CJ 720 Trauma & Crisis Intervention Blog
Animal-Assisted Intervention and Trauma
There are several different therapeutic approaches available to trauma victims. One of which is called animal-assisted intervention (AAI). AAI is defined as “the utilization of various species of animals in diverse manners beneficial to humans” (American Veterinary Medical Association, 2023). The most common form of this approach seen in everyday life is through the use of service dogs. Psychiatric service dogs are specially trained to assist their handlers in the areas where assistance is needed, especially if the handler is incapacitated (Rousseau, 2023). However, service dogs go far beyond providing physical assistance. They also provide mental and emotional assistance as well. Studies prove that the use of AAI has proved to be beneficial in a number of populations such as trauma victims suffering from post-traumatic stress disorder (PTSD), individuals with dementia and children diagnosed with autism spectrum disorder (O'Haire, et al., 2015).
In regards to individuals suffering from PTSD, researchers found that emotional numbness and isolation are common symptoms. AAI has proven to be beneficial to individuals with PTSD because the presence of an animal such as a dog encourages positive emotions and warmth (O'Haire, et al., 2015). Further, animals have been demonstrated to be social facilitators, which connect and unite people thus reducing loneliness and ultimately isolation (O'Haire, et al., 2015). Animals also require routine care, which can mean daily walks, a trip to the store for food, and bathroom breaks. All of which encourages an individual with PTSD to get out of the house and socialize with the world.
As such, animal-assisted intervention is an effective therapeutic approach worth considering for trauma victims.
References
American Veterinary Medical Association. (2023). Animal-assisted interventions: Guidelines. American Veterinary Medical Association. https://www.avma.org/resources-tools/animal-health-and-welfare/service-emotional-support-and-therapy-animals/animal-assisted-interventions-guidelines#:~:text=Animal%2Dassisted%20intervention%20(AAI),types%20of%20animal%2Dassisted%20intervention.
O'Haire, M. E., Guérin, N. A., & Kirkham, A. C. (2015). Animal-Assisted Intervention for trauma: a systematic literature review. Frontiers in psychology, 6, 1121. https://doi.org/10.3389/fpsyg.2015.01121
Rousseau, D. 2023. Module 4: Pathways to Recovery: Understanding approaches to trauma treatment. Boston University.
The Adverse Childhood Experience (ACE) Study
The Adverse Childhood Experience (ACE) was the biggest study of its kind ever created (Rousseau, 2023). In 1958, Dr. Vincent Felitti and his colleague Dr. Robert Anda of Kaiser Permenente studied more than 50,000 patients, finding clear characteristics or commonalities (Rousseau, 2023). It is highlighted that the most damaging statistic found is how the trauma could later manifest into adults (Rousseau, 2023). Furthermore, as the number of ACE categories higher, the number of conditions also increases (Rousseau, 2023). When there is exposure to one category, there is an 80% likelihood of exposure to another category (Rousseau, 2023). These ACE categories include, alcoholism and alcohol abuse, chronic obstructive pulmonary disease, depression, drug use, heart and liver disease, risk of partner violence, smoking, suicide, and overall decline in quality of life (Rousseau, 2023).
Expanding more about the ACE study, Felitti and Anda spent more than a year creating ten new questions that involved defined categories of adverse childhood experiences which included, physical and sexual abuse, physical and emotional neglect, and family dysfunction like having parents who were divorced, mentally ill, addicted, or in prison (van der Kolk, 2014). Ultimately, the ACE study showed that traumatic life experiences during childhood and adolescence are a lot more common than previously expected (van der Kolk, 2014). It is stated that the study respondents were mainly White, middle class, middle aged, well educated, and financially secure enough to have good medical insurance, highlighting that only one-third of the respondents stated no adverse childhood experiences (van der Kolk, 2014). Additionally, the study revealed that the effects of trauma permeated these patients’ adult lives (van der Kolk, 2014). An example mentioned is that high ACE scores turned out to correlate with higher workplace absenteeism, financial issues, and less lifetime income (van der Kolk, 2014).
Furthermore, Felitti and his team discovered that adverse experiences are interrelated, even though they are usually studied individually (van der Kolk, 2014). For example, people do not usually grow up in a household where one brother is in prison, but everything else is okay (van der Kolk, 2014). Incidents of abuse are never ‘standalone’ events, and for each additional adverse experience reported, the toll in later damages rises (van der Kolk, 2014). Felittti and his team also discovered that the impact of childhood trauma initially became noticeable in school (van der Kolk, 2014). Referring to the ACE study results, more than half of those with ACE scores of four or higher reported having learning or behavioral issues, which was compared with three percent of individuals with a score of zero (van der Kolk, 2014). It is expressed that as the children matured, they did not ‘outgrow’ the impact of their early experiences (van der Kolk, 2014). Felitti highlights, ‘“Traumatic experiences are often lost in time and concealed by shame, secrecy, and social taboo”’ (van der Kolk, 2014). However, the ACE study revealed how the effects of trauma permeated these patients’ adult lives (van der Kolk, 2014).
Moreover, after Robert Anda presented the results of the ACE study, he realized that they had found the gravest and most expensive public health issue in the United States, which is child abuse (van der Kolk, 2014). Anda’s calculations entailed that the overall costs surpassed those of cancer or heart disease (van der Kolk, 2014). In addition, eliminating child abuse in America would lessen the overall rate of depression by more than half, alcoholism by two-thirds, and suicide, IV drug use, and domestic violence by three-quarters (van der Kolk, 2014). Eradicating child abuse in America would also have a huge impact on workplace performance, and greatly lessen the need for incarceration (van der Kolk, 2014). Furthermore, follow up studies and papers are still showing up around the world regarding the ACE study. However, the day to day reality of those who suffered child abuse, as well as children in outpatient clinics and residential treatment centers around the country remains the same (van der Kolk, 2014). The only difference now, is that they receive high doses of psychotropic agents, which makes them more manageable, but will also affect their ability to feel pleasure and curiosity, to grow and develop emotionally and intellectually, and to ultimately become contributing members of society (van der Kolk, 2014).
Expanding more on psychotropic agents, the reason why taking medications could be effective, is because it could be used to lessen extreme or debilitating symptoms as an initial step in trauma recovery (Rousseau, 2023). A few of the symptoms that could be lessened with medication include, sleep disorders, hyperarousal, emotional reactivity, depression, and intrusive or recurring thoughts and images (Rousseau, 2023). However, it is highlighted that an approach that may work for one person, may not work for another, potentially even increasing the other person’s experience of trauma symptoms (Rousseau, 2023). Nonetheless, pharmacotherapy, or the use of medication, is one approach to addressing the impact of trauma, specifically in situations where people will experience symptoms like anxiety, depression, or other mental health problems associated with traumatic experiences. Pharmacotherapy would be a very effective approach, especially in tandem with other therapeutic approaches, like psychotherapy in order to provide a comprehensive treatment plan (Alcohol and Drug Foundation, 2021).
Elaborating more on pharmacotherapy, from a neurology perspective, there are many different neurotransmitters in one’s brain (Rousseau, 2023). All in all, pharmacotherapy works by manipulating neurons and neurotransmitters to gain the desired effect (Rousseau, 2023). In addition, medications can be effective in reducing specific symptoms associated with trauma such as, intrusive thoughts, nightmares, or panic attacks. Furthermore, medicines that target the autonomic nervous system, like propranolol or clonidine, could help in lessening hyperarousal and reactivity to stress (van der Kolk, 2014). This group of drugs works by blocking the physical effectiveness of adrenaline and the fuel of arousal, therefore lessening nightmares, insomnia, and reactivity to trauma triggers (van der Kolk, 2014). Additionally, blocking adrenaline can help to keep the rational brain online and make choices possible (van der Kolk, 2014). Ultimately, a detailed approach by a mental health professional is crucial to identify the most appropriate treatment approach, whether it involves medication, psychotherapy, or a combination of both.
Lastly, referring back to the importance of the ACE study, the implementation of this research could be very beneficial if integrated in one’s workplace. For example, providing training among professionals to recognize and respond to people affected by adverse childhood experiences. This could provide more awareness into one’s potential trauma history, guiding more efficient and sensitive methods. Another implementation could be developing support systems that consider the findings of the ACE study in order to help those affected by childhood trauma. Overall, the goal is to use the ACE study’s findings to apply more informed, understanding, and efficient approaches when dealing with people who have experienced childhood traumatic events.
Resources:
Australian Drug Foundation. (2021). Pharmacotherapy for young people. Alcohol and Drug Foundation. https://adf.org.au/talking-about-drugs/seeking-help/pharmacotherapy-young-people/what-is-pharmacotherapy/#:~:text=Pharmacotherapy%20is%20the%20treatment%20of,with%20a%20legally%20prescribed%20substitute.
Rousseau, D. (2023). BU Learn. Retrieved from https://learn.bu.edu/bbcswebdav/pid-12438217-dt-content-rid-91014393_1/courses/23fallmetcj720_o2/course/module1/allpages.htm
Van, K. B. A. (2014). The body keeps the score: Brain, mind, and body in the healing of trauma.
Existential Crisis Online: Where is the Trauma Hidden?
Contemporary literature defines racism and ethnoviolence as one of the main catalysts for causing traumas in individuals, where racism is a system of oppression based on racial categories and domination considering one group to be superior while the others inferior, and ethnoviolence is violence and intimidation of members of particular ethnic groups who are stigmatized by the dominant culture to maintain their status in society (Helms & Nicolas, 2010: 54). Undoubtedly, a continuous exposure to violent oppression regarding a person’s inherent cultural or racial self- integrity may shape PTSD symptoms. This is happening mainly because both racial and ethnic features are innate, and individuals are victimized due to their identity that under pressure leads to denial of their self-identity and self-hatred or constant fear to be judged and blocked from opportunities. In other words, on a regular basis individuals receive a reminder from a society that they belong to a marginalized group, and this fact shapes a cycle of oppression so the brain stays in the state of constant alert, developing symptoms such as aggression, anxiety, depression, panic attacks, etc.
Now, the dilemma of trauma targeting minority groups is that mostly it involves psychological abuse rather than the physical one, and for this reason, it is easy to overlook the problem since it may be a victim's subjective interpretation of events. Thus, the scholarship has identified that it is important to distinguish the difference between harassment and discrimination. If, indeed, the harassment includes the active person-level discrimination that is more straightforward, the discrimination itself is more passive and may be emotionally avoidant. Helms and Nicolas (2010) revealed the findings that “people’s psychological and emotional reactions to racial harassment were more intense and lasted longer than their reactions to racial discrimination” (Helms & Nicolas, 2010: 56). What’s more, another investigation shows a high correlation between identity-based violence and symptoms as well: the higher levels of such racism-related experiences, the higher levels of general stress, suicidal ideation, state and trait anxiety, and clinical depression are being produced (Helms & Nicolas, 2010: 58). Hence, it is possible to conclude that the more racism or ethnoviolence takes the harassment approach, the more interpersonal it becomes, and receives more adverse impact on an individual's self-reflection and self-recognition in society. Despite the missing traces of physical abuse, psychological abuse involves verbal and non-verbal communication: with racism and ethnoviolence it includes the negative treatment that a victim cannot change (gender, race, ethnicity, religion) causing existential crisis. This is crucial to highlight because it is massive and being characterized with inner conflicts due to confusion of personal identity. Consequently, it destroys an individual’s vision of the world, making him/her vulnerable in every single aspect: self-development, personal relationships, career, etc.
That being said, writing this blog post, I would like to state that even though identity-based traumas are silent, they cause alienation that deeply affects emotional, cognitive as well as behavioral elements of an individual. The revealed fact that passive discrimination does not contribute as much as the individual harassment, does not mean that it does not add to each person individually as a global tendency shaping the overall climate of alienation. Discrimination cannot receive a full acceptance as a matter of fact, rather it is manifested through unreported PTSD symptoms that these individuals tend to deny as a priori position themselves as a failure due to both overall discrimination and individual harassment. However, previously each representative of minority groups could experience discrimination in particular dimensions of life such as job applications, healthcare, criminal justice system, education that are more systemic at this point, while returning to communities they could have regained support from each other to maintain positive attitudes that contribute to the personal growth and reduction of stress. It reminds me of Jane McGonigal’s performance regarding the post-traumatic growth where she has developed a game approach called “Superbetter” with the stages of recruiting allies, battling the bad guys and activating the power-ups (Rousseau, Module 1, 2023: 8). This is why the past is full of motivational stories of success among African Americans starting from sports, music/entertainment industry and finishing with politics. Conversely, today the world has shifted towards the implementation of advanced technology and spread of social media that made us accessible and visible wherever we are, unless we are connected to the Internet. The space without time and territorial boundaries established the new reality where it has become possible to freely express your opinion on everything, while reaching everyone with a distance of one click. While we are at home, in our workplace or in the restaurant with our friends, we are exposed to people’s judgments online via their posted comments. Thus, I claim that racism and ethnoviolence has received a new form of manifestation in the cyber environment: this is the hateful speech online against minority groups or particular ethnic groups that tends to tremendously contribute to the alienation of individuals, developing an existential crisis followed by PTSD symptoms.
The controversy of the given issue is that minority groups are being targeted by users online being exposed to traumatic non-stop experiences without proper protection by law enforcement. This occurs due to the First Amendment in the US Constitution where basically oppressive comments are being covered by the freedom of speech: “Congress shall make no law respecting an establishment of religion, or prohibiting the free exercise thereof; or abridging the freedom of speech, or of the press; or the right of the people peaceably to assemble, and to petition the Government for a redress of grievances”. This fact makes victimized people accept their struggles on a daily basis, while entering a cycle of psychological abuse and accumulating all possible post traumatic symptoms. Now, hateful speech can be considered as “words that wound”, even though as it was stated there is no direct physical violence applied. The amount of hate exposure measures the extent of trauma that we eventually get. Thus, it is necessary to know how this procedure works. First, what provokes the danger to happen is the fact that Internet forums / social media shape a digital relationship between anonymous or pseudo-anonymous users, suitable targets for hateful or defamatory messages and the ISP (the Internet Service Provider) that serves as a gateway (Nel, 2007: 193-195). Interestingly, anonymity in this relationship is a variable that enables one’s identity to be concealed for enjoying the social benefit of privacy and free speech (according to the First Amendment in the US jurisdiction) but simultaneously creates a hole in the protection of an individual’s inalienable rights, in particular, the freedom from discrimination and degrading treatment. Meanwhile, a suitable target as a variable falls into the received gap, precisely, focusing on the category of minority groups. The interaction online starts as a regular comment/post, then grows into a hateful message and finally reaches its climax at subsequent hate speech. This leads to a research question: can we balance the rights of free speech belonging to a user and the rights of equal treatment and personal security that are inherently owned by a targeted victim online (Universal Declaration of Human Rights, 1948: Articles 1-5)? The lack of this balance currently results in the deprivation of individual dignity with a subsequent increase in dehumanizing victims since what exactly is targeted in minorities is their personal profile (sexual identity, race, religion, etc), leading to damage of their psychological state, brain or other irreversible outcomes such as alienation, loneliness, despair and finally, suicidal thoughts.
In the settings of the current unstable political climate, I would like to illustrate how this phenomenon affects not only racial minorities but also larger populations of ethnic groups. Once the Russian-Ukrainian conflict started, a lot of social media such as mainly Facebook and Instagram exploded with the amount of hateful comments regarding Russians being all killers and aggressors, even though from the ongoing events not all the country’s population supported the invasive actions of the government. Comments by users contained violence and threats where the main message was that “Russian nation should be eradicated”. For this reason, the Russian authorities took a decision to prohibit Instagram in the Russian jurisdiction, claiming that it is violence-oriented platform trespassing on the individual dignity of citizens. Personally being of Russian origin, even though I was not directly affected by hateful comments (since I limit my participation in the digital daily routine), I received vicarious trauma from reading the hate from thousands of users. As a regular civilian, I couldn’t understand why they wanted me to die just for being ethnically who I am, while I am not even closely related to the ongoing military actions. My trauma started growing from the fact that I did not want to answer questions regarding my descent because I did not want to be judged and finished with self-blaming why I happened to be born as Russian. This journey of trauma demonstrates that I entered the existential crisis, started being confused about who I am since my ethnic background was questioned. Consequently, racism and ethnoviolence tend to break mentally individuals, and if this experience is uniquely new for them, they may not be familiar with how to handle their feelings and opt for silence.
To conclude, I chose racism and ethnoviolence as an overlooked type of accelerators for trauma among racial minorities and ethnic groups. Even though the scholarship is cautious with these issues due to subjective interpretations, the research revealed that harassment may exacerbate PTSD symptoms compared to passive discrimination. However, I claim that today we experience a new catalyst of traumas which is hateful speech online due to the advent of advanced technology and the Internet. I find the given event anti-spatial and diffusing, meaning that it can contribute to people’s exposure to oppression and trauma anywhere anytime, without any right to escape. I have also commented on the contentious lack of legal protection that makes racial minorities and ethnic groups vulnerable and thus more swiftly exposed to the gain of traumatic experiences and development of PTSD symptoms since they enter an existential crisis that is characterized as the confusion of identity. Thus, identity is the main targeted asset that perpetrators aim for to humiliate victims. With assistance of the personal example of online ethnoviolence, I demonstrated how the given relationship operates and which directions trauma may take if being overlooked. To combat the given issue, I think we should find the balance in how to ensure “digital security” on a legal level by avoiding excuses such as freedom of speech since this phenomenon cannot cross somebody else's boundaries, otherwise it takes the form of injustice. Furthermore, I believe that we should invest more resources in educating people’s digital literacy because sometimes the reason why individuals do not report their PTSD symptoms is because they do not realize that they have them just because of constant exposure to stress, violence and discrimination online. The more awareness is being shaped on this problem, the more people or their relatives, community members may recognise the need for help to prevent the development of the given symptoms in advance.
References
- Helms, J., Nicolas, G., & Green, C. (2010, January 01). Racism and Ethnoviolence as Trauma: Enhancing Professional Training. Traumatology, 16(4) 53-62.
- Nel, S. (2007). Online Defamation: The Problem of Unmasking Anonymous Online Critics. The Comparative and International Law Journal of Southern Africa, 40(2), 193–214. http://www.jstor.org/stable/23252662
- Rousseau, D. (2023). Trauma and Crisis Intervention. Module 1. Introduction to Trauma. MET CJ 720. Boston University.
- U.S. Constitution - First Amendment | Resources | Constitution ... (n.d.). https://constitution.congress.gov/constitution/amendment-1/
- United Nations. (n.d.). Universal Declaration of Human Rights. United Nations. https://www.un.org/en/about-us/universal-declaration-of-human-rights
Community Trauma
As this course, along with the rest of the courses for this term close to an end, I’m often thinking about how my courses relate to each other and the real world. One thing that I have been left thinking of is trauma, and how traumatic events affect the community. In one of my other courses, I am looking at aggravated assault incidents, drug related crimes and poverty within a city. Looking at all of this data has left me wondering how communities that are constantly experiencing traumatic events cope, or if they just view it as their new normal. Communities who experience traumatic events once, whether that be neighborhoods that are experiencing an act of violence such as a homicide, or on the larger scale such as the events of 9/11 or the Boston Marathon, seem to be shocked to their core after the events that have happened, and these are usually broadcasted all throughout the media. What about communities who constantly, or on a more continuous basis, experience trauma? Do they build their own subculture around this trauma, and have it become their new normal? Or is it still traumatic every time an event happens, even though they happen frequently?
If you look at this on an individual basis, everyone reacts to trauma differently. With constant exposure to traumatic events, some people continue to view these events as traumatic, while others become desensitized to them. When looking at the community level, how do we support them as a whole? If a whole community is desensitized from all of the trauma they have experienced, how do we treat that at the community level, especially if that is the only normal that the community has ever known? Some responses to this might be to maybe open a neighborhood center where the kids within the community have somewhere to go, or to work on lowering the crime rates in the area.
The Trauma of Incarceration
One of the readings I found to be most interesting this semester was The Trauma of the Incarceration Experience as it discusses a topic I had previously written about in my documentary review. This reading describes the trauma inmates face in the prison system. With over 10 million individuals being incarcerated at any given time world wide, the rates of traumatic experiences and mental health issues that prisoners face are quite high (Piper & Berle, 2019, pg. 1). It is common for people who have been incarcerated to describe unimaginable violence and horrors that they have witnessed during their time in jail. Both DeVaux and Browder described witnessing violence, and both had experiences where defending themselves from violence led to them facing solitary confinement. These experiences that inmates face can lead to things such as PTSD, as an article from 2019 found that “Research examining PTSD in incarcerated populations reported estimates at a staggering 48%, compared to lifetime prevalence rates of 8.7% in the general US population” (Piper & Berle, 2019, pg. 2). These rates emphasize the need for trauma informed care in the carceral system in the United States. Providing trauma informed care to people who are incarcerated could be incredibly beneficial to their mental health, and decreasing recidivism rates.
For the documentary review I watched Time: The Kalief Browder Story. It’s a documentary about Kalief Browder who was 16 years old when he was falsely accused and arrested for stealing a backpack. He was sent to Rikers Island where he was frequently beaten and put in solitary confinement for a majority of the 3 years he spent in jail. He struggled immensely after being released due to the trauma he faced while being incarcerated, and at the age of 22 he committed suicide. His story highlighted the trauma inmates face in prison, and this article also describes a first hand experience of trauma in the carceral system. A quote that I found incredibly important from The Trauma of the Incarceration Experience was that “The experience of being locked in a cage has a psychological effect upon everyone made to endure it. No one leaves unscarred.” (DeVaux, 2013). Kalief also described the impact that incarceration has on everyone that faces it, and the lack of support given to him while he was incarcerated during his as an activist. This article by DeVaux explains how “people in prison may be diagnosed with posttraumatic stress disorders, as well as other psychiatric disorders, such as panic attacks, depression, and paranoia; subsequently, these prisoners find social adjustment and social integration difficult upon release” (DeVaux, 2013). Prison can cause long lasting mental health issues, and oftentimes these issues are not treated while in prison, making the adjustment back into the community more difficult.
During Browders time at Rikers Island, he experienced a severe mental health decline, and despite begging prison officials for help and treatment, his pleas were ignored. Despite the fact that treatment for him could have been life saving, he was denied help multiple times, causing his suffering to worsen. Kalief spent 700 days in solitary confinement, which accelerated the rapid decline of his mental health. According to Chadick et al, those in solitary confinement “typically spend 22–24 hrs of isolation with approximately 1 hr allotted for exercise or shower each day; some facilities only allow shower time three to 4 days a week” (Chadick et al, 2018, pg. 2). As social creatures, this isolation can have severely detrimental impacts on inmates and their mental health. A study from 2001 looking at the impact that solitary confinement (SC) has on mental health found that the “Incidence of psychiatric disorders developed in the prison was significantly higher in SC prisoners (28%) than in non-SC prisoners (15%). Most disorders were adjustment disorders, with depressive disorders coming next” (Anderson et al., 2001). They found stress to be a major contributing factor, which oftentimes prisoners in solitary confinement experience extreme levels of stress in isolation. Chadick et. al stated that prisoners in solitary confinement often “experience a myriad of mental health concerns and symptoms, including appetite and sleep disturbance, anxiety (including panic), depression and hopelessness, irritability, anger and rage, lethargy, psychosis, cognitive rumination, cognitive impairment, social withdrawal, and suicidal ideation and self-injurious behaviours” (Chadick et al, 2018, pg. 2). Implementing trauma informed care in our prison systems could be beneficial because “ all staff can play a major role in minimizing triggers, stabilizing offenders, reducing critical incidents, de-escalating situations, and avoiding restraint, seclusion or other measures that may repeat aspects of past abuse” as the prison setting is full triggers that could be impacting the mental health of inmates (Miller & Najavits, 2012).
Kalief also described post-release how difficult it was for him to adjust and integrate back into society. He was enrolled in college before his passing, but it was something he really struggled to adjust to due to the trauma that he faced. With trauma-informed care and better support during his transition from jail back into the community, Kalief could have had the support he needed in order to adjust smoothly and thrive post release. He struggled for the remainder of his life due to the trauma and lack of support he faced during his time in jail, but spent the remaining time after his release advocating for better treatment of those who are incarcerated. The trauma that both of these men faced during their time in jail is something that impacted them for the rest of their lives. I had watched the Kalief Browder documentary when it first came out in 2016, and it was just as impactful to watch now as it was the first time I saw it. Devaux’s experience in the system is incredibly similar to Browder’s, and unfortunately many others have had similar experiences. Kalief described the same paranoia that Devaux had, and both also described witnessing and experiencing unimaginable violence. Kalief’s story was one of the first times I had realized the trauma inmates face in the system, and this article gave me an even better insight and understanding as to how the carceral system facilitates traumatic environments for inmates.
Resources:
Andersen, H. S., Sestoft, D., Lillebaek, T., Gabrielsen, G., Hemmingsen, R., & Kramp, P. (2000). A longitudinal study of prisoners on remand: psychiatric prevalence, incidence and psychopathology in solitary vs. non-solitary confinement. Acta psychiatrica Scandinavica, 102(1), 19–25.https://doi.org/10.1034/j.1600-0447.2000.10200
Chadick, C. D., Batastini, A. B., Levulis, S. J., & Morgan, R. D. (2018). The psychological impact of solitary: A longitudinal comparison of general population and long‐term administratively segregated male inmates. Legal and Criminological Psychology, 23(2), 101–116. https://doi.org/10.1111/lcrp.12125
DeVeaux, M. (2013). The trauma of the incarceration experience. Harvard Civil Rights–Civil Liberties Law Review, 48
Miller, N. A., & Najavits, L. M. (2012). Creating trauma- informed correctional care: a balance of goals and environment. European journal of psychotraumatology, 3, 10.3402/ejpt.v3i0.17246. https://doi.org/10.3402/ejpt.v3i0.17246
The Importance of Self-Care for Law Enforcement Officers
Matthew S. Paradis
It is no secret that law enforcement officers are repeatedly exposed to stress and trauma throughout their careers. The cumulative stress and/or PTSD can wreak havoc on the overall health of an officer, especially if left unmanaged. Police officers generally experience higher rates of depression, PTSD, burnout, and anxiety when compared to the general population (NAMI). They also commit suicide 54% more than the general population (Violanti, 2020). This number is exacerbated when considering small departments, as this rate increases to over three times the national average” (NAMI).
There are many contributing factors to these statistics and yet despite knowing the statistics, the underlying problems persist. Police officers are tasked with solving or addressing many societal problems and yet they are hesitant to address their own. Barriers exist that discourage or prevent officers from seeking out help, even if they recognize that they are having difficulties with PTSD or some form of mental illness. More importantly, there is a stigma surrounding officers and emotional and/or psychiatric conditions, such as fear of losing their job, having their ability to carry a firearm taken away, reassignment to a less “stressful” position, and being labeled as weak and eliciting ridicule, humiliation, and retaliation from fellow officers or administration (Rousseau, Module 6).
In light of the ominous statistics previously discussed, there are viable options to help address the underlying issues at hand, mainly in the form of self-care. While officers are hesitant to seek assistance, exercising various forms of self-care can be incredibly beneficial to an officer’s overall health and well-being. Simplistically, officers should do their best to get adequate sleep, exercise regularly, eat well, do their best to relax, and connect with those who they have meaningful relationships with, particularly significant others. These areas need to be prioritized by officers who wish to continue to enjoy their lives and their careers rather than just going through the motions. These things must be done with purpose and in doing so, officers may find themselves in a better position to serve others to the best of their ability.
When the oxygen masks come down in an airplane during an in-flight emergency, flight attendants advised passengers to take care of themselves first before taking care of others. This same principle holds true with police officers prioritizing their own health (Cordico). Whether it be yoga or some other type of physical exercise, practicing mindfulness, journaling, finding a hobby, speaking with a mental health professional or peer support, or some combination of these strategies or others, police officers need to champion their own health and in doing so, they will be better suited and equipped to effective manage what the job will throw at them and be in a position to serve their families and communities to their best of their abilities. Self-care can provide a sense of personal control in an otherwise chaotic world, allowing us to pursue meaningful endeavors and engage in healthy lifestyle choices, supporting personal growth and furthering our resilience to the stress and trauma inherent in policing (Rousseau, Module 1).
Greco, N. (2022, March 4). The importance of self-care for law enforcement. Cordico. https://www.cordico.com/2021/05/21/take-care-of-yourself-why-law-enforcement-officers-need-self-care/
National Alliance on Mental Illness. (2023). Law enforcement. NAMI. https://www.nami.org/Advocacy/Crisis-Intervention/Law-Enforcement
Rousseau, D. (2023). Module 1 - Introduction to Trauma. MET CJ720. Boston University.
Rousseau, D. (2023). Module 6 – Trauma and the Criminal Justice System. MET CJ720. Boston University.
Violanti JM, Steege A. Law enforcement worker suicide: an updated national assessment. Policing. 2021;44(1):18-31. doi: 10.1108/PIJPSM-09-2019-0157. Epub 2020 Oct 21. PMID: 33883970; PMCID: PMC8056254.
Can Playing Dungeons & Dragons Be a Trauma Treatment Tool That Bridges the Victim-Offender Overlap?
It’s close to midnight when your party enters the roadside inn half a mile outside of the town of Waterdeep. You’re a rogue and thief wanted for murder, so you conceal your face. While your friends make their way over to the bar, you slink into a booth in the darkest corner of the dining room. As you note all the possible exits in the building, a waitress meets your gaze and begins to make her way over to where you are sitting. Before she can get close, two strangers block her path and start speaking to her in hushed but insistent tones. You succeed in rolling a perception check. The waitress seems extremely distressed, and you hear her say, “I said ‘no,’ now leave me alone.”
You’re a rogue and a thief. It would be best if you didn’t make a scene, but your character sheet also says that part of your background is that your family abused you, and you vowed never to let an innocent person be hurt by someone else. Your friends are distracted at the bar and don’t see the woman who needs help. It’s up to you. You roll a successful intimidation check and put a hand on the shoulder of one of the aggressors. “She asked you to leave,” you say. Thankfully, the strangers leave the inn, only looking a little annoyed. “Thank you,” the waitress says, stopping short when she sees you more clearly. Recognition flashes across her face. “It’s you!” Well, here it comes, you think. Off to jail, again. “Everyone, everyone!” she says, “It’s The Savior of Baldur’s Gate! Get this hero a drink!!” Oh yeah, you remember, I guess we did save that city a few sessions ago. Word travels fast.
~
In the first discussion post for this course, I was instantly drawn to van der Kolk’s (2015, p. 17) observation about imagination: “Imagination is absolutely critical to the quality of our lives [and] it is the essential launchpad for making our hopes come true.” From victims of child abuse using sand to play and act out narratives that they may not remember the words for (Rousseau, 2023b, p. 16) to veterans of war struggling to see peaceful images in inkblots (van der Kolk, 2015, p.16) to offenders of horrific crimes having to live with the trauma of institutionalization on top of learning to live a crime-free life (Rousseau, 2023c, p. 15), imagination is the most essential tool to build resilience in environments where inspiration is in short supply.
While the story I wrote above might seem goofy to you as the reader, I believe that as the player, and as your own main character, the choices you make and the actions you take can be exhilarating, and important at the very least. This is why I think we love knowing a little bit about our star sign, and why we take all those surveys that tell us which character of whatever TV show we would be. This can be a fun reverie for anyone, if, of course, your horoscope says you’re going to win the lottery and you’re most like the protagonist, hot girl, cool guy, etc. For people who may avoid their past or find that they are unable to leave their past behind them, I believe games, like trauma-informed Dungeons & Dragons (D&D), can be used to practice imagination, act as a complex form of talk, group, and exposure therapy, and instill a long-lasting resilience in people who have experienced many different forms of trauma and chronic stress.
If you’re unfamiliar with D&D, this is a great synopsis of the game, written by Blakinger (2023), who interviewed inmates on death row who used the game to cope with their death sentences: “[D&D is a] tabletop role-playing game known for its miniature figurines and 20-sided dice. It combines a choose-your-own-adventure structure with group performance[.] Participants create their own characters — often magical creatures like elves and wizards — to go on quests in fantasy worlds. A narrator and referee, known as the Dungeon Master, guides players through each twist and turn of the plot [with] an element of chance.”
Before you discount me completely, remember that playing games that improve our “physical, mental, emotional, and social resilience” can add years to our lives (McGonigal, 2012; Rousseau, 2023a, p. 8) and individuals who have experienced trauma and chronic stress may already have had the physical effects of stress take years off their life (Rousseau, 2023a, p. 4). Rousseau (2023a, p. 4) lists “uncertainty, loss of control, and a lack of information” as factors that trigger stress. It is unrealistic to imagine a future in which none of these factors occur, but the human body’s response to stress (van der Kolk, 2015) calls for treatment in safe spaces where we can learn how to deal with this natural response to past trauma. With every roll of the dice, the success of your decisions in this game is left completely to chance, but the player is always in control of what they decide to do and how they respond to successes and failures. While there is a lack of information, the Dungeon Master knows everything about this fantasy world. There are boundless opportunities to learn, explore, and discover the unknown.
In addition to the safe space that this game creates as a practice zone to cope with stress and possibly even face one’s fears, I believe that D&D can also be used as a tool for reclaiming positive narratives and labels, particularly for offenders. Labeling theory states that “people become stabilized in criminal roles when they are labeled as criminals” (Cullen et al., 2022, p. 7). A tool known as “redemption scripts” (Cullen et al., 2022, p. 248-250) has been used in efforts for people to discover their “true selves” or the best parts of them that could be the foundation for a crime-free life. I believe with guidance from a therapist or other trained mental health professional, the character creation portion of this game, which often takes place one-on-one and before the roleplaying part of the game, could be beneficial to offenders seeking a personal label change.
While this is just a brief exploration of this idea, it would be very interesting to see how resilient trauma-impacted individuals both inside and outside of prisons were after just a few sessions of playing D&D, and if they thought about their fantasy adventures outside of the sessions at all, and in what way. If you’ve never played D&D, I understand it might be confusing to think about how powerful this game can be. But, before you go, please look at the picture below. This is a D&D character sheet. It’s what you fill out for the character you play during the game. This is where you list your character’s strengths, weaknesses, background, personality, and if you’re inherently good, bad, or just straight chaotic. If you have a moment, read the categories on the sheet, and think about two things: 1. What would this sheet look like if I were the character in the story? Particularly, what would the four categories on the righthand column say? And 2. If I could be anyone, my true self, what would it say then?
Thank you very much for keeping an open mind, maybe learning more about something new, and considering my perspective!
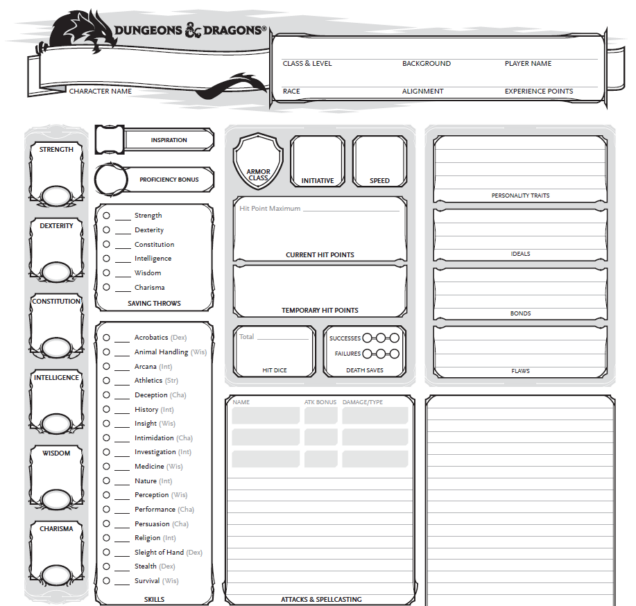
(D&D Blank Character Sheet, 2023).
References
Blakinger, K. (2023, August 31). When Wizards and Orcs Came to Death Row. The Marshall Project. Retrieved December 11, 2023, from https://www.themarshallproject.org/2023/08/31/dungeons-and-dragons-texas-death-row-tdcj
Cullen, F. T., Agnew, R., & Wilcox, P. (2022). Criminological theory: Past to present (7th ed.). Oxford University Press.
D&D Blank Character Sheet [PDF]. (2023). Wizards of the Coast. Retrieved December 11, 2023, from https://dnd.wizards.com/resources/character-sheets
McGonigal, J. (2012, June). The game that can give you 10 extra years of life. TEDGlobal 2012. Retrieved December 11, 2023, from https://www.ted.com/talks/jane_mcgonigal_the_game_that_can_give_you_10_extra_years_of_life
Rousseau, D. (2023a). Trauma and Crisis Intervention Module 1. Retrieved December 11, 2023, from Blackboard [url].
Rousseau, D. (2023b). Trauma and Crisis Intervention Module 2. Retrieved December 11, 2023, from Blackboard [url].
Rousseau, D. (2023c). Trauma and Crisis Intervention Module 6. Retrieved December 11, 2023, from Blackboard [url].
van der Kolk, B. (2015). The Body Keeps the Score: Brain, Mind, And Body in the Healing of Trauma. Penguin Books.
Haitian Resilience, Natural Disasters & COVID-19
During the course, I read a piece by Guerda Nicolas about Haitians coping with the traumas associated with natural disasters and their resilience. Several post-disaster studies have found that there was notable prevalence of post-traumatic stress disorder (PTSD) and depression in the Haitian population. They have faced many political, economic, and environmental storms to include natural disasters (Nicolas et al, 2014, p. 93). Nicolas (2014) argues that the sociocultural traditions and customs of the Haitian people, family, religion, and community, are the reason for their resilience in the face of disaster.
Some refer to the COVID-19 pandemic and its aftermath as a “collective trauma,” defined as the “psychological response of an entire group to a traumatic event, such as the Holocaust” (Kaubisch et al, 2022, p. 28). From a psychological point of view, the threat of serious illness or death, the loss of jobs, the increased stress, the disruption in daily lives, the growing uncertainty, and the disconnect and isolation generated by the pandemic led to the consideration of COVID-19 as a traumatic event. Research suggests that one in five people could experience psychological distress post-COVID-19, such as depression, anxiety, and PTSD (Kaubisch et al, 2022, p. 27).
Prior to COVID-19, Haiti had just lifted restrictions from a political lockdown that had lasted almost a year and the country was also experiencing violent civil unrest triggered by an abrupt increase in fuel prices, a movement that became known as Peyi Lòk (Blanc et al, 2020). “When the first case of COVID-19 arrived in March 2020, the country was just beginning to regain a certain sense of normalcy despite the socio-economical and psychological ramifications of being on lockdown” (Blanc et al, 2020). Majority of the Haitian population continued to live their daily lives, as they were desensitized to the effects of disruption and forced isolation and distancing. Within three months, COVID-19 in Haiti had reached its peak and there was a decrease in the number of detected cases, predicting that the damage of the pandemic would not be too devastating to the country (Blanc et al, 2020).
It is argued that other countries, such as the United States, could learn from the Haitian experience of coping with traumatic events. Resilience is possible after exposure to trauma. Factors that promote posttraumatic growth are “positive social support, gratitude, strong family ties, attachment, and meaning making, or the way in which a person interprets or makes sense of life events” (Rousseau, 2023). The country of Haiti was created after the only successful slave insurrections in history and the resilience of that revolution threads through its history of tremendous struggles.
References:
Blanc, J., Louis, E.F., Joseph, J., Castor, C., & Jean-Louis, G. (2020). What the world could learn from the Haitian resilience while managing COVID-19. Psychological Trauma, 12(6), 569–571.
Kaubisch, L.T., Reck, C., von Tettenborn, A., & Woll, C.F. (2022). The COVID-19 pandemic as a traumatic event and the associated psychological impact on families – A systematic review. Journal of Affective Disorders, 319, 27–39.
Nicolas, G., Schwartz, B., & Pierre, E. (2014). WEATHERING THE STORMS LIKE BAMBOO: The Strengths of Haitians in Coping with Natural Disasters.
Rousseau, D. (2023). Module 1: Introduction to Trauma. Blackboard.
Overcoming Barriers to Trauma: Rural Women Facing Domestic Violence
Riley A. Thomas
Considerations surrounding rural and sparsely populated America and its criminogenic nature are overlooked. Therefore, much needed attention on rural centric crime considers factors not applicable to the urban. This fact may be related to issues that make society as a whole precieve rural criminology less important than metropolitan areas (Ceccato, 2018), where a majority of the American population lives. Therefore, a much greater emphasis and attention is needed for victims of traumatic crimes in rural areas due to the spatial differences than percieved mainstream criminology.
Aspects such as limited access to services, isolation, poverty, and rural cultural values make rural women more vulnerable to domestic violence than women living in urban areas (Ceccato, 2015). This post will mainly focus on rural women who suffer from intimate partner violence (IPV), and the geographic challenges of recieving treatment or support outside of the immediate area.
Examining intimate partner violence in this case is significant because it can be evaluated as one of the most underreported figures of crime. For example, Ceccato (2018) identifies that physical isolation may also lead to a disproportionately high declared fear of crime
because of individuals’ relative vulnerability. For a variety of reasons, women and victims of IPV may fall silent due to public perceptions, shame, guilt, or embarassment to name a few (van der Kolk, 2014). Reagrding trauma related to IPV, rates for violence against women vary geographically, making it difficult to untangle underreported cases between rural and areas (Ceccato, 2015). Additionally, the cohesive nature of rural areas adds another dimension of trauma support avoidance.
This consideration of a cohesive system stems from smaller communities being well versed with eachother, and the events that take place within the community. In other words, everyone knows everyone, and collective efficacy is rarely thrown off balance. Knowing this, woman may avoid support for their trauma with the fear of being ostracized by speaking out on violence, which may have the unintended effect of enabling domestic violence, and the inability to seek help for IPV trauma (Ceccato, 2015).
Knowing this the geographical difficulties of seeking help in rural IPV and trauma cases still remain prevalent. For example, rural communities and towns are in far geographical areas from metropolitan areas with greater support systems. In other words, long distances create isolation to a greater degree than urban areas (Ceccato, 2015). With these outlets out of reach, rural communities may lack the resources and support systems and highly populated areas have. This can lead to victims of trauma and IPV staying silent, since breaking the efficacy and cohesion of their community can have drastic effects on the abuser and the victim. The lack of support systems for women in rural areas can contribute for women to stay in their traumatic situations. Victims of traumatic domestic violence often cover up their abusers (van der Kolk, 2014) for a variety of reasons. Here, I can assume because of the limited access to getting treatment, and the unwillingness to face public embarrasmenterassment. Since the cohesive nature of small communities may put these victims of trauma in the shadows.
This post considers the challenges rural women may face when dealing with IPV and seeking treatment for their trauma. Knowing the spatial differences between the rural and the urban seek out potential barriers for women to attain the help that they need, due to factors such as isolation and reliance on their domestic partner. An attention on rural centric crime considers factors not applicable to the urban, and must be researched further to understand the hidden figures and perception of rural life.
Ceccato, V. (2015b). Rural crime and community safety. https://doi.org/10.4324/9780203725689
M.D., B.V.D. K. (2014). The Body Keeps the Score. Penguin US. https://bookshelf.vitalsource.com/books/9781101608302
Approaches to Childhood Trauma
I have always found the psychology of children a fascinating topic because much of our habits, actions, and language developments occur during our childhood years. So, I was excited to learn more about childhood trauma; more specifically, how children are impacted by trauma. Unlike adults, children experience, express, and cope with trauma differently compared to adults. Because of this, psychologists and psychiatrists have had a hard time recognizing and managing children who experience trauma. Although there are many tests to help guide these professional workers in diagnosing these children. In the documentary “PTSD In Children: Move in the Rhythm of the Child” directed and produced by Joyce Boaz, she highlighted the idea that there are children who are experiencing trauma who seek interventions, but there are children do not seek interventions. Children are vulnerable to their surroundings and their environment due to their sensitive nature. Trauma does not only change their perceptions of the world but also changes their neurobiological development (Rousseau, 2023).
A biology approach to childhood trauma:
Kolk’s chapter on “Developmental Trauma: The Hidden Epidemic” discusses the idea that trauma and stress may be involved in a more-than-just environmental impact, but rather could be a transfer of genetic makeup to progeny generations (Volk, 170). This idea is not a new idea, with understanding if our genes give rise to certain behaviors and traits. However, strong research has also found the importance of epigenetics which can certainly change behaviors (Kolk 2015).
Currently, I am taking a course in Animal Behavior, and one of the case studies we looked at is the idea that genetics influences an individual's primary response, however, epigenetics (aka the impact of the environment on our DNA) can change this primary response. Similar to Szyf’s words, “major changes to our bodies can be made not just by chemicals and toxins, but also in the way the social world talks to the hard-wired world.” (Kolk, 2015)
A social approach to childhood trauma:
Now that we discovered the idea that trauma may impact a child differently depending on their innate genetic information, different children will respond and react to trauma differently. The “hard” part of this is how researchers can determine this. In Boaz’s documentary, she introduced us to multiple psychiatrists who specialize in treating children who have experienced trauma, and a consensus that all the psychiatrists agreed on is that children are hard to read. Sometimes they are unable to identify and express their feelings, and for this, therapeutic tools as well as diagnostic tools have been implemented to assist psychologists and psychiatrists to help with diagnosis and treatments. In our course, we looked at multiple different therapeutic tools including the art of yoga project, Sand Tray Therapy, and Trauma-Informed Behavioral Therapy (Rousseau, 2023).
These tools and approaches are important for early interventions of children who experienced trauma, but I do want to recognize children who are unable to find interventions. The ACE study (Adverse childhood experiences) found with a sample size of 50,000 patients that:
* One out of ten adults responded that he/she was a victim of some form of emotional abuse.
* More than one-quarter of respondents were victims of some form of physical abuse.
* Twenty-eight percent of the adult women and sixteen percent of the adult men responded that they were victims of some form of sexual abuse.
* One in eight of the adults responded that he/she witnessed his/her mother being a victim of abuse.
(Taken from Rousseau 2023)
In simple terms, trauma impacts a lot of children, and it continues to impact millions of children through different routes such as domestic abuse or school bullying. From 2021-2022, a total of 327 documented school shootings have occurred in US elementary to high school (National Center for educational statistics, 2023). This speaks words to not only the individuals who are causing the school violence but also individuals who experience the school violence. Domestic abuse has also been coined as a public health issue. Intervention is only provided when an individual seeks it, so I find it extremely disheartening for those who cannot seek it or don’t know how to seek it. Although there are many techniques and therapies involved, at the end of the day, only certain types of individuals can receive it.
References:
National Center for Education Statistics (2023). Violent Deaths at School and Away From School, School Shootings, and Active Shooter Inceidents. Retrieved December 9, 2023, National Center for Education Statistics. https://nces.ed.gov/programs/coe/indicator/a01/violent-deaths-and-shootings
Boaz, J. (Director + Producer). (1995). PTSD In Children: Move in the Rhythm of the Child.
[Video/DVD] Gift from Within. https://video-alexanderstreet-com.ezproxy.bu.edu/watch/ptsd-in- children-move-in-the-rhythm-of-the-child/details?context=channel:counseling-therapy
Rousseau, D. (2023). Trauma and Crisis Intervention Module 1. Retrieved November 20, 2023,
from Blackboard.
Van der Kolk, B. (2015). The Body Keeps the Score: Brain, Mind, And Body in the Healing of
Trauma. Penguin Books.