insight and understanding as to how the carceral system facilitates traumatic environments for inmates.
Resources:
Andersen, H. S., Sestoft, D., Lillebaek, T., Gabrielsen, G., Hemmingsen, R., & Kramp, P. (2000). A longitudinal study of prisoners on remand: psychiatric prevalence, incidence and psychopathology in solitary vs. non-solitary confinement. Acta psychiatrica Scandinavica, 102(1), 19–25.https://doi.org/10.1034/j.1600-0447.2000.10200
Chadick, C. D., Batastini, A. B., Levulis, S. J., & Morgan, R. D. (2018). The psychological impact of solitary: A longitudinal comparison of general population and long‐term administratively segregated male inmates. Legal and Criminological Psychology, 23(2), 101–116. https://doi.org/10.1111/lcrp.12125
DeVeaux, M. (2013). The trauma of the incarceration experience. Harvard Civil Rights–Civil Liberties Law Review, 48
Miller, N. A., & Najavits, L. M. (2012). Creating trauma- informed correctional care: a balance of goals and environment. European journal of psychotraumatology, 3, 10.3402/ejpt.v3i0.17246. https://doi.org/10.3402/ejpt.v3i0.17246