Home
Obedience/Conformity to Legitimate Authority Figures
For my module 5 react post, I spoke about a qualitative research paper I completed for my undergraduate degree. My paper discussed obedience to authority figures; for my paper, I used Stanley Milgram’s experiment as my primary inspiration. The fundamental question I attempted to answer was: why do individuals obey orders they know are wrong? In addition, I explored why individuals may obey/conform to orders that make them feel uncomfortable.
As this course draws to a close and I think about what I have learned, I reflect on my paper. With my newfound understanding of trauma, I think about how obedience to authority and exploitation of authority can lead to trauma. In my paper, I examined conformity in work environments and how one’s relationship with their superior may influence their level of conformity. I focused primarily on orders or requests that the employee explicitly knows are wrong. For example, maybe their superior asked them to do a task that cuts a corner and violates the policy; or, their superior constantly asks them to stay later or lock up by themselves. Simple everyday orders that are wrong, yet are still obeyed.
I found that most people obey/conform simply to maintain a harmonious relationship. A subordinate remonstrating against their superiors’ orders would most likely cause some rift in the relationship which could have undesirable effects on their day-to-day work experience. Unfortunately, I was not able to explore how this principle of maintaining harmony could intertwine with trauma. At the Nuremberg trials, many soldiers maintained that they were simply following orders. These orders came from individuals they viewed as a legitimate authorities. For Milgram, the subjects in his experiments followed orders because it came from a person of legitimate authority (a doctor in a white lab coat).
Following this course, I would have liked to explore the exploitation of authority and conformity through the lens of sexual misconduct, especially in workplace and home environments. Oftentimes superiors are able to use their positions to exploit others. While interning at the special victims unit, countless cases I read involved a child and someone they trusted (parent, family friend, teacher, etc). Time and time again, people in trustworthy/powerful positions are able to use their “legitimacy” to exploit others. Milgram found that individuals enter into two states of behavior when depending on the social setting, autonomous and agentic states. In the autonomous state, individuals will carry out their own actions while also taking responsibility for those actions. In the agentic state, individuals will take a back seat and allow others to direct their actions, individuals will also allow others to shoulder the responsibility or consequences of those actions. Milgram believed that people will obey authority under the assumption that the person giving the orders will bear the responsibility for their actions.
References:
Rousseau, D. (2022). Module 5: Trauma, Genocide, and the Holocaust. Blackboard
Service Dogs Blog Post
For my blog post, I chose to further my previous post on the therapeutic approach of having a service dog to help address trauma. The therapeutic approach to addressing the impact of trauma that I originally chose was service dogs. The purpose of having a service dog for someone with trauma is to help aid them in times where the owner's symptoms prevent them from being able to do a task. For instance, some of the more basic services that these dogs can provide are, "to guide a disoriented handler, find a person or place, conduct a room search, signal for certain sounds, interrupt and redirect, assist with balance, bring help, bring medication in an emergency, clear an airway, and identify hallucinations" (Rousseau, 2022). Service dogs not only help people with PTSD, but can help people with all different types of disorders, whether from trauma or other similarly mentally altering experiences. They are also commonly used for people who are blind, for those who have seizures, and for those with severe anxiety, from what I have witnessed.
Some people prefer to have their service dogs where a vest, so that people do not try and pet or distract the dog from doing its task (servicing his/her owner). These vests tend to say things like "working dog", "do not pet", or "service animal", etc. in hopes that people will leave the animal be while it is actively working. It is crucial that service dogs stay completely focused on their task while they are "on duty". However, some people have used the term "service animal" lightly and as an excuse to be able to bring their dog(s) from home and into stores with them. This could especially be concerning if the fake service dog reacts to the real service animal, and in turn, distracts the service dog from staying focused.
Although service dogs are great for aiding people with trauma, they are in no way capable of completing relieving one of the symptoms that they experience. Unfortunately, none of the therapeutic approaches addressing trauma can guarantee to completely cure someone of their trauma, but they most certainly can help a great deal. Overall, these dogs focus on ways to support their person before, during, and after a trigger may occur. In some instances, a service dogs actions could be the difference between life or death for someone who cannot get the help for themselves. Service dogs are very effective for many people who have trauma, and they can make for a great therapeutic approach in addition to other forms of therapy.
As mentioned before, even for people that are not diagnosed with PTSD, but who have mental health related issues, service dogs can be great. Additionally, other types of animals can be just as therapeutic, as we are continuing to learn about the benefits of animals with mental health. I personally have met people who struggled with trauma or their mental health, and had a service animal other than a dog. Although the animal may not be able to do certain tasks that a dog could, not everyone has the same opportunities to own a dog. Therefore, other (smaller) animals are still helpful in providing that 24/7 comfort to someone who struggles with their mental health and may need in order to function throughout their day.
References:
Rousseau, D. (2022). Module 4: Pathways to Recovery: Understanding Approaches to Trauma Treatment. Blackboard

By: Cameron Kunkle
Workplace Violence in the Emergency Department
Workplace violence (WPV) in the emergency department is entirely too common. Emergency medicine has one of the highest rates of WPV each year (Hartnett & Jasani, n.d.). The movement against WPV in healthcare is geared toward resources for nurses, as they spend the majority of the time with a patient, but it is an important factor for techs, CNAs, doctors, and any healthcare staff present in the midst of an incident. I have worked in the emergency department for about seven or eight months now and I have seen and heard of at least five or six different incidents of WPV, one of them being my own experience. The types of WPV range from tight grips in which a patient refuses to let go (this was the matter in my case) to having bones in the face or hand broken to the point where someone's career is ended. During my orientation on the job, I was informed that the reason we have signs for some patients saying "see patient's nurse before entering room" is because a nurse was killed by a patient when she was not fully informed of the background of a patient.
This leads to primary trauma being prevalent on the job for healthcare workers as well as the already established secondary (vicarious) trauma that is frequently experienced by first responders in the field and in the emergency room. One of the first steps to resolving WPV as a whole is to know how often it is happening, who is perpetrating it, and who is being targeted. One of the main barriers to this is the fact that staff often do not know what acts constitute violence (Stene, Larson, Levy, & Dohlman, 2015). I was surprised that my incident had to be reported as WPV. It was scary, of course, because the guy was like 6'5", 200-something pounds, psychotic, and wouldn't let go of my wrist that he was holding incredibly tightly, but it didn't seem like a particularly violent act (though my wrist was and still is sprained). It wasn't until I had to document the report (because security had to be called) that I was told by a senior nurse that the proper documentation would be listed under WPV.
Most healthcare workers in the emergency room report that they feel that violence is an expected part of their job as a part of the emergency department (Hartnett & Jasani, n.d.) I think that part of this is due to the fact that many times, even when not necessarily indicated, police will bring in patients who are a risk for violence. Then when we try and press charges because we've been assaulted, the police will often want to leave that patient at the hospital because they don't have the resources to deal with them or believe they still have to be treated, even when the doctors have cleared the patient. This also leads to a large number of healthcare workers not pressing charges against those who perpetrate WPV. Even when our employers back us up, this lack of support from the other emergency services that exist for purposes such as responding to WPV leads to a sense of learned helplessness. Asking for help feels like it won't do that much, so people don't ask for help. We just expect this to be a part of the job.
This expectation, primary trauma, and secondary trauma are all significant factors leading to professional burnout and stress disorder symptomology (not to mention the actual physical trauma that often accompanies WPV).
References
Hartnett, E., Jasani, G. (n.d.) Emergency Medicine on the Frontline: Workplace Violence in the Healthcare Setting. AAEM and Student Association. Retrieved from https://www.aaemrsa.org/advocacy/resources/workplace-violence
Stene, J., Larson, E., Levy, M, & Dohlman, M. (2015). Workplace violence in the emergency department:
Giving staff the tools and support to report. The Permanente Journal, 19(2), 113-117. doi: 10.7812/TPP/14-187
SGB Treatment for PTSD
Upon his return to civilian life after having served in Afghanistan and Iraq, Army Sergeant Sean Messett struggled with PTSD. Having tried therapy and medication management with no relief, Sergeant Messett heard another veteran speak on a podcast regarding an injection, or stellate ganglion block (SBG), that he had just received himself. With the help of Hanover's For the Love of a Veteran Inc., Sergeant Messett received this injection, and it has changed his life.
SGB treatment consists of a localized injection of insulin into the individual’s stellate ganglion nerves, which are part of the sympathetic nervous system. This consists of a bundle of nerves that are directly connected to the sympathetic nerve, which triggers the body’s reaction to situations of stress or danger. This in turn causes the amygdala to release hormones that produce the fight or flight response. In the case of an individual whose amygdala and medial prefrontal cortex within the frontal lobe have been dramatically changed by trauma, this person can exhibit extremely emotional, angry, fearful or violent responses and/or reactions. The insulin injection serves to reprogram or restart one’s system, working to return it to normal functioning, pre-trauma.
Studies have shown that success rates range from 80-90%, results are immediate and can last from months to years dependent upon the patient’s needs and response to the injection. While SGB is not a cure, it greatly assists with talk therapy, as it allows patients to be able to think clearer and slow down their mind which was previously always on high alert. Individuals report being able to rest, decrease anger, stress and anxiety, and to reconnect with loved ones.
Quincy Kasper is another veteran who has benefited from the SGB injection. As an advocate for veterans with Post-Traumatic Stress Disorder, he states: ““The only way we’re going to be able to continue to help people and continue to move forward with this is to be talking about it. Because, again, mental health has such a stigma.” (Kasper, Q., 2022). With the overall successfulness of SGB treatment, perhaps more individuals will feel less stigmatized and feel more comfortable in seeking the help they may need.
References:
Escalante, A. (2021). Helping PTSD With A Shot: The New Treatments That Are Changing Lives. Forbes. Retrieved from: https://www.forbes.com/sites/alisonescalante/2021/02/02/curing-ptsd-with-a-shot-the-new-treatments-that-are-changing-lives/?sh=55ff1ed06912
Mediak, G. (2022). Injection helping veterans manage PTSD symptoms. Fox43. Retrierved from: https://www.fox43.com/article/features/sbg-insulin-injection-veterans-ptsd-stellate-ganglion-block/521-49967b48-9e4c-42a1-a2ff-2bdfbed02b46
Rousseau, D. (2022). Neurobiology of Trauma. Module 3. Boston University Metropolitan College.
SGB for Vets (2022). Treatment for PTSD. Retrieved from: https://www.sgbforvets.com
Sutherland, D. (2022). Veteran gets effective PTSD relief through injections. 7WSAW-TV. Retrieved from: https://www.wsaw.com/2022/11/19/veteran-gets-effective-ptsd-relief-through-injections/
Van der Kolk, B. (2014). The Body Keeps the Score: Brain, Mind, and Body in the Healing of Trauma. New York, NY: Viking.
Yoga Blog post
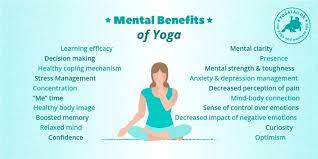
For my blog post, I decided to expand on my previous discussion post and use a visual representation to promote the benefits of yoga for physical, mental, and spiritual wellness. As I mentioned in my earlier post “ My older brother has brain stem damage due to repeated concussions from playing sports which has slightly altered bits of his personality, making him more hot tempered for example, as well as (we believe) played a part in helping with the onset of some mental and emotional struggles he's dealt with other the past few years. Yoga was one of the first therapies he used that helped him to feel better both physically and mentally.” When I was younger both my parents had also practiced yoga to a small extent and had tried to get my brother and I involved but as children this was difficult because we found it hard to sit still and make that mind-body connection because we couldn’t understand it. Now after COVID (which my family used as a period for fitness, mostly to burn energy so we didn’t turn our pent up energy on each other) my brother as I said, my father, and myself all have used yoga as a mindfulness practice just as much as a physical workout. This semesters readings finally made that connection for me. I never understood the why behind Yoga as a intersectional wellness activity until now. One of the pieces I did not mention in my previous post but I found enlightening is that many of the intimate actions in yoga, such as the happy baby pose, can be triggering for some individuals, the idea of mimicking of movements that occurred during their traumatic experiences causes many to freeze. It is not until individuals can learn to breathe, push through, and maintain this pose or the physical touch of an instructor that they can “let go” or feel the relief of a deep breath and begin to relax. Now while I do not have the same experiences as these individuals, I can feel this sense of relief on a smaller scale, when I can finally hold a pose or a certain muscle that has been tight all week finally relaxed through my yoga movements it is a relief and also gives me a sense of pride as I have been able to accomplish what many from the outside see as a simple task but to me it takes the discipline of both my mind and body working together to do it. I also think that yoga, or any workout routine can also assist in the treatment of trauma. As we’ve mentioned in both lecture and posts throughout the semester, people who are mentally suffering are often unable to lead goal driven lives, they are too focused on the now. So these workout routines not only require forethought and planning by the individual but also creates easily understandable goals, such as holding a pose to a certain amount of time or gaining the flexibility to even be in a certain pose at all.
Van der Kolk, Bessel . The Body Keeps the Score. Penguin Publishing Group. Kindle Edition
Rousseau, Danielle, Lecture, Trauma and Crisis Intervention.
Trauma’s Effect On the Brain
Trauma impacts an individual’s body physically, mentally, and emotionally. Whether someone has experienced abuse, war, accidents, natural disasters, any violence, etc., the body creates imprints of these memories on the brain and body causing major changes. While these changes and reactions are detrimental to someone’s health, there are ways to heal from traumas and help individuals keep living their lives. Due to the impact on the brain and body, a person’s life can be flipped around without much understanding of why. Sometimes, the hardest element to consider for someone affected by trauma is understanding the neurological aspect of what has happened to them, what it means in terms of their lives, why it affects them the way it does, and how healing is possible with these unchanging effects.
Before turning to criminal justice, I began as a psychology undergrad. In this time, a main component we learned of was the “3-part brain” or the Triune Brain model (also mentioned in Rousseau’s Module 3). In this model, it is said that there are three parts that make up the brain: the brain stem (reptilian), the limbic/midbrain (mammalian), and the cortex/forebrain (neommalian). The Reptilian is responsible for survival instincts and automatic body functions, the mammalian is responsible for emotions and sensory input, and the neommalian is responsible for decision-making, learning, and memory. All three components are impacted during a traumatic experience, some more than others. The reptilian brain (survival instinct) takes over during a trauma triggering fight or flight and turning off all non-essential bodily functions. Typically, after a traumatic experience has ended, the body is able to switch back to homeostasis- reducing the fight or flight hormones and returning the non-essential bodily functions. For those individuals who end up developing PTSD, however, this switch back to homeostasis never happens. The reptilian brain never returns function to the rest of the other brain areas, leaving them in a continuous state of reactive mode. This reactive mode leaves individuals with symptoms that they don’t understand (PTSD symptoms like mood swings, being easily startled/triggered, having undesirable memories, etc.). This leaves people feeling a loss of control over their own thoughts, decisions, and functions.
The brain itself goes through a biological change after trauma. Several things happen that wouldn’t happen to a brain that has not experienced trauma. A major piece of the brain (and my personal favorite to talk about) is the amygdala. This small formation located close to the center of the brain is responsible for processing threatening stimuli and activating the appropriate response. It also connects emotions to certain memories. In a traumatic situation, the amygdala becomes overstimulated and starts processing everything as a threat. Another crucial piece of the brain is the hippocampus. This part of the brain oversees learning and memory. To create memories, the hippocampus must make synaptic connections (between neurons, as noted in Rousseau’s Module 3) letting the body know that something is in the past and not happening currently- a memory. When the hormones from the fight or flight response are flooding through the body, they kill the cells that carry out these synaptic connections, making it challenging to let the body know that a traumatic event is over and in the past. This leaves the body in a continuous state of reactive mode. Lastly, the SNS (or sympathetic nervous system) manages that fight or flight mode; it releases epinephrine (adrenaline) into the bloodstream. With everything happening with the amygdala and the hippocampus, the SNS is constantly elevated and stressed unable to regulate or pass off to the parasympathetic nervous system, which would restore the body back to normal function and keep it from overworking. The combination of the three function dysregulations alters someone’s mind and body.
These changes, if left untreated can be detrimental. Thankfully, with what we know today about healing and PTSD, we know that healing is possible. All three brain areas can be restored to normal function, reducing the effects of trauma and sometimes eradicating PTSD symptoms fully. Individuals’ healing processes are all different and need to be treated as such in order to help create change.
References
Smith, I. (2021, September 22). How does trauma affect the brain? - and what it means for you. Whole Wellness Therapy. Retrieved December 2022, from https://www.wholewellnesstherapy.com/post/trauma-and-the-brain
Rousseau, D. (2022). Module 1: Introduction to Trauma. Boston University.
Rousseau, D. (2022). Module 2: Childhood Trauma. Boston University.
Rousseau, D. (2022). Module 3: Neurobiology of Trauma. Boston University.
Rousseau, D. (2022). Module 4: Pathways to Recovery: Understanding Approaches to Trauma Treatment. Boston University.
Theraputic Avenues for First Responders
Police Officer's and many other first responders have experienced trauma in many different ways. The job entails not knowing what you are going to be experiencing on the other side of the call. Many first responders hear that there is an accident that they have to respond to but they don't know that the accident could be fatal. Unfortunately, they are here to work for the community and with the community, so they can't just turn their eyes when going to the scene of a fatal accident. They actually have to take it a step further and assess the situation and make sure everything and everyone is safe before proceeding on with their investigation. Accidents and other different traumatic events can take a toll on officers and many other first responders like fire fighters, and EMT's. One of the solutions to this problem of dealing with traumatic situations is having therapy or (Critical Incident Stress Management) ready for the first responders when they get back to their station after their hard work out in the field. CISM offers meetings and privacy when talking about tough situations like the ones mentioned above.
“Police service is an inherently stressful occupation, which often results in both physical (e.g., cardiovascular, gastrointestinal, musculoskeletal problems) and psychological symptoms (increased depression, anxiety, posttraumatic stress disorder; e.g.,” (Berg et al., 2006). Members of the community don’t usually understand the traumatic events police officers and other first responders go through day in and day out. After responding to the scene of an accident, many of them feel they need to stand tall and not worry about what they might have just experienced at the scene. They try to bottle it up inside themselves and they can’t let anyone know that they are weak or can’t perform the duties of their job due to their weakness of seeing someone that has been deceased due to an accident or a harmful act from another's actions.
CISM (Critical Incident Stress Management) is a form of therapy for first responders and anyone who has experienced a traumatic event. An example of a critical incident is as follows “Critical incidents often include a component of life threat and may range from being threatened (e.g., with a knife or gun) to direct exposure and/or injury (e.g., accidental or intentional)” (Maguen et. al, 2009). CISM provides strategies to cope with these stressors. “The critical incident stress management strategies are very effective at lessening the burden on the officers, relieving some of the tension that they're feeling, and giving them some strategies and coping mechanisms that are healthy” (Abbott). In this case, we are talking about first responders and their trauma coming from a scene where there has been a death. CISM has two ways of bringing in the first responders to therapy. One of the ways is diffusing, which is a meeting that takes place with a therapist or mental health clinician right after they return to the station. This meeting will consist of having all responders to the call that was traumatic sit down and talk about what happened, what were some of the worst things that occurred at the call, etc. Basically, it is a chatting session to get the first responders to express how they are feeling and get some info off of their chest at the time after the call. The next part of the CISM strategy is debriefing. The Debriefing period happens a couple weeks after the incident. This is basically a follow-up period where the same group of first responders sits down and talks about what happened and what they have done to get their minds back on track. This is also a point in time when the therapist or the mental health clinician can help them to further their therapy if they need it. They will be able to provide different resources to benefit their well being and help them to get back on their feet. Having this program will help the officers and other first responders cope with the trauma they have been dealing with and make sure that they know they aren’t alone in this situation, they are always going to have someone that will have their back in making sure they have anything and everything they need.
Some of the fears that officers and other first responders have are losing their job, being reassigned, or having their licenses taken away which would prevent them from being able to complete their duties. In this case, police officers could lose their job, get reassigned to admin duties until they are back on their feet, or lose their license to carry a firearm within their department and state. All of these factors can lead to someone becoming depressed, which can then lead them to feel weak. They can prevent these types of things from happening if they get the help they need at the time when they need it the most.
I feel that all police and fire departments should have a mental health clinician on hand when there are traumatic events going on within the sector that the officers and firefighters are patrolling. Many police departments are now starting to hire mental health clinicians to help with the public needs and deal with many different mental health situations that police departments deal with on a daily basis. Along with the clinicians, I feel that CISM and CISD should be incorporated to make sure that first responders are getting the attention they need when they return from the scene. This is important for their well being and for their mental state of mind after experiencing tragic and traumatic events such as death.
References:
Berg AM, Hem E, Lau B, Ekeberg Ø. An exploration of job stress and health in the Norwegian police service: A cross sectional study. J Occup Med Toxicol. 2006; 1:26. Available at: http://www.occup-med.com/content/1/1/26. [PubMed: 17156489]
Maguen, Metzler, T. J., Mccaslin, S. E., Inslicht, S. S., Henn-Haase, C., Neylan, T. C., & Marmar, C. R. (2009). Routine work environment stress and PTSD symptoms in police officers. The Journal of Nervous and Mental Disease, 197(10), 754–760.
(n.d.). Two Primary CISM Strategies.
Restorative Justice in Young Adult Courts
The Use of Restorative Justice in Mitigating Young Adult Criminal Offenses

Three core concepts of Restorative Justice:
- Holding Offenders Accountable
- Repairing Harm to Victims
- Providing Support for Reintegration into the Community
This new concept is being trialed in several courts throughout the United States.
Young Adults (ages 18-25) are often referred to as emerging adults. We know that in the Criminal Justice System, juvenile offenders are afforded consideration based on their development, not only physically but also emotionally and cognitively. This category of offenders should also be treated as a separate group. Psychologists, physicians, and scientists have recognized the differences these young adults present concerning how they are intersectionally involved with the criminal justice system. Young adults have yet to fully form the cognitive or emotionally necessary development to appreciate the consequences of their impulsive actions. Innovative courts are responding to these theories and developing alternative methods of accountability.
One example is the Restorative Community Court in Cook County, Nevada. Participants must meet the following criteria:
- Be 18 to 26
- Have been charged with a nonviolent felony or misdemeanor
- Live, work or worship in one of the neighborhoods which has a community court
- Have a nonviolent criminal history
- Accept responsibility for the harm caused
“Twenty-nine young men and women now have clean slates after graduating from a six to nine-month-long program teaching participants conflict resolution and job skills. It even provides emotional support for overcoming trauma.” (Chicago, 2022)
This Program allows young people a chance to have a fresh start in an already stacked world. I am dedicated to spreading the word about such initiatives and hope to bring such ideas to my office.
Chicago, E. N. (2022, June 29). Cook County Restorative Justice Program Offers Second Chance for young, Nonviolent Offenders.
Deborah Sonagere December 8, 2022
The Neurobiology of Trauma. The Science Behind Trauma.
It is important to understand the neurobiology of trauma because it is important for people to understand how their brain effects their body. The University of Northern Colorado states that "the neurobiology of trauma--essentially the effects of trauma on the brain--is important to understand because it helps break down common misconceptions and victim-blaming about gender-based violence and it helps survivors to understand their experience and the aftermath in a new way" (University of Northern Colorado, 2022). Understanding the various ways in which trauma impacts the body allows people to victims to fully grasp their trauma, and can help guide them on their path of healing. Also understanding the ways in which the mind and body are connected may allow the victim to fully understand and comprehend their trauma. It allows them to understand why they may have acted/or not reacted the way they did in a situation. A substantial part of someone's trauma may stem from the way they acted during the traumatic event. Often times people can become so locked into what they did or did not during that time. By understanding the neurobiology of trauma it can be a huge stepping stone in the healing process for a trauma victim. "Decades of research into the neurobiology of trauma tells us that there are three responses humans (and many mammals) have to terrifying situations: fight, flight, AND freeze" (University of Northern Colorado, 2022). Copious amounts of research in Neurobiology has lead to the progression of trauma treatment and has had a significant impact on the field of psychology and the way that professionals conduct treatment.
Neurobiology plays a powerful role in ameliorating the impact of trauma. Understanding the neurobiology of trauma debunks and breaks down the myths from the facts in terms of trauma. It dismantles the common misconceptions that are often associated with trauma. It also breaks down stigmas that are often associated with individuals that suffer from trauma. Far too often stigma, rudeness and meanness from others is due to a lack of understanding. By teaching professionals working the world about the neurobiology behind trauma, as well as people out in the world, we might be able to dismantle myths and stigmatization surround trauma. Overall, understanding the various ways in which the mind effects the body is key in trauma treatment.
Sources:
University of Northern Colorado. (2022). Neurobiology of trauma. Retrieved Nov. 16, 2022.
University of Northern Colorado. (2022). Neurbiology of trauma: Dismantling common misconceptions and victim blaming statements about sexual violence. Retrieved Nov 16, 2022.
https://www.unco.edu/assault-survivors-advocacy-program/pdf/neurobio_trauma.pdf
Sexual Offenses & Treatment
When I first started working in the criminal justice system in Montana, I was convinced that I would never be able to work with offenders who have committed sexual offenses. I thought that I knew too many people who had been assaulted and had too many personal experiences and that it would be incredibly difficult for me to be able to work with those types of offenders and remain unbiased. While it is not an easy population to work with due to the varying types of offenses (some of which are incredibly difficulty to learn about), for the most part they are also some of the easiest due to the fact that most of the time they are going through some of the most intense treatment and because they usually are not treated very well at other facilities, so they tend to follow the rules a little more strictly. This is not to say that every type of sexual offender is like this, but I would say that the majority that I have worked with are.
Something that I find really interesting about sexual offenses is the amount of different things that an individual can do to end up with the label of “sex offender.” Anything from streaking at a football game or urinating in public to assaulting multiple people can get you the same label. While I agree that there should be consequences for all of these actions, I do not believe that someone who streaks at a football game should be treated the same as someone who has assaulted multiple people. In my eyes, those crimes are not the same and I think that treating them the same could do more harm than good. Research has shown that when you mix high risk offenders with low risk offenders, the low risk offenders increase their risk instead of high risk offenders lowering their risk. This applies across the board for all types of offenders. A lot of cases that I work with in Montana are statutory cases, meaning that the offender assaulted someone who was either below the age of consent (16 in Montana) or the offender was 18 at the time and the survivor was younger than that. Statutory cases are difficult because the circumstances vary, so even within those types of situations there is an incredible amount of difference from one crime to another. Currently, treatment includes groups sessions as well as individual sessions with an LCSW or similarly licensed counselor. There are workbooks and various assignments that offenders work through, but they are all covering the same material regardless of what their specific crime is. Implementing a blanket form of treatment for anyone isn't usually the best course of action, but especially with such differences in crimes, in my mind there is no way that each person is getting their needs met and their problem areas addressed.
I am in no way advocating for there to be no treatment or consequences for sexual offenses, I am instead advocating for there to be more treatment options and that we do a better job of considering the circumstances for the offense before just assigning blanket treatment. I understand that that takes more time as well as requires more staffing to accommodate more types of treatment, but I ultimately think that it would be beneficial to have a system more tailored to specific offenses and that allows for higher risk offenders to be separated from the lower risk ones.