The Real Cost of COVID-19: The Fractured Health Care System
The coronavirus (COVID-19) pandemic has uprooted the very foundation everyday life, turning socialization into a moral evil, and weaponizing safety precautions as political propaganda. These clear immediate costs, amounting in the loss of life, jobs, and social pleasures, are merely the surface to a rather elaborate system of institutional market failures that are bound to follow. While the coronavirus promptly began a long-awaited economic recession, forcing more than 31 million people in the United States to file for unemployment insurance, there has been a catastrophic loss of employer based health insurance coverage for many individuals, leaving only those who are eligible and qualified to move over to Medicaid or other subsidized health insurance policies. Unfortunately many have found themselves stuck in what is known as the “coverage gap,” with health care access becoming a novelty when its demand is at an all-time high.
Hospital and Insurance Coverage Crisis
Hospitals are largely believed to be price inelastic institutions, where demand for health services will remain constant, and funds will continuously keep providers operational even during economic recessions. While one might think that the COVID-19 public
health crisis would drive health care consumption, benefiting hospitals, it has actually been quite the opposite. Demand for healthcare services has been primarily for expensive specialized care, imposing high out-of-pocket expenses on individuals who are treated for COVID-19, and has further shifted from routine visits, seeing reductions as high as 60%.. The increased costs in specialized care, combined with the decrease in less costly routine care has not been the only shock to the health care industry. Additionally, by April of 2020, 1.4 million health care jobs were lost to enable hospitals to produce positive profit margins, creating staffing shortages across many US hospitals. This, paired with over 40 million Americans losing their jobs and shifting to subsidized healthcare and Medicaid, has created a loss of up to 20% of the commercial insurance market. By decreasing those covered by commercial insurance plans, cost aversion behaviors will decline health care usage, and those who are eligible will move over to Medicaid. Shifting from private to public insurance at this rate will cost Hospitals $95 billion in annual revenue. While Hospitals are experiencing adverse pressure, threatening what was believed to be recession proof industry, it is merely one of the many cracks that make up an unsustainable health care system.
The CARES Act and FFCRA’s Truncated Effect on the Health Care Crisis.
The passage of both the Coronavirus Aid, Relief, and Economic Security Act (“CARES Act”) and the Families First Coronavirus Response Act (“FFCRA”) has provided economic stimulus and safety protocols to expand health care access. These measures have covered COVID-19 diagnostic testing, mandating the elimination of cost-sharing, such as co-payments, deductibles, and coinsurance, for a wide array of group health plans and insurances. While this improves accessibility to preventative measures, it leaves open a large regulatory gap for the actual treatment of COVID-19, where individuals are still vulnerable to out-of-pocket expenses until they reach their cap for insurance to kick in, “ exceeding “$8,000 for an individual and $16,000 for a family.” The benefit of expanding access to testing is immeasurable, but the high costs of treatment poses a significant risk to those who are already underinsured. Further, these acts fail to eliminate cost-sharing for the uninsured, which accounts for 27.9 million nonelderly individuals in the US in 2018. While the number of uninsured Americans is certainly alarming, it is a great improvement from the number of uninsured prior to the enactment of the Affordable Care Act (“ACA”), where over 46.5 million nonelderly individuals were uninsured in 2010. Yet, the many positive effects that have followed the enactment of the ACA are at risk of being undone, with the Supreme Court of the United States reviewing four legal questions pertaining to the ACA.
The Uncertainty of Health Care in the face of California v. Texas.
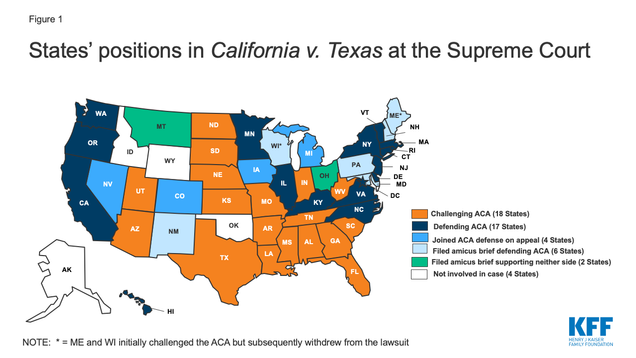 California v. Texas will be a test to the legislative muster of the ACA. With the recent confirmation of Justice Amy Coney Barrett to the Supreme Court, concerns of the ACA being overruled have surfaced as Justice Barrett has claimed that Chief Justice Roberts has “pushed the Affordable Care Act beyond its plausible meaning to save the statute.” The fate of the ACA hinders on whether the individual mandate is unconstitutional, and if so, if the individual mandate of the ACA is severable from the rest of the legislation. If the court does decide to overrule the ACA in its entirety, we may see more than 20 million individuals lose health care insurance, exacerbating the already grim public health crisis brought on by COVID-19, impacting our most vulnerable communities who struggle to gain access to health care.
California v. Texas will be a test to the legislative muster of the ACA. With the recent confirmation of Justice Amy Coney Barrett to the Supreme Court, concerns of the ACA being overruled have surfaced as Justice Barrett has claimed that Chief Justice Roberts has “pushed the Affordable Care Act beyond its plausible meaning to save the statute.” The fate of the ACA hinders on whether the individual mandate is unconstitutional, and if so, if the individual mandate of the ACA is severable from the rest of the legislation. If the court does decide to overrule the ACA in its entirety, we may see more than 20 million individuals lose health care insurance, exacerbating the already grim public health crisis brought on by COVID-19, impacting our most vulnerable communities who struggle to gain access to health care.
Disparities on Minority Care and COVID-19 Infection.
Racial and ethnic minority groups face the greatest barriers to health care access, and, in turn are more likely to be uninsured or underinsured compared to their non-Hispanic white counterparts. While the ACA had greatly reduced the proportion of racial and ethnic minorities who lack health insurance, there are numerous systemic and social hurdles that have left these minority groups uninsured at higher rates than white individuals. As a consequence, racial and minority groups have been disproportionately affected by COVID-19, with racial minorities being over 2.6 times as likely to contract COVID-19, with rate of hospitalization for African American individuals being 4.7 times more than that of white individuals. Not only this, but the mortality rate is 2.1 times that of white people in the US, showing clear disparity in treatment outcomes and access to treatment.
The disproportioned access to health care services from racial and ethnic minority groups, has undoubtedly put these individuals at higher risk to unexpected out-of-pocket expenses, surprise bills, and physical harm from COVID-19. COVID-19 has shed light on the systemic racism in our health care system, unfortunately adding to the already disastrous public health crisis. The many cracks that are forming throughout our health care system will have untold effects on minority populations, and needs to be addressed through comprehensive legislative health care reform that is aimed at providing universal insurance coverage and eliminating implicit biases that contribute to lower standard care.
While the sprawling costs of COVID-19 stand out as clear reminders that we are living anything but a normal life, the true long term costs on minority populations, health care institutions, and health care access is now even more clear as Americans face another wave of COVID-19 outbreaks during these colder months. This cocktail of failures will greatly impact an already fragmented health care system, leaving our most vulnerable communities without proper health care access. Congress and the state legislatures need to secure funding for the providers of our health care services, while also increasing access to health care insurance and treatment for all individuals to minimize the long-term costs associated with COVID-19.
 Kyle Hafkey anticipates graduating from Boston University Schoo of Law in May 2022.
Kyle Hafkey anticipates graduating from Boston University Schoo of Law in May 2022.