Home
Enabling Evil: How the Nazi Regime Made Atrocities More Palatable
One of the shocking realizations about the Holocaust and other campaigns of genocide around the world is that these atrocities were perpetrated by seemingly ordinary individuals rather than monsters. In his book “Ordinary Men: Reserve Police Battalion 101 and the Final Solution in Poland,” Christopher Browning (1992) explores how average middle-aged German police officers became mass murderers. The author’s “multicausal explanation” (Browning, 1992, p. 215) includes a wide range of factors that include propaganda and dehumanization of the Jews, conformity and peer pressure, deference to authority (however tentative), gradual desensitization and routinization, division of labor, assertions of fear of punishment, career advancement, and the context provided by the war.
Another book features similar themes but appears only as a footnote in Browning’s tome. Hannah Arendt’s (1963) “Eichmann in Jerusalem: A Report on the Banality of Evil” discusses Adolf Eichmann, the mid-level bureaucrat who managed the logistics of deportation of Jews to death camps. This man did not consider himself to be evil, found concentration camps revolting, and could not stand the sight of blood (Arendt, 1963). Yet, this was the man who directed the deportation of Hungarian Jews described in Elie Weisel’s “Night” (2006).
Arendt reveals how the context of living in Nazi Germany shaped the non-Jewish citizens’ thinking about the Jews. Through executive action, Jews were excluded from public service work in Germany beginning in 1933 – nine years before the events discussed by Browning (Wikipedia, 2019). Jewish students were not accepted at universities, and Jewish doctors and lawyers were gradually driven from those professional communities. Nazi troopers habitually vandalized Jewish businesses with total impunity. By 1935, Germany had a separate set of laws for Jews (Wikipedia, 2019). As a result, it was not just propaganda but facts of German life at the time that contributed to the perpetrators’ dehumanization of Jews.
Arendt notes that Heinrich Himmler, the architect of the “final solution,” framed the extermination of Jews as a necessary evil that had to be shouldered by the current generation to secure Germany’s future. Himmler told SS leaders that they must be “superhumanly inhuman” (Arendt, 1963, p. 104). In fact, participation in atrocities was framed not in terms of inflicting horrible things on people but rather in terms of having to shoulder the weight of witnessing the horror (Arendt, 1963). This framing allowed the perpetrators to view themselves as tragic heroes making a short-term sacrifice in the name of a thousand-year Reich.
Another linguistic tool for addressing the potential trauma was the elaborate system of euphemistic language that helped obscure the reality of Eichmann’s and others’ actions. Arendt states that documents where the words “killing” or “extermination” appear are extremely rare. The Nazi government instituted strict “language rules” (Arendt, 1963, p. 83) that replaced the above-mentioned terms with code words such as “final solution,” “evacuation” and “special treatment.” This consistent use of euphemistic terms removed perpetrators from the reality of their actions and was strictly adhered to throughout the entire Nazi government, even in interagency cooperation.
Consistent with Browning’s findings, Arendt notes that breaking the process of genocide into small, ostensibly benign steps was another key mechanism employed by the Nazis. The officers from Reserve
Battalion 101 arrived at this idea by trial and error, but in the upper echelons of the Nazi government, this was part of the design. Arendt illustrates this through Eichmann’s role, which primarily involved managing the logistics of deportations. Eichmann viewed himself not as a facilitator of mass murder but as a transportation expert solving complex problems. In fact, prior to the introduction of the “final solution,” he applied himself to making it easier for Jews to emigrate to Palestine with equal zeal. Wading through Eichmann’s revelations, self-delusions, obfuscations, and lies, Arendt arrives at the image of Eichmann as a middle-class, not supremely talented man whose thoughts were primarily occupied by finding ways to excel and build a career. By focusing solely on the tasks at hand, whether they resulted in saving people or killing people, Eichmann avoided considering the moral dimension of his actions.
The Nazi government's systematic approach to enabling atrocities is a frightening reminder that ordinary people can become complicit in morally reprehensible actions. Through gradual dehumanization, manipulation of language, framing terrible actions as necessary sacrifices, and breaking down the process of genocide into small, seemingly benign tasks, the Nazis created a system that enabled and facilitated moral disengagement. Browning's and Arendt's writings show that we are all vulnerable to the influences of authority, social pressure, and ideology. They remind us that we need to remain mindful and actively resist the forces that push us towards dehumanizing or devaluing any group of people.
References
Arendt, H. (1963). Eichmann in Jerusalem: A Report on the Banality of Evil. London: Penguin Books.
Browning, C. R. (1992). Ordinary Men: Reserve Battalion 101 and the Final Solution in Poland. New York: Harper-Collins.
Wiesel, E., & Wiesel, M. (2006). Night. New York: Hill And Wang. (Original work published 1958)
Wikipedia. (2019, May 2). Nuremberg Laws. Retrieved from Wikipedia website: https://en.wikipedia.org/wiki/Nuremberg_Laws
Controlled Substances For PTSD
Over the decades, psychiatrists have prescribed numerous medications for those suffering from PTSD. More recently, scientists have been curious as to the effects of using psychedelics in attempting to treat Post Traumatic Stress Disorder. The drug professionals are most curious about is methylenedioxymethamphetamine, or MDMA. As with all other medications or brain-altering substances, it is encouraged to seek therapy while taking MDMA to treat one's PTSD. The drug has been shown to reduce fear, increase social engagement and openness, increase empathy and compassion, increase emotionality, and many other benefits (Morland, 2024)
Understandably, there are some fears surrounding the use of substances such as MDMA due to their high addiction rates. This is why it is recommended to only take these substances under a controlled environment where patients can be monitored and the treatment can be stopped if the treatment is beginning to harm the patient or if negative effects are beginning to take shape. Another issue patients may have is that these substances can be quite expensive. They can range from $600 to $8,000 (Olmstead, 2023). Health insurance does not cover these procedures yet as they have not officially hit the market and research is still in progress.
There is a lot more research that needs to be done when considering the long-term effects on the brain for the users of MDMA. For many years the drug has been banned from public consumption and mainly used as a "party drug". However, more and more medical uses have been found for the drug and others which are known to alter one's emotions and to make individuals more easygoing and open to the outside world. Scientists are also looking into using the drug to assist with the treatment of anxiety, substance abuse, and eating disorders. Individuals who wish to seek this type of treatment should speak with their current psychologist and discuss if these types of substances could benefit them or if they are the right type of candidate for further research studies.
References:
Morland, L., & Wooley, J. (2024, March 28). Va.gov: Veterans Affairs. Psychedelic-Assisted Therapy for PTSD. https://www.ptsd.va.gov/professional/treat/txessentials/psychedelics_assisted_therapy.asp#four
Olmstead, K. (2023, September 13). New PTSD treatments offer hope, yet people seeking help should exercise caution. RTI. https://www.rti.org/insights/new-ptsd-treatments-offer-hope-with-caution
Introducing Psychological First Aid Techniques to First Responders
Introducing Psychological First Aid Techniques to First Responders
One of my favorite assignments in this class has been the film review project. For this assignment we were tasked with picking a documentary to watch and analyzing the goal of the documentary. I chose to watch and review the documentary Counselors Responding to Mass Violence Following a University Shooting: A Live Demonstration of Crisis Counseling was created by the American Counseling Association and published by Alexander Street. In this film we saw a presentation about a fictional school shooting at a college and techniques mental health professionals use in the immediate aftermath and a follow up session a month later with one of the survivors. The techniques demonstrated were Psychological First Aid (PFA) and Cognitive Behavioral Therapy (CBT). Psychological First Aid is the technique used in the immediate aftermath of the incident and stood out to me as a powerful tool. While there were a lot of documentaries to choose from, I hope at some point everyone in the class can dedicate some time to watching this.
In this fictional scenario, the presentation shows the use of Psychological First Aid with two different survivors of a mass shooting on a college campus. One of the survivors is a bit more visibly shaken, as she heard the gunshots and saw bodies on the ground. The presenters of this scenario then begin to use Psychological First Aid techniques with the survivor. They first begin with helping the survivor return their breathing to normal by introducing the box breathing exercise to them. This breathing method works by having the person breath in through their nose for four seconds, holding that air in their lungs for four seconds and then releasing that air for four seconds. Repeating this method multiple times helps activate the bodies parasympathetic nervous system after a stressful situation.
The next method of Psychological First Aid the presenters use is asking the survivor to describe five non-distressing objects in the room they are in. In doing this, the survivor became more grounded back to reality and into the present situation she was in. To continue grounding the person back to reality, the presenters then had her describe the things she can feel. The survivor went on to express that she could feel the chair she was sitting in, her jeans on her legs and her feet tapping the ground. One last technique they used was having the survivor describe all the feelings she was currently experiencing.
In both scenarios with survivors, the mental health specialists never directly asked the person to describe what they just witnessed and experienced. Doing so could have a negative impact on the long-term effects of surviving this. They let the survivor decide what and how much information they wanted to discuss. All these methods used in Psychological First Aid are extremely useful and easy to implement while working with a survivor or witness to such a traumatic event.
While in this fictitious scenario the mental health professionals were on scene not too long after the event occurred, I wonder how realistic that is in everyday situations. The fictitious scenario of a mass shooting on a college campus is certainly something we can expect a massive response from all sorts of agencies- including mental health professionals. I sadly doubt that there are similar resources readily presented to those who witness something equally traumatic like a stabbing, fatal car accident or fatal fire. I am aware that in the city of Boston the Boston Police have a partnership with the Boston Medical Center’s Boston Emergency Services Team (BEST). These co-response clinicians ride along with officers and respond to calls that deal more with individuals who are in some sort of mental health crisis in hope to avoid the need to arrest the person. There are also currently only 12 of these co-response clinicians on staff, meaning that there may not always be access to someone with this specialty.
As mentioned, the techniques and methods of Psychological First Aid are easy to implement in real-life situations in the moments after the incident occurs. More likely than not, first responders to scenes will be without a mental health professional. Having all first responders familiar with Psychological First Aid methods would be extremely beneficial. Especially giving them an understanding that sometimes-asking direct questions about what someone just survived or witnessed right in the first moments after it happened may have a long-term negative impact on the trauma they endure from the incident.
Counselors Responding to Mass Violence Following a University Shooting: A Live Demonstration of Crisis Counseling. . (2014).[Video/DVD] American Counseling Association. Retrieved from https://video.alexanderstreet.com/watch/counselors-responding-to-mass-violence-following-a-university-shooting-a-live-demonstration-of-crisis-counseling
Lack of Mental Health Resources in Rural Areas
Throughout this course and reading the course material like Bessel van der Kol’s book The Body Keeps the Score, it is clear that a great deal of time and resources have been put into mental health treatment and the advocacy for it. While this is phenomenal and quite beneficial for people who need it, the only people who can benefit from it are those who have access to services and the various treatments that have been developed. Unfortunately, it is often difficult to find appropriate mental health services, particularly in certain areas of the country. Many people in rural areas will have a more difficult time receiving mental health treatment than their counterparts in urban or suburban areas because of a lack of money, lack of transportation, or limited availability of services.
In areas where people have to drive an hour, or more, to get to the grocery store, a doctor's office, or school, it is very hard to find and utilize specialized treatment, particularly for mental health. The National Library of Medicine put out a publication on this very issue. “Approximately one-fifth of the US population live in a rural area, and about one-fifth of those living in rural areas, or about 6.5 million individuals, have a mental illness [1,2]. Though the prevalence of serious mental illness and most psychiatric disorders is similar between US adults living in rural and urban areas [3,4], adults residing in rural geographic locations receive mental health treatment less frequently and often with providers with less specialized training, when compared to those residing in metropolitan locations.” (ncbi.nlm.nih.gov). While there may not be more people in rural areas that need mental health treatment, as opposed to urban areas, the access that they have to these services is much more limited.
This is such a prevalent issue that there are entire organizations created to combat the disparity of mental health resources in rural areas. The Rural Health Information Hub is one of these organizations. This group has published on their website that “According to the Results from the 2023 National Survey on Drug Use and Health: Detailed Tables, approximately 7.7 million nonmetropolitan adults reported having any mental illness (AMI) in 2023, accounting for 22.7% of nonmetropolitan adults. In addition, 1.6 million, or 4.8%, of adults in nonmetropolitan areas reported having serious thoughts of suicide during the year.” (ruralhealthinfo.org). There is a clear need for mental health resources in vast areas of our country, but the allocation and willingness of trained professional people to relocate to these rural areas is lacking.
While there are an insufficient number of qualified professionals and facilities in these areas, that does not mean that access to these resources is completely cut off. One of the few positive things to come out of the Covid-19 Pandemic was the mainstream acceptance and use of virtual platforms like zoom. Many therapists were able to continue serving their patients through platforms like this. Virtual treatment may not be a complete substitute for in person or more intensive treatment. By itself, making such services available will probably not solve the problem of limited mental health treatment in rural America. However, for many patients who need a therapist to talk through things, but do not not necessarily need inpatient treatment, virtual therapy can provide many of the benefits of in person therapy. Virtual therapy appointments can provide some important relief when no other services are available..
The limited availability of mental health services in rural America highlights another issue , which is a more limited acceptance of mental health treatment or a stigma in these areas. Several involved groups have observed that there is a greater stigma associated with mental illness and treatment in rural communities than in urban communities. (nami.org, usda.gov). As mental health services become more available, even starting with virtual treatment, treatment may become more acceptable and this stigma may be reduced. More people may seek out and be willing to use treatment.
Ultimately however, with all of this in mind, the question of why there are so few resources dedicated to this in rural areas will need to be addressed if we plan to make necessary services available equally to all Americans.
Citation:
Morales, Dawn A, et al. “A Call to Action to Address Rural Mental Health Disparities.” Journal of Clinical and Translational Science, U.S. National Library of Medicine, 4 May 2020, www.ncbi.nlm.nih.gov/pmc/articles/PMC7681156/.
Nami. “Confronting Mental Health Challenges in Rural America.” NAMI, 7 May 2024, www.nami.org/advocate/confronting-mental-health-challenges-in-rural-america/.
“Rural Mental Health Matters: Challenges, Opportunities & ...” USDA.Gov, United States Department of Agriculture,
www.usda.gov/sites/default/files/documents/mental-health-awareness-month-community-webinar.pdf. Accessed 12 Aug. 2024.
“Rural Mental Health Overview - Rural Health Information Hub.” Overview - Rural Health Information Hub, www.ruralhealthinfo.org/topics/mental-health. Accessed 9 Aug. 2024.
How To Think When Interacting With Justice Impacted Youth
Youth justice is an essential area of concern for the criminal justice system that is often not given enough attention (Rousseau, 2024). Trauma and crisis related issues involving youth are far more common than society perceives, and the current systems in place, are not equipped to effectively aid justice-impacted youth (Rousseau, 2024). It is important to remember that there are fundamental differences between how youth and adults react to trauma, and as a result, there are two significant considerations that practitioners should keep in mind when interacting with justice impacted youth. Incorporating these suggestions into daily practice will ensure that proper and effective treatment is administered.
The first consideration to keep in mind is that youth often don’t openly disclose trauma that’s affecting them. Youth do not openly discuss the traumatic experiences of their lives, which can act as a barrier for both diagnosis and treatment (van der Kolk, 2014) - it is impossible to effectively administer treatment if we are unaware of what we are treating. This lack of forthcomingness should not be viewed as youth being intentionally “difficult”, but a consequence of them experiencing trauma at such a young age. Studies have shown that early trauma can affect the development of the prefrontal cortex, which causes increased sensitivity to physical and psychological environments (Rousseau, 2024). Keep in mind that the resulting changes to the prefrontal cortex can lead some youth to become hypersensitive to stressful stimuli, unable to self-regulate emotions, or have elevated levels of fear or anxiety (Rousseau, 2024). Those who interact with which justice impacted youth need to recognize that their demeanor and lack of transparency is a natural part of their reaction to trauma, and therefore interactions should be adapted accordingly.
Secondly, practitioners should recognize that due to a lack of openness on the part of youth, misdiagnosis is common (van der Kolk, 2014). When working with justice-impacted youth, it is important to look past any previous diagnostic labels since they can be unrepresentative of that individual. False diagnosis can lead to improper treatment, and therefore the underlying issues of that patient, will never be addressed. Diagnoses can stick, meaning that a patient might be destined to an ineffective treatment plan if practitioners don’t look past previous labels. While it’s not suggested to throw out any previous diagnoses, what is important to remember is that based on the nature of how youth respond to trauma as discussed above, practitioners should reasonably question previous diagnosis in order to determine effective treatment plans.
To better integrate trauma informed practices into juvenile justice there are a number of recommendations that can be implemented such as the following;
- Utilize trauma screening and assessment;
- Incorporate evidence-based trauma treatments designed for all justice settings;
- Partner with families and communities to reduce the potential traumatic experience of justice involvement;
- Collaborate across all juvenile justice systems to enhance continuity of care;
- Create and enhance a trauma-responsive environment of care;
- Reduce disproportionate minority contact while addressing the disparate treatment of minority youth (Rousseau, 2024).
In addition to these recommendations, it would be beneficial to recognize that triggers and stressors are different for every youth, and that every aspect of a youth's life can act as a stressor or trigger to their trauma. Since trauma impacted youth can have their entire lives affected by trauma, it is important for professionals working with youth to understand that everyday interactions can pose significant challenges and should therefore adapt their behavior accordingly (Van Der Kolk, 2014).
Additionally, practitioners should remember that reactions to trauma can, and often are different for everyone. Labeling a reaction as “not normal” or “unreasonable” would be an improper trauma-informed practice. While tolerance might not always be easy, it is an essential practice when interacting with trauma impacted youth.
Bibliography
Rousseau, D. (2024). Module 2: Childhood Trauma. Boston University Metropolitan College.
van der Kolk, B. A. (2014). The body keeps the score: Brain, mind, and body in the healing of trauma.
A Brief History of Trauma and PTSD
The word trauma is widely known and its meaning is generally understood. However, it can oftentimes be misused to add dramatic effect to a situation; for example, using the phrase, “That was traumatizing,” when perhaps merely an embarrassing situation occurred. Was it traumatizing? What does it mean to be traumatized? As the American Psychological Association (2024) defines it, “Trauma is an emotional response to a terrible event like an accident, crime, natural disaster, physical or emotional abuse, neglect, experiencing or witnessing violence, death of a loved one, war, and more.” When emotional responses such as shock, flashbacks, denial, and physical symptoms such as headaches or nausea persist well after the occurrence of an event, a person is likely suffering from trauma.
What may be less commonly known is the history of the word trauma. Trauma is derived from the Greek word τραῦμᾰ, or traûma, meaning “wound,” with roots dating back to the mid-1600s (Kolaitis et al., 2017). Although the word was originally used in reference to a physical wound, it is now more commonly used to refer to an emotional wound. Let’s look at the year 1861, the beginning of the American Civil War when terms such as “soldier’s heart” and “nostalgia” were used when referring to a soldier's response to traumatic stress. Fast forward 53 years to the beginning of World War I. During this time, the term “shell shock” was introduced to describe the physiological responses that soldiers were experiencing as a direct result of heavy explosives. As noted in Trauma-Informed Care in Behavioral Health Services (2014), “Even with a more physical explanation of traumatic stress (i.e., shell shock), a prevailing attitude remained that the traumatic stress response was due to a character flaw.” At this time, Charcot, Janet, and Freud were articulating that the symptoms that soldiers were experiencing were a direct result of psychological trauma. However, by the year 1939 and the next World War, this information was still falling on deaf ears, as military recruits were being screened to keep out any “who were afflicted with moral weakness.” However, advancements in treatment were being introduced, including allowing soldiers to rest from “battle fatigue.” Talk therapy emerged during the Korean and Vietnam wars, between the years of 1950 and 1975.
Though it took longer than it should have to come to the realization, we now know that there is no single definition of trauma. “The ways we are exposed to trauma are vast, and the individual's response to it is personal. Cultural differences, protective factors, and sense of self can all cause very different outcomes for two people witnessing the same event (Rousseau, 2024, Module 1: Introduction to Trauma).” As van der Kolk expresses in The Body Keeps The Score: Brain, Mind, and Body in The Healing of Trauma (2014, p. 19), it was not until 1980 that the formal diagnosis of PTSD was developed; an effort made by a group of Vietnam veterans and New York psychoanalysts, Chaim Shatan and Robert J. Lifton. Before this, individuals suffering from the symptoms of post-traumatic stress disorder, most of those war veterans, were being unsuccessfully diagnosed with alcoholism, substance abuse, depression, mood disorder, and schizophrenia. Subsequently, they were being treated with the wrong types of medications, and the wrong forms of therapy. Now, almost 45 years later, we also know that there are many different forms of care available for addressing the impact of trauma, including pharmacotherapy, cognitive behavioral therapy, exposure therapy, EMDR, neurofeedback approach, internal family systems therapy, yoga, mindfulness, theater, emotional freedom technique, service dogs, and gender-responsive approaches. We also understand that the symptoms of PTSD are very real, and are in no way due to “moral weakness.”
References
American Psychological Association. (2024). Trauma. Retrieved from, https://www.apa.org/topics/trauma
Kolaitis, G., & Olff, M. (2017). Psychotraumatology in Greece. National Library of Medicine. Retrieved from, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5632764/
National Library of Medicine. (2014). Trauma-Informed Care in Behavioral Health Services: Appendix CHistorical Account of Trauma. Retrieved from, https://www.ncbi.nlm.nih.gov/books/NBK207202/
Rousseau, D. (2024). Boston University Metropolitan College, Module 1: Introduction to Trauma. https://onlinecampus.bu.edu/ultra/courses/_127887_1/cl/outline
Van der Kolk, B. A. (2014). The Body Keeps The Score: Brain, Mind, and Body in The Healing of Trauma. (1st edition). Viking Penguin.
Yoga – A Therapeutic Approach for Addressing Trauma
Written by Bessel van der Kolk in 2014, The Body Keeps the Score: The Brain, Mind, and Body in the Healing of Trauma is a New York Times bestseller that looks at trauma and its impact on reshaping the brain, mind, and body.
Part five of this novel, titled “Paths to Recovery”, introduces the audience to a number of therapeutic ways in which individuals address trauma in hopes of healing from their traumatic experiences. This may include “finding a way to become calm and focus, learning to maintain that calm in response to images, thoughts, sounds, or physical sensations that remind you of the past, finding a way to be fully alive in the present and engaged with the people around you, and not having to keep secrets from yourself, including secrets about the ways that you have managed to survive” (van der Kolk, 2014). One in particular stood out which will be the focus on this blog post and that is yoga.
In The Body Keeps the Score: The Brain, Mind, and Body in the Healing of Trauma, van der Kolk highlighted the impact that mediation has on the brain, specifically yoga. When an individual alleviates the muscle tension in their body, this allows the individual to relax and feel a sense of calmness. Individuals who are experiencing trauma may feel tense or numb because of the trauma that they endured or still continue to endure (van der Kolk, 2014). However, yoga allows these individuals to feel connected to their bodies again. Additionally, yoga therapy is designed to regulate an individual’s arousal and control their physiology (van der Kolk, 2014). Van der Kolk found in a study that ten weeks of yoga reduced PTSD symptoms in individuals who previously attempted to use medications to reduce PTSD but failed (van der Kolk, 2014). In order to relax the mind and heal from trauma, mediation is key.
A 2022 study done by the Cleveland clinic looked at 64 women who were living with chronic, treatment-resistant PTSD (“How Yoga Can Help Heal Trauma”, 2022). The researchers decided to split the women in two groups for them to participate in: trauma-informed yoga or women’s health education. 52% of women no longer met the criteria for PTSD after participating in the yoga trial while only 21% of women no longer met the criteria for PTSD after participating in the education trial (“How Yoga Can Help Heal Trauma”, 2022). Trauma informed yoga is designed to make you feel safe and relaxed. By participating in this, individuals are more likely to feel in control of their body and mind rather than a stranger in their own body and mind (“How Yoga Can Help Heal Trauma”, 2022).
Yoga also plays a major role in prisons. Most incarcerated individuals face feelings of anxiety, stress, and trauma as they are locked in cells for a long period of time. Written by Dragana Derlic, A Systematic Review of Literature: Alternative Offender Rehabilitation—Prison Yoga, Mindfulness, and Meditation is an article that focuses on the importance of yoga, mindfulness, and mediation in order to reduce recidivism and increase the likelihood of rehabilitation (Derlic, 2020). The initiation of yoga programs in prisons is designed to reduce negative thoughts, create a sense of relaxation, strengthen inmates’ attitudes, and show them that there are people out there that still care about them and their health. Not only does yoga reduce stress, anxiety, and trauma, but yoga also plays a vital part in improving an individual’s physical and mental health (Derlic, 2020).


References
Derlic, D. (2020). A systematic review of literature: Alternative offender rehabilitation—prison yoga, mindfulness, and meditation. Journal of Correctional Health Care, 26(4), 361–375. https://doi.org/10.1177/1078345820953837
“How Yoga Can Help Heal Trauma” (2022). Cleveland Clinic. Retrieved from https://health.clevelandclinic.org/trauma-informed-yoga
van der Kolk, B. (2014). The body keeps the score: Brain, mind, and body in the healing of trauma. New York. Penguin Books.
Art Therapy for PTSD
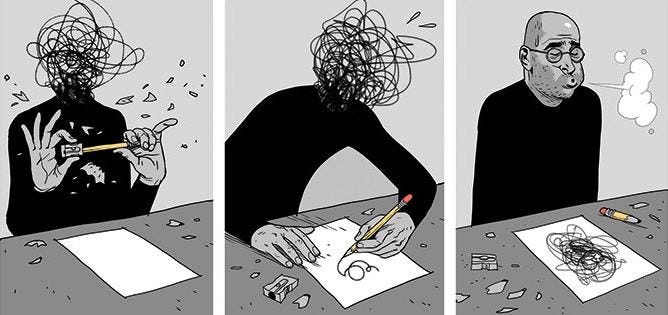
When it comes to trauma, there are different outlets that help with the recovery process. One way of processing is through expressing and finding peace. Art therapy offers a unique and powerful avenue for self-discovery and healing by providing an innovative approach to mental health and emotional well-being. According to the American Art Therapy Association, “Art Therapy is an integrative mental health and human services profession that enriches the lives of individuals, families, and communities through active artmaking, creative process, applied psychological theory, and human experience within a psychotherapeutic relationship” (2017). There are many creative means to art therapy such as, “drawing, painting, coloring, collage, and sculpture” (Fabian, 2019). For individuals who live with PTSD, art therapy can help enhance emotional expression by having a safe outlet when it is difficult for them to verbalize their feelings.
Art therapy is usually led by licensed art therapists who help guide those who have had traumatic events, such as those with PTSD, through the creative process. During the sessions, the therapists use different exercises that allow free expression of the individual’s goals and needs. The clients are encouraged to discover their feelings and experiences through their specified art medium. With the therapists ongoing support and comprehension, they help the client expand a deeper perception of their inner selves (Fabian, 2019). According to Van der Kolk, “there are thousands of arts, music, and dance therapists who do beautiful work with abused children, soldiers suffering from PTSD, incest victims, refugees, and torture survivors, and numerous accounts attest to the effectiveness of expressive therapies (p. 260, 2014). Through art therapy, therapists “enable clients to grow on a personal level through the use of artistic materials in a safe and convenient environment” (Hu et al, 2021).
This form of therapy offers a beneficial and balancing approach to managing PTSD. By opening the power of creativity, individuals can find new ways to process their trauma, gain insight, and move toward healing and recovery. Art therapy helps with reducing anxiety and stress by having a calming and meditating aspect which allows the clients to feel comfortable. The art creates a deeper understating of their feelings and heal from the traumatic experience which creates a sense of control and resilience. By working with a therapist who is trained and certified, this can help build a therapeutic relationship with the client which would allow them to participate and be more open with their experiences (Good Therapy, 2024).
Bedi, S. (2017, September 18). My experience with art therapy!. Medium. https://medium.com/@saniyabedi05/my-experience-with-art-therapy-2124afc9f2f7
Fabian, R. (2019, August 13). How art therapy can heal PTSD. Healthline. https://www.healthline.com/health/art-therapy-for-ptsd#PTSD,-the-body,-and-art-therapy
Hu, J., Zhang, J., Hu, L., Yu, H., & Xu, J. (2021). Art Therapy: A Complementary Treatment for Mental Disorders. Frontiers in psychology, 12, 686005. https://doi.org/10.3389/fpsyg.2021.686005
A therapist explains why we shut down when flooded with big emotions. UnityPoint Health. (2024). https://www.unitypoint.org/news-and-articles/a-therapist-explains-why-we-shut-down-when-flooded-with-big-emotions#:~:text=Risk%20of%20Addiction%2C%20Self%2DHarm,negatively%20impact%20a%20person’s%20health.
Van der Kolk, B. (2014). Language: Miracle and Tyranny. In The Body Keeps Score: Brain, Mind, and Body in the Healing of Trauma (pp. 248-266). essay, Penguin Books.
What is art therapy?. American Art Therapy Association. (2024, January 17). https://arttherapy.org/what-is-art-therapy/
Using Horror as a Therapeutic Tool for Trauma and Trauma Disorders
In the field of trauma and crisis intervention, innovative approaches to therapy are constantly being explored to enhance treatment outcomes. One emerging and somewhat unconventional method involves the use of horror—through movies, video games, and thrill attractions—as a therapeutic tool for individuals dealing with trauma and trauma-related disorders. While this approach may seem counterintuitive, the potential benefits of engaging with horror media in a controlled environment offer intriguing possibilities for trauma recovery.
The Psychology of Horror: Facing Fears in a Safe Space
Horror media, whether it’s a spine-chilling movie, a tension-filled video game, or an adrenaline-pumping haunted house, taps into deep-seated fears and anxieties. For many, these experiences are thrilling and even enjoyable, providing a way to confront and process fear in a controlled setting. This concept aligns with the therapeutic principle of exposure therapy, which involves gradually and safely exposing individuals to anxiety-provoking stimuli to reduce fear responses over time (Foa & Kozak, 1986).
Exposure Therapy in a Different Light
Exposure therapy has long been a cornerstone in treating anxiety disorders and PTSD. The underlying principle is that repeated, controlled exposure to the source of fear or trauma can help desensitize individuals and reduce avoidance behaviors. Horror media can serve a similar function by allowing individuals to confront fear in a context where they know they are not in actual danger. This controlled exposure can help trauma survivors regain a sense of agency and control, which is often lost after traumatic experiences (Pittman & Karle, 2015).
The Therapeutic Potential of Horror Media
Emotional Processing and Catharsis
Horror movies and video games often evoke strong emotional responses, ranging from fear and anxiety to relief and exhilaration. This emotional rollercoaster can serve as a form of catharsis, helping individuals process complex emotions associated with their trauma. Research suggests that horror fans may use this genre as a way to confront their fears and anxieties in a safe, manageable way, which can lead to a sense of mastery over these emotions (Clasen, 2017).
Re-experiencing and Reclaiming Narrative
For trauma survivors, horror media can provide a unique opportunity to re-experience fear and terror within a narrative framework. Unlike real-life trauma, where individuals often feel helpless, engaging with horror media allows for a controlled re-experiencing of fear, where the individual can pause, stop, or disengage at any time. This can empower trauma survivors to reclaim their narrative and develop a new relationship with fear (Scrivner et al., 2021).
Social Connection and Shared Experience
Horror is often a shared experience, whether watching a scary movie with friends or discussing a horror game online. This shared experience can foster social connection, reducing feelings of isolation that often accompany trauma. Group therapy sessions incorporating horror media could potentially strengthen group cohesion and provide a shared platform for discussing fears and coping strategies (Scrivner, 2020).
Clinical Considerations and Ethical Implications
While the use of horror media as a therapeutic tool is intriguing, it is essential to consider the clinical and ethical implications. Not all individuals may benefit from this approach; for some, horror media could exacerbate symptoms or trigger distressing memories. Therefore, careful screening and individualized treatment planning are crucial. Clinicians should also be trained to handle potential negative reactions and provide appropriate support.
Moreover, this approach should be seen as a complementary tool rather than a standalone treatment. Integrating horror media into a broader therapeutic framework that includes established methods like Cognitive Behavioral Therapy (CBT) and Eye Movement Desensitization and Reprocessing (EMDR) may offer the best outcomes for trauma survivors (Shapiro, 2017).
The use of horror as a therapeutic tool for trauma and trauma-related disorders is a novel approach that challenges conventional treatment paradigms. By leveraging the psychological mechanisms of exposure, emotional processing, and narrative control, horror media has the potential to help trauma survivors confront and master their fears in a safe, controlled environment. While more research is needed to establish the efficacy of this approach, it offers a fascinating avenue for expanding the therapeutic toolbox in trauma and crisis intervention.
References:
Clasen, M. (2017). Why Horror Seduces. Oxford University Press.
Foa, E., & Kozak, M. (1986). Emotional Processing of Fear: Exposure to Corrective Information. Psychological Bulletin, 99(1), 20-35.
Pittman, C., Karle, E. (2015). Rewire Your Anxious Brain: How to Use the Neuroscience of Fear to End Anxiety, Panic, and Worry. New Harbinger Publications.
Scrivner, C. (2020). The Psychology of Horror: Why Scary Movies and Thrilling Attractions Are Good for You. Journal of Media Psychology, 32(2), 85-94.
Scrivner, C., Johnson, J., Kjeldgaard-Christiansen, J., & Clasen, M. (2021). Pandemic Practice: Horror Fans and Morbidly Curious Individuals are More Psychologically Resilient During the COVID-19 Pandemic. Personality and Individual Differences, 168, 110397.
Shapiro, F. (2017). Eye Movement Desensitization and Reprocessing (EMDR) Therapy: Basic Principles, Protocols, and Procedures. Guilford Press.
American Heroes: The Battlefield Against PTSD
Mental health professionals recognize that trauma comes in different forms and there is no “one size fits all” for treatment. Combat trauma was something observed after World War I, and it was through combat veterans that PTSD was given its name and recognition as a formal diagnosis in 1980. (van der Kolk, 2014). Since the beginning of the war in Iraq and Afghanistan in 2001, our country has seen a tidal wave of soldiers returning home to face a secondary battle with PTSD. In response, a variety of organizations and programs have been organized to help fight this new epidemic, and one charitable organization leading the effort is the Wounded Warrior Project (WWP). What first started in 2003 as a group who provided basic needs and comfort items to wounded soldiers returning from the war, the WWP has now ballooned into a sophisticated operation that has served millions of service members and their families. (Wounded Warrior Project, 2024).
The WWP project has three main programs to assist veterans. WWP Talk offers weekly telephone therapy sessions to veterans and their families at no cost. (Wounded Warrior Project, 2024). This provides vital care to those who could not afford private therapy and those who are unable to travel to an on-site provider. (Wounded Warrior Project, 2024). These therapy sessions also focus on the veteran setting goals while the therapist recommends resources and helps devise a plan to help the person achieve those goals. (Wounded Warrior Project, 2024). Project Odyssey is 12-week program with a five-day retreat that incorporates outdoor activities that teach veterans how to communicate better, develop resiliency, and restore self-confidence. (Wounded Warrior Project, 2024). Because many veterans are still physically active and enjoy adventure activities, this is a unique way to offer education and treatment while allowing the veteran to engage in activities that excite them. (Wounded Warrior Project, 2024). Finally, the Warrior Care Network focuses on more intensive medical treatment through a partnership with several world-renowned medical centers. (Wounded Warrior Project, 2024). Whether suffering with PTSD, TBI, or sexual trauma, veterans receive treatment that is custom tailored for their needs. (Wounded Warrior Project, 2024). This 2-week in person program gives the veteran an average of 50 hours of trauma treatment in addition to talk therapy, yoga, nutrition advising, etc. (Wounded Warrior Project, 2024).
Treatment for combat veterans is different from other types of trauma, because soldiers can also suffer from physical conditions such as a traumatic brain injury. (Rousseau, 2024). While a lot of the symptoms can be the same as those of PTSD, treatment options vary widely. Perhaps the most important goal in treating veterans suffering from PTSD is that we provide trauma informed care. (Rousseau, 2024). Regardless of the type of trauma one has suffered, the goal should be to provide treatment that includes a proper diagnosis, proven treatment practices, and a respectful collaboration with families and communities. (Rousseau, 2024). This is why the WWP programs are a valuable resource for our veterans. They receive specialized care associated with trauma from combat and they never pay for anything. All treatment costs, transportation, and housing is included. The founders of this program have made sure that no one goes untreated due to their financial circumstances or geographical location. The WWP is an example of a charitable organization formed to provide specialized care to a specific type of trauma victim. As a result, individuals are given care that is optimal for their condition and circumstances.
Sources:
Rousseau, D. (2024). Module 1& 2. Boston University.
van der Kolk, B. (2014). The Body Keeps the Score. Penguin Books.
Wounded Warrior Project (n.d.). Veterans & PTSD. Retrieved August 4, 2024, from https://www.woundedwarriorproject.org/programs/mental-wellness/veteran-ptsd-treatment-support-resources