Home
Self-care is Important in our Busy Life!!
I think that mental health is important for anyone and it will affect our emotions, actions, thinking, making a choice, and relation to other (NIMH, 2022). Self-care is the best way for me to decrease pressure and relax because we are graduate students and some of us might work and study at the same time. According to the National Institute of Mental Health, if we spent some time in self-care, we can improve our physical and mental health. On the other hand, some self-care methods do not need too much time and also can let people relax and calm down.
I have some experience to decrease pressure based on self-care. When I was 16 years old, I came to the US to study. At that time, my English is very poor, and it is difficult to communicate with someone. I feel stressed and nervous, I always cried at night. Since I came to the US by myself only, no one can help me or support me. Assignments, essays, grammar, and speaking are the worst part of my learning. I tried some types of self-care to help me cross this challenge at that time, for example, physical self-care, recreational self-care, and social self-care (Beard, 2022).
First, physical self-care is a good way to let me decrease my pressure because at that time I went to play rugby at school, and as we know that tackle is the way to defend the competitor. At that time, if I can tackle one competitor really hard, it let me feel more confident, and I know that no matter how hard the assignments or essays are, I also can do it. NIMH (2022) mentions that small amounts of exercise also can let people boost their mood and improve their health.
Second, recreational self-care is the way that I really like because I do not need to do anything and just relax. Watching some TV shows or movies is a way that enjoys our life because when you focus on the movie, you won't think about anything about stress. Also, I like playing computer games to create my own world and build some houses, and adventure in the game. Next, having a pet also is a way to self-care because research proves that having a pet can "provide a huge boon to lonely individuals, pets can be a serious mood lifter, even if you’re not experiencing feelings of isolation (Drewis, 2017)".
Third, social self-care is my favorite way to relax because I really missed my friends and parents when I studied in the US. I almost called my parents every day to talk about what I experienced at that time and asked them for some advice about sometimes I feel stressed about and what should I do. On the other hand, I also hung out with my friends whom I met in the US, and we went to eat sushi, and play bowling. keep in touch with parents and friends can provide emotional support and practical help (NIMH, 2022).
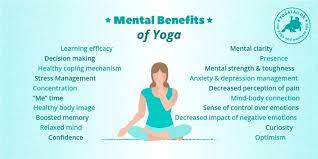
Even though this course wants the student can have a better understanding of forensic psychology, however, self-care also can help people who have trauma. Like service dogs for a veteran that has PTSD, or people who have panic disorders, anxiety disorders, major depression, or autism spectrum disorders (DAV, 2022) because service dog can help people to become positive and good for their emotional health (Rousseau, 2022). On the other hand, Yoga also is a good self-care for people who have trauma. Rousseau (2022) and Fenneld (2023) also mention in different resources that yoga can effectively help our brain and muscle relaxation, and can help us to slow down.


Reference Material
Beard, C. (2022). The 7 Pillars of Self-Care and How to Use Them. The Blissful Mind. Retrieved February 20, 2023, from https://theblissfulmind.com/pillars-of-self-care/.
Drewis, D. (2017, October 5). Why having a pet is officially the best ever form of self-care. Collective Hub. Retrieved February 25, 2023, from https://collectivehub.com/2017/10/why-having-a-pet-is-officially-the-best-ever-form-of-self-care/
DAV. (2022, December 5). Service animals. Retrieved February 26, 2023, from https://www.dav.org/get-help-now/veteran-topics-resources/service-animals/
Fenneld. (2023, January 16). What is trauma-informed yoga? . Cleveland Clinic. Retrieved February 26, 2023, from https://health.clevelandclinic.org/trauma-informed-yoga/
Rousseau, D (2022). Lecture note, Trauma, and Crisis Intervention
U.S. Department of Health and Human Services. (2022). Caring for your mental health. National Institute of Mental Health. Retrieved August 14, 2022, from https://www.nimh.nih.gov/health/topics/caring-for-your-mental-health
Trauma in Incarcerated Inmates.
Kayla Antolik
February 24th, 2022
MET CJ 752 O1 Forensic Behavior Analysis.
Blog Post.
For my blog post, I am going to be touching base regarding trauma in incarcerated inmates. One of the important things regarding my training when becoming a Sheriff Technician for the jail was, we are told to have professional and respectful relationships with the inmates. Just because they committed crimes that are unforgivable does not mean they are any less of human. While we may have our own prejudice and implicit bias feelings regarding criminals, we should also know in this field that we are not only serving the public, but also to the inmates as well. From my time here I have spent my first week of training building a relationship with the inmates. I’ve found that respect goes a long way in not getting into it with an inmate if they mouth off, as everything they say should not be taken personally and let it roll off your back. For example, while most Technicians can become frustrated with an inmate’s attitude, if I am still in the wrong and they are calling me all sorts of names. I will continue with my apology if I prematurely turn off the TV’s when locking down, due to still being new and finding out the routine for the housing unit.
Additionally, inmates’ experiences other forms of trauma just like outside from sexual abuse, assaults, fighting with their cell mate. Our institution has what is called a ‘consent decree’ which ensures that inmates are treated humanely from pod time, yard time, additional resources such as classes, counseling, medical treatment, and court assistance. However, there can be situations which an inmate may not be able to participate in, such as if they are out to court, they do not receive recreational time in the pod, and can miss out on being out. So, this can potentially create an issue, as well with video calls/visits for if the visit/call/court appointment goes terribly where it can affect an inmate’s mental health for not being able to go outside after their appointments.
Such as for example, an inmate who comes back from court must be stripped down and are held in a multi-purpose room where all the inmates are able to mingle while being searched. This can create shame, or embarrassment due to being stripped searched in front of others. For an inmate who may have experience sexual assault/abuse in their life this could potentially lead to them being retraumatized or feeling ‘violated’ even though this is for our policies and procedures to ensure safety towards staff and inmates. I think it would be beneficial to at least be more cognizant of the inmates to prevent revictimization for them if there is a more private manner to do searches and that of the same sex. So female, strip searching female, and male strip-searching males.
Classes and programs that we provide to improve recidivism rates and prepare inmates for release. These classes are classes that could provide them with the tools and skills they need in search for work, anger management, counseling services for mental health in healthier ways to cope, or information for behavioral health inmates to utilize and explain what is available to them as they may not know the number of resources at their fingertips.
Other trauma’s that inmates can experience in the jail can be experiencing an overdose and being brought back from Narcan. Experiencing their cell mate committing suicide, or discovery of their cell mate, including overdose deaths. While they may not have experienced the following trauma’s each situation is unique as the criminals can be revictimized from childhood wounds or traumas in the past, to their experiences in the prison system as well. This all comes down to their triggers, how they function as an individual with trauma, coping, and dealing with stress, as each person is unique so something that may not be as traumatic for one person, it doesn’t say others would have a more enhanced emotion as it’s something that triggers them in different ways. Not each situation is the same, but there are a lot of what we can learn from the differences with criminal behavior, and forensic behavior analysis regarding the mentally ill, psychopaths, and criminals.
Mental Health and Crime: The Issue of Misdiagnosis and Overdiagnosis
Emily Larsen
Mental Health and Crime: The Issue of Overdiagnosis and Misdiagnosis.
February 24, 2023
Mental health and crime are complex issues that are often interconnected. One issue that arises is the potential for overdiagnosis and misdiagnosis of mental health conditions in the criminal justice system. Overdiagnosis occurs when a mental health condition is diagnosed when it may not be present or when the diagnosis is too broad and not specific enough (Morrison, 2016). Misdiagnosis occurs when a mental health condition is diagnosed incorrectly, leading to improper treatment or inappropriate consequences (Morrison, 2016). Overdiagnosis and misdiagnosis can have serious consequences for individuals involved in the criminal justice system.
For example, if someone is incorrectly diagnosed with a mental health condition, they may be prescribed medication or treatment that is unnecessary or potentially harmful. If under the wrong treatment plan it could impact an individual's perception of reality and actions (Rousseau, 2023). Alternatively, if someone with a mental health condition is not properly diagnosed, they may not receive the treatment they need, leading to further negative consequences. With the criminal justice population, trauma is another factor that can go hand in hand. Research has found that approximately 75% of incarcerated adults report histories of trauma exposure (Fretz, 2023). That is statistically significant, with more than half of the incarcerated population having connections to trauma. Not only does this population have major connections with trauma, and mental health but also can have influencing factors of substance abuse. In the United States, those who have suffered from addiction and committed crimes relating to drugs or alcohol have made up 85% of the prison population (Rousseau, 2023). There are so many factors that contribute to who an individual is. The criminal justice population is more susceptible to crime with different influencing risk factors, which is why it is so important that they receive the right diagnosis.
There are several factors that contribute to overdiagnosis and misdiagnosis in the criminal justice system. One issue is the lack of training and expertise among some professionals in the criminal justice system, such as police officers or judges, in recognizing and diagnosing mental health conditions. Another issue is the stigma surrounding mental health, which can lead to biases and stereotypes that influence diagnoses (Rousseau, 2023). Additionally, the pressure to quickly resolve cases in the criminal justice system can also lead to hasty diagnoses and inaccurate conclusions (Morrison, 2023).
To address the issue of overdiagnosis and misdiagnosis in mental health and crime, it is important to increase education and training for professionals in the criminal justice system. This could include providing specialized training for police officers, judges, and other professionals in recognizing and responding to mental health conditions. Additionally, reducing the stigma surrounding mental health and improving access to mental health care could also help to address this issue. Finally, it is important to ensure that mental health diagnoses are based on sound evidence and not influenced by biases or stereotypes.
References
Morrison, M. (2016). Overdiagnosis, medicalization and social justice. Journal of Medical Ethics. 42 (705-714). Retrieved from; http://dx.doi.org/10.1136/medethics-2016-103717
Fretz, R. (2023). What is the impact of trauma in the criminal justice population?. MHS Assessments: Public Safety. Retrieved from; What is the impact of trauma in the criminal justice population? - MHS Assessments
Rousseau, D. (2023). Modules 1-6. Boston University.
Self-Care Practices
Self-care is extremely important for everybody to engage in. It is even more important for those who experience or have experienced trauma. Those healing from traumatic events and are going through the trauma healing process, should practice self-care and listen to their bodies. According to Dr. Hood, “if you truly want to overcome your trauma, you must face your feelings and practice self-care” (2018). Being able to let yourself feel and learning how to level out different feelings with self-care is crucial. However, self-care is not one specific act, or even a combination of certain acts. Self-care looks different for every individual.
Self-care acts can be broken down into seven pillars (Beard, 2022). These seven pillars work together to paint a complete picture. The seven pillars, according to Beard, include: mental, emotional, physical, environmental, spiritual, recreational and social (2022). What is important when practicing self-care is being aware of the seven different pillars and seeing what area needs focusing on. With those healing from traumatic events, it could be just an emotional focus of self-care and letting yourself feel the feelings or it could be a combination of a few of the pillars, such as mental, emotional and physical. Whatever it may be, self-care is essential for healing and dealing with trauma.
Below are ideas of self-care that fall into each pillar.
Mental:
- Journaling
- Meditation
- Intentional breaks from technology/social media
Emotional:
- Listening to music
- Watching a movie that makes you feel
- Setting boundaries
- Affirmations
Physical:
- Working out
- Eating healthy meals
- Drinking more water
- Taking vitamins
Environmental:
- Cleaning and resetting your space
- Exploring somewhere new
Spiritual:
- Connecting to a higher power
- Volunteering for something you believe in
Recreational:
- Engaging in hobbies
- Playing games, such as board or video games
Social:
- Spending time with family and friends
- Texting or calling a family member or a friend
- Joining a group
References:
Beard, C. (2022). The 7 Pillars of Self-Care and How to Use Them. The Blissful Mind. Retrieved February 20, 2023, from https://theblissfulmind.com/pillars-of-self-care/.
Hood, J. (2022). The Importance of Self-Care After Trauma. Highland Springs Specialty Clinic. Retrieved February 20, 2023, from https://highlandspringsclinic.org/the-importance-of-self-care-after-trauma/#:~:text=During%20the%20trauma%20healing%20process,to%20during%20this%20healing%20process.
ADHD, Assessments, and The Criminal Justice System
According to Skowyra et al., (2007), “seventy percent of youth in juvenile justice systems have at least one mental health condition and at least 20 percent live with a severe mental illness" (p. vii). According to the U.S. Surgeon General Report, “10% of children and adolescents in the United States suffer from serious emotional and mental disorders that cause significant functional impairment in their day-to-day lives at home, in school, and with peers” (Rousseau, Module 2, 2023). This means the likelihood is high that youth in the juvenile justice system struggle in both school and vocational planning, significantly impacting their future. One reason this may occur is that “norms for vocational inventories and assessments have not been established that consider minority groups" (Dipeolu et al, 2019). One minority group that this affects are individuals with attention deficit hyperactivity disorder (ADHD).
ADHD is a neurodevelopmental disorder with which symptoms can cause clinically significant distress or impairment in school and occupational functioning (DSM, 2013). This is also shown to influence criminal behavior. According to Bartol et al., (2021) approximately one-fourth of children diagnosed with ADHD “engage in serious antisocial behavior during childhood and adolescence and criminal behavior as adults” (p. 53). Within correctional facilities, “the prevalence rate for ADHD at 3 to 10 times higher than are found in the general population” (Bartol et al., 2021, p. 54). With ADHD considered a “puzzling problem (Bartol et al., 2020, p.53) it is often misunderstood. For forensic psychologists to provide effective support and guidance when working with juveniles and adults in the criminal justice system with ADHD, ADHD must be well understood.
Research has shown that inventories based on norms from the majority that are used to assess personality and behavior characteristics along with career paths in individuals with ADHD are ineffective (Dipeolu et al., 2015, Royal et al., 2015). With that, it is important for a forensic psychologist to be able to identify the common characteristics of ADHD. Being well versed in common thought and behavior patterns of someone with ADHD is important to consider to ensure that what is being asked within an inventory and assessment is being interpreted and measured accurately. If we are not doing this, how can we assume results to be accurate for those with ADHD if the inventories used are based on majority norms?
Administering assessments and inventories to a minority group, designed with norms established by a majority within the criminal justice system may be impacting the effectiveness of treatment. In the words of Dr. Rousseau, “without treatment, the consequences of mental illness for the individual and society are staggering” (Rousseau, Module 2, 2023).
For more information on ADHD please check out:
References:
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th edition). Washington, DC
Bartol, C. R., & Bartol, A. M. (2021). Criminal behavior: a psychological approach (12th ed.). Pearson.
Dipeolu, A., Deutch, S., Hargrave, S., & Storlie, C. A. (2019). Developmentally Relevant Career Constructs: Response Patterns of Youth with ADHD and LDs. Canadian Journal of Career Development, 18(1), 45-55.
Dipeolu, A., Hargrave, S., & Storlie, C. A. (2015). Enhancing ADHD and LD diagnostic accuracy using career instruments. Journal of Career Development, 42(1), 19-32.
Rousseau, D. (2023). Module 2. Boston University.
Royal, C., Wade, W., & Nickel, H. (2015). Career development and vocational behavior of adults with attention-deficit/hyperactivity disorder [ADHD]. Career Planning & Adult Development Journal, 31(4), 54-63.
Skowyra, K. R., & Cocozza, J. J. (2007). Blueprint for change: A comprehensive model for the identification and treatment of youth with mental health needs in contact with the juvenile justice system. Policy Research Associates, Inc.
self care post
Since I have had multiple classes with Professor Rousseau in the past I have decided to explain my approaches to self care using both information from previous classes as well as pieces of my previous blog (since this is still a part of my self care routine) but recently I have also found another avenue to self care that allows me to take a step back from my life and almost live in someone else’s.
Reflecting on my previous blog post, I have learned to use yoga as a self care and wellness activity. As an athlete, I have always been taught that if you are not pushing yourself, or getting better everyday that you work out that that work out is all but useless, and this a mindset that many athletes regardless of age have, and it is one that is untrue and very damaging to both mental and physical health. So instead, I have turned to yoga as well to become more in tune with my body and mind, as well as still “pushing” myself just in a different manner. Through the different styles of yoga I am able to choose on a day to day basis what my mind and body need. Do I feel overwhelmed and need more of a meditation yoga, am I tight/sore and tired and need more of a Yin yoga where I hold a couple of different positions for an extended period of time, or do I have the energy to really push and challenge myself where I aim for more of a strength building yoga? Below I have included an excerpt from my previous post about how yoga has helped me personally and also how it can help people who have experienced trauma:
“when I can finally hold a pose or a certain muscle that has been tight all week finally relaxed through my yoga movements it is a relief and also gives me a sense of pride as I have been able to accomplish what many from the outside see as a simple task but to me it takes the discipline of both my mind and body working together to do it. I also think that yoga, or any workout routine can also assist in the treatment of trauma. As we’ve mentioned in both lecture and posts throughout the semester, people who are mentally suffering are often unable to lead goal driven lives, they are too focused on the now. So these workout routines not only require forethought and planning by the individual but also creates easily understandable goals, such as holding a pose for a certain amount of time or gaining the flexibility to even be in a certain pose at all.”
However, at first yoga may be frustrating to many people (at first to me it was) it can take time to be able to appreciate all if its benefits. For some people however, the intimacy of yoga can be overwhelming and triggering for some people who have experienced a trauma; “
“intimate actions in yoga, such as the happy baby pose, can be triggering for some individuals, the idea of mimicking of movements that occurred during their traumatic experiences [or feeling the touch of an instructor] causes many to freeze. It is not until individuals can learn to breathe, push through, and maintain this pose or the physical touch of an instructor that they can “let go” or feel the relief of a deep breath and begin to relax.”
As I mentioned before, while I still practice yoga and other forms of wellness, I have also recently (re)discovered the power of immersing yourself in a good book. Coming back to classes this semester after having a few weeks off from school and being able to spend 4 days at home for Christmas (which is the most I’ve been able to do since high school) made me so relaxed and content but I also dreaded coming back to classes. Since I had worked and taken classes through summers and over breaks for the past few years, this winter break was my first time since winter break of my sophomore year that I had not been in classes, and I realized how nice it was to have absolutely nothing to worry about academically for 6 weeks. So, when classes started again a few weeks ago I was trying to find a new way to keep busy and relieve stress without putting extra strain on my mind or body (as most of my other self-care actions usually do). So, I decided to try and read more, while I read occasionally I usually only did it for pleasure when I was sitting on a beach or traveling on a plane and there was not much else for me to do. But now, having taken some book recommendations from my friends, I spend hours almost every day reading. I will start a book and finish it a day. I become so removed from my reality and feel as if I am in another person for a short period of time that it gives me a break from having to worry about the small things in my life, I may make bigger in my own head than they are. And while I would never suggest that avoiding life problems is the best way to deal with any of them, it does allow me to step back and take a breath.
Both self-care activities are things that I think could also be beneficial to those who work in a field that is related to trauma. It allows for a break in the harsh reality that some people may be facing in the form of a book or meditation, and it also promotes healthy mind/body connection as well as planning and goal orientation in the form of yoga.
Van der Kolk, Bessel . The Body Keeps the Score. Penguin Publishing Group. Kindle Edition
Rousseau, Danielle, Lecture, Trauma and Crisis Intervention, 2022
Rousseau, Danielle, Lecture, Forensic Behavior Analysis, 2023
Risk Assessment-Forensic Behavior Analysis
Risk assessment can be determined by forensic psychologists within the prison system to justify whether or not a prisoner is at risk for committing more crime when they are released from prison. A risk assessor is there to prevent criminals from getting out of prison if they still have a key factor in their mind that would make them want to commit crime. There are many different kinds of risk assessment, one of them that stands out is "threat assessment". When looking at how individuals came about committing crime and becoming criminals, there are different social and environmental factors which can take place to cause these outbursts as criminals. There is also the term "dangerousness". Dangerousness is the thought of how dangerous an offender might be when they are re-integrated to the community (Bartol & Bartol, 2020). Risk assessment also includes the understanding of family life, peer interactions, household environment, and individual mental health states. By examining all of these environmental factors as well as different risks that correspond to the environmental factors, researchers will be able to come up with conclusions about how individuals develop criminal tendencies and how they might develop mental health, whether it be genetic or learned from family or peers. "Risk assessment suggests that clinicians and researchers are more proficient at assessing the probability that a given individual—or group of individuals—will engage in harmful behavior than they are at out rightly predicting that someone is dangerous or will be violent" (Bartol & Bartol, 2020).
According to Dr. Rousseau, “Outcomes of forensic assessments can be used to determine criminal responsibility, culpability, capacity to stand trial, and risk of re-offense. Forensic assessment can inform not only court procedures and outcomes, but also placement and treatment planning” (Rousseau, 2023). “In addition to general psychological-testing tools, there are tools that are designed specifically for forensic assessment and the assessment of risk of criminal behavior. Forensic risk-assessment strategies are commonly integrated into a psychological-testing protocol when one is dealing with a client involved in the criminal justice system” (Rousseau, 2023). There is a benefit to having risk assessment within the prison system to make sure that the prisoners who need treatment the most get it. As mentioned above, the program helps place individuals in treatment programs and place them in certain prisons that would benefit them in the long run.
According to the American Psychological Association, “They can give an informed opinion of whether a suspect knew right from wrong at the time of a crime and even whether a minor is being truthful in recounting an unlawful act. Some forensic psychologists work in the area of threat assessment, an emerging science predicting who may be at risk for committing a violent act” (APA, 2014). Understanding the roles of forensic psychologists within the criminal justice system is important because it will help individuals like researchers who are outside of the criminal justice system understand what their mission is and how it is beneficial for everyone that criminals are diagnosed and get the help they need if they are living under a mentally unstable life. Threat assessment is another program which pinpoints the problem and makes sure that it is resolved before the reintegration process is started. After they do their time whether it be at a prison or in a mental institution getting the treatment they need, then the forensic psychologist makes sure that the offender is able to get back into society or if he or she will be a risk to society when they are released. This kind of goes hand in hand with veterans, after coming back from overseas and fighting wars, the forensic psychologists can determine whether or not they need treatment to get them used to the way society is run and make sure they are ready to return to society at the best they can be without having a relapse of fear or anger from their overseas battle (APA, 2014).
The question of owing morale to different branches has come about when talking about forensic psychologists. After they do their time whether it be at a prison or in a mental institution getting the treatment they need, then the forensic psychologist makes sure that the offender is able to get back into society or if he or she will be a risk to society when they are released. This kind of goes hand in hand with veterans, after coming back from overseas and fighting wars, the forensic psychologists can determine whether or not they need treatment to get them used to the way society is run and make sure they are ready to return to society at the best they can be without having a relapse of fear or anger from their overseas battle (APA, 2014).
Overall, by having a specialized unit in the prison system for forensic psychologists to work is a good idea when thinking about the risk assessment and threat assessment models. By having these forensic psychologists work daily to improve this program and find treatment for the criminals incarcerated, this will benefit the overall threat to the community if the criminal gets out of prison. There are specialized units within Law Enforcement Agencies which work directly with the community for community engagement and to make sure that everything is ok in peoples minds and at their homes. For example: a Problem Oriented Policing Unit is formed to follow up with victims of domestic violence. They follow up with them to make sure that everything is ok within the household and their life overall. If there is the slightest of problems, then the officers will find different treatment or counseling programs they could attend to put them back on their feet and get them motivated to move past the incident that occurred in the past.
References:
American Psychological Association. (n.d.). Forensic and public service psychology. American Psychological Association.
Bartol, C. R., & Bartol, A. M. (2020). Criminal Behavior: A Psychological Approach (12th ed.). Pearson Education (US)
Rousseau, D. (n.d.). Assessment In Forensic Psychology. Onlinecampus.bu.edu.
Ketamine Infused Therapy for PTSD

Ketamine Infusion Treatment for Post-Traumatic Stress Disorder (PTSD)
Written By Cady Balde
Over the last two decades, the anesthetic drug ketamine has become a popular new treatment approach for mental health disorders such as anxiety, depression, and post-traumatic stress disorder (PTSD). Derived from the psychedelic drug phencyclidine, commonly known as PCP or angel dust, ketamine is a dissociative anesthetic. Legally, ketamine is a F.D. Ketamine is an approved anesthetic that is commonly used in emergency rooms; however, when used recreationally, it causes mind-altering effects that are described as a "separation of mind from body even as the mind retained consciousness" (Witt, 2021). With regard to illicit drugs and human subject research, purposefully inducing these hallucinogenic properties has raised controversy within the clinical and psychiatric realms. However, in 2006, the National Institute of Mental Health, along with Yale clinician Dr. Gerard Sanacora, found schizophrenic patients experienced mood improvement after receiving a single intravenous dose of ketamine.

Patients who suffer from major depressive disorder, chronic stress, or PTSD experience synapse loss. Synapses are wire-like signals that regulate our brain's responsibility for behavior, mood, and cognitive function. Neurotransmitters such as cortisol, dopamine, and serotonin are brain chemicals that signal danger in our bodies. However, when an individual experiences a traumatic event, these chemicals become imbalanced due to the brain synapses thinking they are in a constant fight-or-flight situation. Ketamine therapy, administered intravenously, has shown promise in re-growing lost synapses. Chief Psychiatrist at Yale-New Haven Hospital, John Krystal, identified that "within 24 hours of a person’s first dose of medically supervised ketamine, those lost connections start to regrow. The more synapses they grow, the better the antidepressant effects of ketamine are for them" (Collins, 2022). Dr. Krystal did note that ketamine therapy should not be used as a sole treatment plan but should be used in conjunction with anti-depressant medication and cognitive behavioral therapy (CBT).
A possible limitation of ketamine infusion therapy is the increased risk of psychosis due to its hallucinogenic effects and the possibility for individuals to develop drug dependence. However, I found ketamine infusion therapy overall to be an effective new treatment approach for those with medication resistant depression and treatment resistant PTSD.
References
Witt, E. (2021, December 29). Ketamine Therapy Is Going Mainstream. Are We Ready? The New Yorker. https://www.newyorker.com/culture/annals-of-inquiry/ketamine-therapy-is-going-mainstream-are-we-ready
Collins, S. (2022, May 4). What is Ketamine? How it Works and Helps Severe Depression. WebMD. https://www.webmd.com/depression/features/what-does-ketamine-do-your-brain
Self-Care: Not Just for Therapists
One of my favorite aspects of this course has been the emphasis on self-care and evaluating self-mental well-being. Two+ years ago when you asked me about what my self-care looked like as an over-tired and overworked 911 dispatcher, I likely would have laughed and asked what that was. Now, as a trauma clinician with a caseload including sexual assault, homicide bereavement, and horrific stories of verbal and physical abuse, the term self-care is engraved in my vocabulary and routine.
Many of us might participate in self-care on smaller levels without even knowing it- exercising, getting our nails done, listening to music, etc. However, taking to time to truly reflect and put energy into our mental and physical well-being takes things a step further. The National Institute of Mental Health reports self-care to be helpful in managing stress, increasing energy, and lowering the risk for illness by doing things focused on improving mental, physical and emotional well-being (NIMH, 2022). Self-care can look different for everyone but is important for all to incorporate it into routine regardless of someone's job. While it's true, someone in my position or in law enforcement, in the medical field might be more immediately exposed to trauma and vicarious traumatization, the practice of self-care certainly doesn't only pertain to those individuals. Some examples of self-care could be:
-exercise
-eating healthy foods
-deep breathing or meditation
-time spent with animals
-drinking enough water
-time spent focusing on hobbies
-setting a healthy sleep routine and goal
For those of us who find it difficult to do things for ourselves, or find ourselves invalidating the need to focus on ourselves, starting to incorporate self-care can start slow and as one small thing a day. For example, if I have had a long day already and am feeling the weight of my client's traumas, I will take 10-20 minutes to sit in the big comfy chair in my office and shut my eyes and take some deep breaths. Something that might seem simple can really have such a big impact. One of the best forms of self-care I have discovered is being able to vent and release such weight to my coworkers who can relate and understand what I am going through. Sometimes opening up to others about the struggles we face can be quite intimidating and force us to feel as though we are alone in feeling the weight of the world. Put yourself out there- start to incorporate the aspects of self-care into your routine little by little and watch it change your life.
U.S. Department of Health and Human Services. (n.d.). Caring for your mental health. National Institute of Mental Health. Retrieved December 16, 2022, from https://www.nimh.nih.gov/health/topics/caring-for-your-mental-health
Warnings signs for suicide in the workplace
The holiday season can be a time of great joy, social support, gifts, and nostalgic traditions. However, the holidays can also be a challenging time for many people, being reminded of their grief and loss, effects of seasonal depression, and end of the year reflections. Some people might feel extremely joyous and hopeful for the new year, and some might feel great anxiety and hopelessness.
In this post, I want to share warning signs for suicidality that may show up in the workplace. Employees that are often sad. There may be changes in the appetites, extreme weight gain or weight loss, and they might be more agitated over time. A decrease in productivity could be an indicator of other issues. Some employees may have trouble concentrating, remembering things, and following through on tasks, and this may be a change in their regular work behavior. You might notice employees having a lot less energy, expressing changes in sleep patterns, showing up late, or not keeping up with their appearance in the same way. They may potentially come to work less, calling out sick, or not attending events as they used to. On the more dangerous spectrum, employees may be under the influence of drugs or alcohol at work and they may even just express thoughts or comments about suicide.
If you are a supervisor or another employee seeing these changes in someone you work with, I would encourage you to approach their behavioral changes with curiosity instead of judgment. An example could be “Hi, I just wanted to check in and see how you’re feeling or if there is any way I can help. I’m noticing that your tasks are being completed late when you used to complete them early.” Also, maintaining confidentiality. If any information is shared, sharing with the proper people in the workplace who can help provide necessary care. It would not help for someone’s mental distress to become workplace gossip. Lastly, reach out to people who can help. Encourage the employee to utilize appropriate hotlines, ask Human Resources for accommodations, or use EAP benefits to get mental health treatment. Don't feel that you have to manage someone’s suicidality alone.
988 Suicide and Crisis Lifeline
Goel, C. (2022, August 8). Top 7 employee suicidal warning signs . Axiom Medical. Retrieved December 15, 2022, from https://www.axiomllc.com/blog/employee-suicidal-warning-signs/