CJ 720 Trauma & Crisis Intervention Blog
Images, Trauma, and Motherhood
Please note: This blog post reflects primarily my opinion about a topic I have wanted to discuss for quite some time. My writing does not reflect the entire picture, nor is it meant to reflect truth for all. Many experiences can look different. I would offer, however, that engaging with my post might offer some insight into a topic that is too often ignored or understudied in the academy today.
As many are painfully aware, trauma is not a one size fits all. It does not come neatly wrapped in something we can understand in its full magnitude. It is, however, a reality for so many people, if not most living in the world. From natural disasters to cycles of abuse in families, it permeates the bodies and experiences of those living in various situations. Though it does not just affect one population in the US, a few populations are more inclined to deal with constant and complex trauma than other groups. To name a few, those in marginalized groups, including women, poor people, people of color, and those with disabilities, are at the top of the list.
Though there are other populations, including veterans, EMTs, and police, as we have discussed in our course, these groups often experience trauma connected to their profession, not simply existing. Though trauma is trauma, the distinction I am making here is that a poor single caregiver is experiencing trauma by living in a society that values wealth and production. In contrast, the enlisted person chose to engage in what they knew could involve dangerous and violent situations. Neither of them deserves trauma by any means, but one is more based on a career path versus how the other is forced to live. I note this because I will be discussing a population experiencing trauma based on the color of their race and gender.
Since the transatlantic slave trade, Black mothers have watched their children be abused, assaulted, and harmed at the hands of predominantly white men. This is not a debatable assertion but rather a fact and reality. I mention this first because to discuss the topic of images, trauma, and motherhood; one must first understand this is not a new issue. However, it has not been centered and will be in the rest of my post. For many who have studied relatable issues, this has looked like trying to understand how these mothers respond to their black sons being abused or killed. This conversation is meaningful and has some research attached, so I will discuss Black mothers' relationships with their daughters.
Black women have to protect their daughters who share their faces, anatomy, and common experiences in a country deeply struggling with white supremacy and sexism. For Black mothers raising black daughters, the images of young women being assaulted, abused and slammed down by men is highly traumatizing. It is the constant reminder that not only do black girls and women have to deal with racism, but their anatomy somehow makes them a target for what folks might refer to as a double whammy.
Black mothers seeing the images of Breona Taylor, Sandra Bland, and the countless faceless women who experience sexual assault remind us that we live in a country that is not only okay with abuse and harm of black women but also causes harm. This is due to structural racism and sexism. They are constantly retraumatized by the images and respond as parents in ways that mirror that trauma, often in parenting styles. We find that Black mothers can be very strict with their daughters (almost to a fault) because they constantly fear losing their children. This can mean telling them to cover of their bodies, forcing them to be more mature than anyone around them, or training them to never be their fully vibrant selves in the face of any authority figures. These teachings take a toll on black young women's light; it dims it and often make them feel less powerful, worthy, and valued. Even as this is not the intent of black mothers, it is the protective response to trauma they do not want to be imposed on their daughters.
I believe that knowledge is power, so having media outlets offer stories about the experiences black women and their daughters are facing is important. However, the images do not help. Instead, it can be traumatizing and creates extreme fear in the bodies of black women, young and old. I am not saying these images should not be shown, but to have no support in place for black women is seemingly by design and further exacerbates the issues. It is an everyday nightmare for a black mother to see images of young women who are being harmed by individuals and systems. I would offer this is not by accident but rather as bold statements that the bodies of black women do not matter.
Harm toward black women should be stopped. It is imperative that as this continues, we must build out specific support tailored for black women. In essence, the issue needs to be studied and researched so models of support can be developed around the country.
My Journey with Art Therapy
With a history of anxiety, addiction, and depression on both sides of my family, my mother believed it was best for our family to start therapy when I was around the age of 7. At that time it was cognitive behavioral therapy. Sometimes I would play with toys and games while talking to my therapist and other times I would just sit on her couch for the whole session. At the age of 9 my father died unexpectedly of a heart attack. At that time my mother moved us to a center specific to families who are experiencing new grief. who have recently lost someone. I was added to a therapy group for children who lost a parent.
That time in my life following my father's death is so clear for me at some points and so hazy at others, which I have learned is my brain protecting me. I brought up the group therapy because we practiced art therapy every week, and I had not even realized that is what my grief therapy group was centered around until I started researching art therapy for this blog post. To the best of my memory the pieces of art I made were:
- a clay object to commemorate my father (I think it was in the shape of a heart...
- A mini flip book containing ten reasons I love my dad. Those are the only two pieces of art I remember vividly.
- A box with pictures I associated with my father on the lid, and important objects I associated with him in the box. I think we made the box to contain all the pieces of art we had made in our time at the center as well.
In researching for and writing this post I am able to realize the power of art therapy. I had been so skeptical of it when we began learning about different therapeutic approaches for people dealing with trauma. But, something clicked in my head and I realized that therapy group was so essential to my grieving process. Focusing on using art to celebrate the parents we had lost gave us the safety and comfort to open up to one another about our feelings and what we were going through emotionally. I think the perfect therapeutic combination for me at that time was art therapy and cognitive behavioral therapy. I am so grateful for this class for giving me the tools, materials, and space to realize this truth about my past. It may even inspire me to take up art therapy again.
Yoga and PTSD
Expanding on a previous discussion post I created, regarding one of the alternative approaches, yoga and mindfulness. Learning about the practice of yoga and its beneficial value to individuals mental health and other psychological stressors has intrigued me over the past few years. Growing up, I was taught the importance of movement and mindfulness but had not always fully appreciated its purpose. For example, my parents always turned to physical activity as a way to de-stress. Even my mom can recall from her childhood, as a pre-teen, going for runs throughout her neighborhood as a way to escape her parental/familial stressors. Interestingly enough, my mom carried this healing method into adulthood. She is now is a yoga and pilates teacher and personal trainer. She has used her training to not only benefit those within a vast range of ages and/or capabilities, but also to a unique group. She specialized in a practice of yoga for veterans in order to help treat/alleviate their symptoms of PTSD. As learned throughout this course and from reading The Body Keeps The Score, "ten weeks of yoga practice markedly reduced the PTSD symptoms of patients who had failed to respond to any medication or to any other treatment". It is amazing the power that yoga has on mindfulness, movement, creating a connection to ones own body that once seemed foreign to them, being present and in control, calming of the vagus nerve/amygdala, and much more. My mom, throughout my upbringing, has remarked on the benefits of sleep, deep breathing, mindfulness, and nutrition. She often utilized her breathing techniques when feeling nauseous and has also used it to teach me how to avoid fainting when I would be in claustrophobic environments.
In terms of veterans and PTSD, she aimed to provide support and teach them that their body is a safe place that they can trust because a lot of them may feel violated by their own bodies or closed off as a survival skill. She spoke about how important it was to acknowledge that sometimes they may need to leave the session because the class was too palpable and how important the language you use is. They may feel that their bodies have been violated. She aimed to teach them how to down regulate their nervous systems, connect them back to their senses in a way that does not overwhelm or overload their nervous stems, and more. I think, like my previous self, people hold misconceptions on yoga. They may view it as strictly a way to stretch or as not a proper work-out therefore pose the question as "why even bother?" or view meditation as boring. I think proposing more interventions/awareness around why yoga is so beneficial to ones mental health would help create awareness, a safe space for those struggling, or opportunity for those who were skeptical on its other purposes get a chance to explore it. There is now plenty of science to support the fact that nasal breathing, deep breathing, mindfulness, and movement allows the parasympathetic system to be activated or "re-registered". Mindfulness can help with this too, because "The basic premise of the practice was not only to notice the things that surround you, but also to pay attention, without judgment, to sensations that happen within the body, regardless of how painful they seem. This practice has been shown to help not only with reducing negative thinking and rumination, but also with rebuilding brain structures that are impacted in people who have survived trauma." (Rousseau, 2022) People who are suffering from PTSD need grounding, and yoga is a practice that IS grounding.
Rousseau, D. (2022). Module 4: Pathways to Recovery: Understanding Approaches to Trauma Treatment. Trauma and Crisis Intervention. MET CJ 720 02. Boston University Metropolitan College.
Van der Kolk: The Body Keeps the Score: Brain, Mind, and Body in the Healing of Trauma (Reprint ed.). Cloud reader - read.amazon.com. (n.d.). https://read.amazon.com/reader?asin=B00G3L1C2K&ref_=dbs_t_r_kcr
PTSD, Vicarious Trauma, and the Emergency Frontline
Whose Trauma Is It Anyway?
Vicarious Trauma
The term "vicarious trauma" entered the lexicon in the 90s with McCann and Pearlman's article in the Journal of Traumatic Stress, among other works. They observed that mental health professionals were being affected by their exposure to the trauma of their clients (McCann & Pearlman, 1990). The outlook of the therapist mutated as they immersed themselves in the torment of the client's past. Of the affected schemas they identified, Dependency/Trust was afflicted with mistrust of others, for the client had been betrayed by the adults entrusted with their wellbeing. Safety became suspect - how could anyone be safe in a world that allowed such cruelty? Power was not guaranteed, as it had been ripped from their client and replaced with helplessness. Independence, Esteem, Intimacy, Frame of Reference - the therapist’s very concept of the world around them was changed as their client’s trauma slipped around their professional boundaries and seeped into their psyche. Vicarious trauma manifests its toll on the mental health professional in ways very similar to post-traumatic disorder (PTSD) itself, including intrusive thoughts, numbness, sleep problems, and hypervigilance (Rousseau, 2022).
Arguably, vicarious trauma would be the diagnosis best fitting the emergency frontline healthcare worker (EFH) who suffers from similar symptoms. While “frontline healthcare worker” is used in the age of COVID to describe any caregiver who interacts directly with patients, EFH is used here to identify the members of the healthcare team who encounter a patient in vital first hours that decide if they go to the hospital floor, a detox, home, or the morgue. These include emergency medical technicians (EMTs) and paramedics, police and firefighters in some systems, emergency physicians and nurses, patient care technicians (PCTs), and consulting providers such as trauma surgeons and neurologists who come to the emergency department (ED) to help guide the intricacies of care in which they are experts. Research on the impact EFH’s work imparts upon them often uses the term “secondary traumatic stress” (STS) which can be considered synonymous with vicarious trauma but should be kept separate from “burnout” and “compassion fatigue,” which are sometimes used interchangeably but are better viewed as distinct but related processes (Hunsaker, 2015). Studies have investigated the prevalence of vicarious trauma in subsets of EFHs, particularly emergency nurses, and found that as many as 39% meet criteria and 75% experience at least one symptom (Ratrout & Hamdan; Mansour, 2019). Certainly there is value to looking at the prevalence of vicarious trauma across mental and physical health disciplines, but is the phenomenon experienced by EFHs truly the same as that seen in other settings? While the contributions of the inpatient team must not be minimized, on the hospital floors the screaming has stopped, perhaps because a breathing tube has been passed through the vocal cords and made screaming an impossibility. The bleeding has been controlled - for as the moribund often state, “all bleeding stops eventually” - and the soiled clothes have been removed. The patient is now a resident of the hospital, as if they were never a member of the community, never a being from the same world as the caregiver at the bedside. Hospital floors are the world of vicarious trauma, where the patient’s pain and terror are experienced via empathy and rapport. The patient’s home, the street, and the emergency department are their own arena and their own phenomenon.
Post-Traumatic Stress Disorder
When one is wrestling a woman whose arms and legs have been ripped off by a tractor trailer truck in order to control her delirious panic and save her life - is the trauma still vicarious? When tying someone to a bed and injecting them with sedating medications while they scream that the experience feels like when they were raped? The question was a point of some debate during the revisions that resulted in the DSM-V. Classically, the individual had to be the target of “actual or threatened death or serious injury, or a threat to the physical integrity of self or others” (APA, 2000). While EFWs are the frequent targets of threats, verbal abuse, and physical assaults, these direct traumas are a distinct entity from those experienced while treating a patient in extremis (Gates et al., 2006; Touriel et al., 2021). Further, the definition required that the subject’s response be one of “intense fear, helplessness, or horror” (APA, 2000). This response is exactly what EFHs train to overcome. The ability to takes swift and evidence-based action in a crisis and suppress fear, helplessness, and horror is at the core of what makes an EFH. DSM-IV included the qualifying experience of being “confronted with” trauma, which certainly occurs in the ED, but this fails to capture the actual interaction, whether it be the sensation of breaking ribs during CPR or of a hand that was squeezing so tightly but then goes limp. The EFH may become a courier of trauma, shuffling into a quiet room to confront a family with news of the “unexpected or violent death, serious harm, or threat of death or injury experienced by a family member or other close associate” - all additional DSM-IV criteria for a trauma such as one that might result in PTSD (APA, 2000).
Recognizing these experiences as trauma, the DSM-V expanded its definition to include “repeated or extreme exposure to aversive details of the traumatic event(s)” (APA, 2013). Surely then, the experience of the EFH has come to find its place in the scope of PTSD. Popular media would have us believe that the DSM has captured what it is to be an EFH surrounded by triggers for PTSD. In this world, the EFH walks into every shift with the knowledge that a bus full of hemophiliac toddlers will careen into a jagged glass factory after which terrorists will crash the MedEvac helicopter into the ambulance bay and take everyone hostage - all while a woman with ebola gives birth in a broken elevator as a colleague wonders if the child is his. But the ambulance and the ED are not Hollywood. The EFH trauma is exclusively failing lungs and sucking chest wounds. The ambulance is nearly guaranteed to pull up to a house in such a state of squalor that one wonders how a human being can have survived there. EMTs will respond to the alley where a person has fashioned their last possessions into a tent in which they may stay warm enough to survive the night while injecting the drug that has destroyed their life. An average shift in the ED will likely involve a quiet interview with a woman who can’t stop remembering the night she was raped or a man who, in the face of his brother’s recent death, has relapsed on heroin after eight years of abstinence. It may include telling someone that their persistent cough is due to lung cancer and the spots on their liver suggest it has already progressed past what modern medicine can remedy. Vicarious trauma is alive and well in the ambulance and the ED, as it is on the hospital floor or in the mental health professional’s office.
So vicarious trauma fails to incorporate the visceral experience and PTSD does not capture the empathetic burden of bearing witness. Where does this leave the emergency frontline? Perhaps with a term of their own...
Emergency Frontline Trauma
Where is the value in identifying this middle ground - this Emergency Frontline Trauma? The symptoms and treatments of vicarious trauma and PTSD overlap extensively. Is there any reason to distinguish the experience of the EFH or is this simply self-pity and self-importance? Well, like any illness the phenomenon can only be managed if it is specifically characterized and studied. If the experience of the therapist is different from that of the emergency nurse, then those conditions must be examined as the separate entities that they are. The person with a history of PTSD may have a single individual with whom they must come to some kind of peace or reconciliation but the physician may be unable to identify a single party who has caused her harm or damaged her sense of purpose. A mental health provider obtains a depth of understanding and familiarity with a client that an EFH could never match. Each entity possesses its unique qualities and warrants its own study so that caregivers weighed down by the past may thrive in the future.
Note: By virtue of being dedicated to the subject of trauma, this piece focuses on troubling aspects of emergency care. But as the endings of so many adventure novels and movies have celebrated, shadows are only cast in the presence of light. The work is a joy and a privilege. That realization alone is a weapon against the despair and emptiness of vicarious trauma and PTSD, if only one of many that must be employed to persevere on the difficult days and gloomy nights.
References
American Psychiatric Association. (2000). Diagnostic and statistical manual of mental disorders (4th ed., text rev.). Washington, DC: Author.
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC: Author.
Gates, D. M., Ross, C. S., & McQueen, L. (2006). Violence against emergency department workers. The Journal of emergency medicine, 31(3), 331–337. https://doi.org/10.1016/j.jemermed.2005.12.028
Hunsaker, S., Chen, H.C., Maughan, D., & Heaston, S. (2015). Factors that influence the development of compassion fatigue, burnout, and compassion satisfaction in emergency department nurses. Journal of Nursing Scholarship, 47(2), 186-194. http://dx.doi.org/10.1111/jnu.12122
McCann, I. L., & Pearlman, L. A. (1990). Vicarious traumatization: A framework for understanding the psychological effects of working with victims. Journal of Traumatic Stress, 3(1), 131–149. https://doi.org/10.1007/BF00975140
Ratrout, H. F., & Hamdan-Mansour, A. M. (2019). Secondary traumatic stress among emergency nurses: Prevalence, predictors, and consequences. International Journal of Nursing Practice, 26(1). https://doi.org/10.1111/ijn.12767
Rousseau, D. (2022). Module 1: Introduction to Trauma. [Boston University Course Materials]
Touriel, R., Dunne, R., Swor, R., & Kowalenko, T. (2021). A Pilot Study: Emergency Medical Services-Related Violence in the Out-of-Hospital Setting in Southeast Michigan. The Journal of emergency medicine, 60(4), 554–559. https://doi.org/10.1016/j.jemermed.2020.12.007
The Neurobiology of Trauma
I believe that addressing the neurobiological aspect of trauma is vital in understanding the negative effects of trauma. Firstly, trauma is a term used to describe the experience or circumstances that occur which in turn have a negative effect on an individual. This can be quite devastating as one would imagine. Some may experience trauma on a daily basis while others may not. Regardless of the number of occurrences, trauma remains distressing and taxing for all that experience it. How a person responds can vary person to person, they may be in denial of the situation, they may show symptoms of depression, anger, anxiety, etc. There is no one clear set of boxes that a person must check off in order to state that they’ve experienced trauma.
But what causes all of these symptoms to occur in the first place? There are various areas within the brain that tend to be the most affected by traumatic events. This includes the prefrontal cortex, amygdala, thalamus, and hippocampus. One of the issues that tends to come up when talking about trauma is how complex it is. Paul MacLean, a renowned physician and neuroscientist, explained the brain as being separated into three separate brains. Looking at his work can help us better explain trauma in terms of neurobiology. MacLean coined the term “triune brain”; which consisted of the reptilian brain, mammalian brain, and cerebral cortex. The reptilian brain includes the brain stem, cerebellum, and basal ganglia. This is where our autonomic nervous system comes into play, essentially holding all of our autopilot functioning like breathing, blood flow, etc. The mammalian brain is where one would find the thalamus, hypothalamus, amygdala and hippocampus. Otherwise known as the limbic system. This area of the brain is heavily involved in memory and responses. The limbic system connects with our reptilian brain to churn out an appropriate response. This connection is where our fight, flight, or freeze responses would occur. Then we have the cerebral cortex, this is where the right and left hemispheres, and the medial and dorsolateral prefrontal cortexes of the brain are located. These are the outermost layers of our brains, where our “higher-thinking” comes from. Things like intelligence, planning, organization, language processing/learning are all functions found within the cerebral cortex. Each of these “three brains” as outlined by MacLean are involved in how we respond to traumatic stimuli. 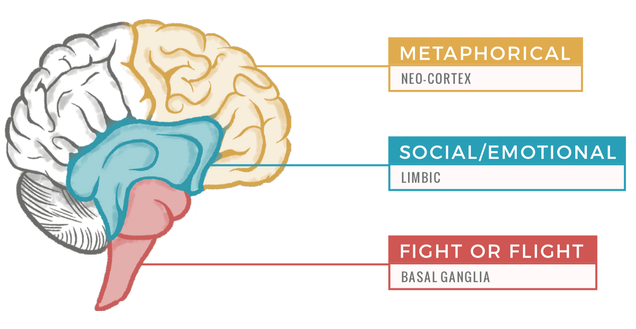
One major argument against this model is it focuses on a hierarchy of the brain. The idea being that the brain developed overtime as a result of evolution. Looking at the outline it would consist of the reptilian brain being developed first, then the mammalian brain and finally the cerebral cortex. Rather than the brain being triune, it has been suggested that it is adaptive and uses “adaptive prediction resulting from interdependent brain networks using interoception and exteroception to balance current needs, and the interconnections among homeostasis, allostasis, emotion, cognition, and strong social bonds in accomplishing adaptive goals” (Steffen et al., 2022). I do still believe that the triune brain model allows us to easily look at how the brain reacts to trauma and stressful situations. Which is why MacLean’s theory is still widely discussed today. Regardless of whether or not you believe in a more adaptive or triune layout of the brain, the information and things that are happening during stressful events remains the same.
I would also argue that if we were to use MacLean’s model to address a specific situation we would be able to do so in a way that was easily understandable to fellow listener’s. For example, let's say we live in a tropical climate like Florida, we’re halfway into a walk in the forest when we hear a rustle and see quick movement by our feet. Our brain perceives this event to be dangerous, there could be a snake nearby. The sensory information that we internalized, the noises and brief visuals were processed and sent to our thalamus and then relayed to the amygdala to rule out whether or not we were in a safe or unsafe situation. In our case it was deemed to be unsafe given prior knowledge of our surroundings. Due to our situation being seen as dangerous our hypothalamus then releases adrenaline and norepinephrine to trigger our fight, flight, or freeze response. Once that event occurs our cerebral cortex receives this information from the limbic system to create a memory based on the event. That way if another event similar to that one occurs the body will instantly flee, fight, or freeze. The information gets stuck. Sometimes this can be useful, like in this example where you would need to do something on the spot to avoid getting bit by a potential snake. On the other hand, this can also be detrimental to the individual in situations such as a Marine coming home after experiencing war trauma. Trying to integrate back into civilian life can be difficult when dealing with trauma related to war. Using this knowledge we can relate it back to real world situations to try and come up with solutions to address these negative effects.
Fortunately there are various options for therapy available to those who have experienced trauma. There is exposure therapy, EMDR, Yoga therapy, and much more. In having so many options available to address trauma, individuals are able to pick treatment best suited to their needs. Even within exposure therapy there are branches of different forms ranging from imaginal exposure, in vivo exposure, and flooding. The treatment that is ultimately chosen depends on the individual and what they’re comfortable with. What is very clear is that the neurobiology of the brain, what is happening behind the scenes, is equally as important and essential to understand.

Sources:
Rousseau, D. (2022). Module 3: Neurobiology of trauma. Retrieved from https://learn.bu.edu/bbcswebdav/courses/22sprgmetcj720_o2/course/module3/allpages.htm.
Steffen, P. R., Hedges, D., & Matheson, R. (2022, April 1). The brain is adaptive not triune: How the brain responds to threat, challenge, and change. Frontiers in psychiatry. Retrieved April 24, 2022, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9010774/
Burnouts among police officers
In Module 6, we've been presented an article, Routine work Environment Stress and PTSD Symptoms in Police Officers, that discussed the relationship between work environment and PTSD symptoms among police officers. The results showed that their work environment stress was most strongly associated with their PTSD symptoms and more specifically, variables such as gender and ethnicity resulted in having more negative social interaction and discrimination (Meguen et al., 2009). We further discussed the stigma surrounding police officers with mental illnesses and their concerns regards to requesting treatment due to fear of losing their jobs, having their license to carry a firearm taken away, being reassigned to a less stressful position, or being ridiculed by their peers and being seen as weak. While offering all the necessary resources to help better their mental health is crucial, being able to recognize the underlying cause to their problems is also important. Behind every police officer is a husband, a wife, a father, a mother, a friend, a coworker, and most importantly a human being. These qualities are often overlooked because of their heroic actions in the community, and places so much pressure on them to be the "hero." What we don't see is the emotional and physical exhaustion from responding to countless calls where they are expected to make split second decisions under pressure.
Most police officers, male and female, reported that the most frequent stressor was responding to violent family disputes, and the most highly rated stressor was being exposed to battered children. Though infrequent, another most highly rated stressors were killing someone in the line of duty and experiencing a fellow officer being killed. Male officers reported court appearances off duty and working second jobs as stressors while female officers reported experiencing lack of support from supervisors as a stressor (Violanti et al., 2016).
Reducing the amount of incidents that act as stressors may be impossible, but reducing the amount of time and workload police officers is exposed to stressful situations is more practical. Offering debriefings like CISM and overall organizational support is important for officers as it would help them deal with traumatic events that unfortunately comes with the occupation. On the other hand, reports of female officers feeling under-supported by their superiors reiterates how even though we are seeing an increase in female officers across police departments, some organizations are still having issues of discrimination. For that reason, there needs to be more training and education providing statistics and evidence on the positive aspects of women in policing. Overall, without addressing these stressors, more police officers will experience burnouts and significant mental health deterioration leading to depression and suicide.
Maguen, Metzler, T. J., McCaslin, S. E., Inslicht, S. S., Henn-Haase, C., Neylan, T. C., & Marmar, C. R. (2009). Routine Work Environment Stress and PTSD Symptoms in Police Officers. The Journal of Nervous and Mental Disease, 197(10), 754–760. https://doi.org/10.1097/NMD.0b013e3181b975f8
Violanti, Fekedulegn, D., Hartley, T. A., Charles, L. E., Andrew, M. E., Ma, C. C., & Burchfiel, C. M. (2016). Highly Rated and most Frequent Stressors among Police Officers: Gender Differences. American Journal of Criminal Justice, 41(4), 645–662. https://doi.org/10.1007/s12103-016-9342-x
Yoga is Beneficial for inmates with PTSD
I will be talking about how successful yoga is as a treatment for people in prison with PTSD. Yoga also will help the inmates when they get out of prison. Prisoners see a lot of things during their time in prison. They witness different types of violence such as murder, suicide, rape, etc. Sometimes they may not actually see it with their own eyes, but they hear about it in detail. That can still be traumatizing. Juveniles and mothers may have face also of different traumatic events before entering prison. During their time in prison, the goal should be to help them deal with trauma day to day. This will help become a better person for when they are release. As I have mentioned in my post, yoga is used for pain management and for people with a variety of psychological diagnoses. The type of yoga that was talked about this week is trauma- informed yoga which helps with stress safety, predictability, structure, and repetition. The yoga poses in this type is to focus on their breathing and embodiment. So, in other words they are taking over their mind and body. (Rousseau,2022) Yoga is starting to more recognized in prisons. It is understood that yoga will not fit all problems for incarcerated people, but it is a start and is said to play a major role.
As I have mentioned in a few of my post throughout the semester, my uncle was recently released from prison. He joined the yoga program in his correction facility. He is currently 63 years old so you would not think an elderly black man would be in a yoga class. He told me he really enjoyed it and it helped with his pain and anger. He has been diagnosis with PTSD, and I see him do yoga in his room 3 times a day. I can say that I have seen a big change in him since he has first joined yoga. My family use to call and check on his mental health all the time so hearing and now seeing the improvement yoga has had on him is very good. When COVID hit the USA, yoga classes in prisons were suspended. As far as I know, yoga classes are not being held still but some inmates still practice some of the yoga techniques and share with other inmates that did not get a chance to go. My uncle told me once the state allowed prisons to go outside again in groups and to common area sometimes, there would be some people off to the side doing yoga. Yoga has a major impact on these inmates.
In an article I read about a yoga program at York Correctional Institution in East Lyme, CT, a 41-year-old inmate would usually cut herself to deal with anxiety, depression, and PTSD. It was her way to forgive herself. Now after graduating the program, the marks are barely noticeable. The yoga program in York Correctional Institution is a little different from other in Connecticut. This program is a 200-hour course that will allow inmates to become certified yoga teachers. They are allowed to teacher yoga after they are release. This gives an opportunity to find a job they will like and still help with their mental health while they teach others. Deputy Warden Senerth said, "There's evidence it really works with people who are victims of trauma. You have that fight or flight reaction. It helps them to just regulate and be in that moment." (Florin,2017) I believe all prisons should have yoga programs like this. Yoga is always gaining control of your mind and body.
Reference:
Florin, K. (2017, January 15). Yoga spreading mindfulness inside Niantic Prison. The Day. Retrieved April 2022, from https://www.theday.com/article/20170114/NWS04/170119588
Rousseau, D. (2022). Module 4: Pathways to Recovery: Understanding Approaches to Trauma Treatment. Trauma and Crisis Intervention. MET CJ 720 02. Boston University Metropolitan College.
Art Therapy: Why It Helps With Trauma Healing
It’s surprising how one art therapy course can reshape the way you view introspection and healing. Yet, in my first year of college, I found myself in that same position. As someone who was going through crippling social anxiety and depression at the time, I found myself needing the art therapy course I took.
It started with a singing bowl, a special bowl that creates a calming ringing sound when played. This was always used to help us center ourselves and start a rather meditative art-creating process. In the one hour of the class, we got to first hand try out therapy techniques for ourselves through different art mediums. We were then encouraged to draw what came to mind.
Even without meaning to, my hand found itself drawing my innermost thoughts, desires, and hurts. When it was time to look at what I made and talk about it, I found that what I had created was an abstract version of what I failed to verbalize. Yet, after drawing, and saying what was troubling, it became easier to vocalize and heal from.
When it comes to healing from trauma, there are many methods that can be used, but the goal is essentially the same: to reclaim a connection with the body and teach the mind that they are not in as dangerous of a situation as they instinctually feel they are in. Some methods include yoga, massages, meditation, and sports. In this case, I learned that healing can come from art.
Yes, but to what extent? First-handedly, I experienced that art therapy is capable of helping people with depression or with anxiety like myself, but it is also helpful for other mental illnesses. Studies have shown that veterans with PTSD have benefited from art therapy treatment.
This is primarily because some traumatic memories are stored non-verbally and can be retrieved by recollections of sensory and kinesthetic elements.
Sometimes, it is difficult to express how you feel in words especially if you are still processing it. In some cases, victims of trauma with PTSD will cope by shutting down the areas in their brain that transmit emotions to define their terror. Yet, this is crucial because if you cannot define your trauma, then it is hard to heal from it. Art creates an avenue for patients to open up in a way that cannot be expressed with words. Sometimes, verbalization is difficult, but art creates a way to start with something smaller, like color or line.
In a study done by Melissa Campbell, 11 veterans received 8 sessions of art therapy. All participants showed improvement in their symptoms. By the end of the 8 session course, they were able to focus on themselves before and after the trauma. While they drew, blocked memories resurfaced, or crucial realizations were made about how they could further their healing process.
It’s amazing what Campbell was able to do in 8 sessions. With more art therapy, a person with PTSD may even be able to use art as a healthy outlet to process and cope with the stimulation of the outside world.
Sometimes, it’s easy to believe that the arts don’t have power because they don’t show concrete results like a bandaid over a cut, but it helps to exercise the right side of your brain.
If you have PTSD, or like me, were dealing with depression and anxiety, I would encourage you to enroll in some art therapy classes. Art therapy is a great way to get yourself to reflect especially if, like the veterans, some of your trauma is stored nonverbally. If those are too expensive, turn on a singing bowl sound on youtube, center your mind and begin the process of drawing. When you’re done don’t forget to evaluate your drawing too!
By: Olivia Kim
References:
Campbell, M., Decker, K. P., Kruk, K., & Deaver, S. P. (2016). Art therapy and cognitive processing therapy for combat-related PTSD: A randomized controlled trial. Art therapy : journal of the American Art Therapy Association. Retrieved April 6, 2022, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5764181/#:~:text=Art%20therapy%20provides%20a%20safe,Morgan%20%26%20Johnson%2C%201995).
Complementary and Alternative Medicine Approaches to Trauma
Complementary and Alternative Medicine (CAM) approaches to trauma treatment and prevention are treatment plans outside the realm of clinical approaches. These may include yoga, mediation, acupuncture, homeopathy, oriental medicine, massage therapy, herbal medicine, electromagnetic therapy, hypnosis, art therapy such as dance and music, among so many more. (Johns Hopkins Medicine). These forms of treatment are creative ways of healing trauma without the use of prescription medicine.
"Through the years, a significant amount of progress has been made with nontraditional approaches to trauma treatment. Some of the most researched and supported methods include yoga and mindfulness, but they are not the only options available for people who experience symptoms of PTSD." (Rousseau, Module 4).
I want to talk about how meditation is used to improve PTSD symptoms. According to an article by Healthline, "meditation is a practice that can help you focus your mind and gain greater awareness of yourself, thoughts and inner experience, surroundings, and moment-to-moment needs." There are different kinds of mediations, and some might help reduce stress-induced trauma and PTSD symptoms more than others. One of the leading meditation forms is called "mindfulness". According to Healthline, "mindfulness refers to a state of mind where you can acknowledge your thoughts, feelings, and bodily sensations without judgment." This form of meditation helps one become more aware of the present moment, while staying safe and grounded while recalling past experiences or memories.
According to Module 4 of the course materials, Mindfulness refers to "the unprejudiced noticing of physical and emotional experiences, designed to enhance clarity and reduce rumination and self-critiquing." In both definitions, the key word would be "without judgment" and "self-critiquing". It is important to realize that you are engaging in mindfulness to not only heal, but to remember that your experiences do not define you.
CAM approaches are not for everyone, just like traditional treatment options are not. Finding what works for you is all apart of your own journey to healing. The process is ongoing, but it is important to know that there are many options available to you, all you have to do is choose.

References:
Rousseau, D. (2022). Module 4: Pathways to recovery: Understanding approaches to trauma treatment. https://learn.bu.edu/bbcswebdav/courses/22sprgmetcj720_o2/course/module4/allpages.htm
Swaim, E. (2022, April 20). Can meditation help ease PTSD symptoms? Healthline. Retrieved April 21, 2022, from https://www.healthline.com/health/ptsd-medita
Types of complementary and alternative medicine. Johns Hopkins Medicine. (n.d.). Retrieved April 21, 2022, from https://www.hopkinsmedicine.org/health/wellness-and-prevention/types-of-complementary-and-alternative-medicine
Service dogs can help people who have PTSD
Posttraumatic Stress Disorder (PTSD) is a serious problem in the US, according to the "What is Posttraumatic Stress Disorder (PTSD)?" written by American Psychiatry Association, "PTSD affects approximately 3.5 percent of U.S. adults every year, and an estimated one in 11 people will be diagnosed with PTSD in their lifetime. Women are twice as likely as men to have PTSD." (APA) We can see that PTSD affects so many people, therefore, service dogs are a way to help the people who have PTSD. Service dogs can be soothing the PTSD emotional and physical problems, let's talk about how can service dogs can help people.
First, we know that some PTSD patients cannot take care of themselves and cannot perform tasks that will keep them safe(Rousseau, D, 2022). Therefore, we need to have Psychiatric service dogs, the service dogs are trained to help the patients in their life, for example, "find a person or place, conduct a room search, signal for certain sounds, interrupt and redirect, assist with balance, bring help, bring medication in an emergency, clear an airway, and identify hallucinations. (Rousseau, D, 2022)"
Also, the service dog can help the patient emotionally because the service dog can stay with you and support you when you feel sad and lonely. Most people who have PTSD also will have some psychiatric problems like depression, anxiety, service dogs can help them to relax and service dogs can know that the patients have the symptoms of anxiety, when its know, it will try nudging, pawing, or licking the handler till the patients calm down (6 WAYS SERVICE DOGS HELP PEOPLE WITH PTSD, 2020).
Finally, service dogs can be a reminder of the patients, for example, they can remind the patients that is time to take their medicine and remind them of routine tasks such as eating and sleeping (6 WAYS SERVICE DOGS HELP PEOPLE WITH PTSD, 2020).
However, the service dogs have some weak parts, and that is service dogs cannot cure PTSD, and they just can get simple support before, during, and after the trigger(Rousseau, D, 2022). In my opinion, I think that even though service dogs cannot cure PTSD, they also support the patients a lot when the patients need help. Service dogs can be soothing the PTSD emotional and physical problems, when the patients who in danger, they also will help them to solve the problems.
I think that dogs can help us to relax and my dog lets me know that she will stay with me when I need help. I really love my dog because she helped me across the most difficult experience in my life. On the other hand, I also think that not only dogs can help us to calm down, but also cats or horses can help us to solve the problem.
References Material
American Psychiatry Association. (n.d.). What is posttraumatic stress disorder (PTSD)? Psychiatry.org - What is Posttraumatic Stress Disorder (PTSD)? Retrieved April 20, 2022, from https://www.psychiatry.org/patients-families/ptsd/what-is-ptsd#section_10
Jimenez, J. (2020, December 4). 6 WAYS SERVICE DOGS HELP PEOPLE WITH PTSD. New Life K9s Service Dogs. Retrieved April 20, 2022, from https://www.newlifek9s.org/news-events/blog/service-dog-blog.html/article/2020/12/24/6-ways-service-dogs-help-people-with-ptsd
Rousseau, D. (2022). Module 4: Pathways to recovery: Understanding approaches to trauma treatment. Blackboard, https://onlinecampus.bu.edu/bbcswebdav/pid-9960461-dt-content-rid-63971458_1/courses/22sprgmetcj720_o2/course/module4/allpages.htm