Home
Suicidality of Mentally Ill Prisoners
Mental illness can manifest in many different ways such as prolonged depression, excessive fears, worries, anxieties, changes in eating and sleeping habits, social withdrawal, and strong feelings of anger (Rousseau, 2024). It could be argued that these behaviors might go unnoticed in institutions such as prisons, especially given there could be more overt behaviors staff are on the lookout for. While there are checks and balances such as psych evaluations and clinical support in some prisons in most cases those who are mentally ill go ignored within the system (Rousseau, 2024). While in an institution those with mental illnesses are far more likely than the general population to experience thoughts and desires of suicide (Rousseau, 2024). Even if the individual does not complete suicide within a prison, they face integrating back into the "real world" often times with worse mental health than they entered with (Rousseau, 2024). As someone with an undergraduate education in psychology I learned the importance of being mindful of these issues and I believe there is a large issue with unintentional trauma to those with mental illness within the criminal justice system. I do want to emphasize that I do not believe this is intentional behavior on the part of prison staff but human error from people who may not be trained or have not had practice spotting warning signs. Regardless, when these warning signs go unnoticed it causes issues as the individuals mental illness is worsened by interactions with staff or other inmates. These individuals are then released and, in the case of those without parole officers, are left to their own devices where they either commit suicide or continue deviant behavior because no one was able to intervene to assist with positive behaviors or coping skills. If I were to propose a way to intervene I would suggest introductory assessments and release assessments to each prisoner so in the best case they could be referred to a mental health service. I realize this is an "ideal world" suggestion but I believe it would be more effective than needing to flag warning signs along the way and possibly missing someone in need.
Reference:
Rousseau, D., Forensic Behavior Analysis: Module 4 (2024)
Peer Support for Law Enforcement
In this blog post, I am going to address two things. I am going to provide a further explanation of a topic that was covered in class and discuss strategies for self-care. I am a graduate student at Boston University, and I am currently enrolled in Forensic Behavior Analysis (MET CJ 725). I have learned many things from this course and one topic that we covered recently was approach to self-care. This topic hits close to home for me because I am an active police officer and I have been in law enforcement for the past seven years. This career path is challenging and rewarding and there is a lot of pressure and responsibility in this job. However, that is not what I am here to talk about, I am here to talk about the “forbidden” topic that not too many people cared to talk about or admit was true until recently, and that topic is trauma. More specifically, trauma that is experienced by police officers.
Trauma is defined in the Oxford Dictionary as “a deeply distressing or disturbing experience. Now, police officers see the absolute worst that society has to offer and that is just the nature of the job. I have always said, “no one calls the cops to say hello or to invite them over because they are having a great day”. The reality is the police are called for emergencies or to handle abnormal situations that cannot be dealt with civilly. In the past, there was really no room for emotion or at least there was no opportunity for an officer to express their emotions and to admit that they were suffering mentally from what they witnessed or experienced. I mentioned this in class, but it was recently said to me during a training that “no longer are the days of someone saying, suck it up kid, this is what you signed up for”. Police officers are human beings too and to expect people in this profession to not experience some sort of trauma is not fair.
Over the past couple of years, there has been a big push for teams that are called “Peer support groups”. Basically, a peer support group is a team of law enforcement officers (peers) and mental health professionals that make themselves available to their co-workers and to other law enforcement officers who belong to different agencies. The people on this team are there to lend their support, empathy, and anything else that may be needed for the fellow brother or sister that is struggling mentally or has experienced some traumatic event. And because these people are “peers”, police officers tend to feel more comfortable seeking them out and opening up to them. In an article written on the International Chiefs of Police website, there is a quote that says “the biggest choosing of services for police officers is peer support. 3 out of 4 would rather go to peer support than any other kind of services out there” (www.theicap.org). This is huge, because it’s hard to get police officers to open up to anyone about anything because there is the stigma that they need to be tough, both physically and mentally. So the fact that they are willing to open up to their peers finally opens to door for more services and to get these people the help they deserve.
In addition, peer support is not a loosely put together idea that sounds good on paper but is not proven in the field. The COPS office in the Department of Justice has outlined a program that can help establish peer support teams, spanning from the biggest departments to the smaller, more rural departments. In the article “Peer Support for Officer Wellness”, it breaks down why it is important for a peer support team, and it also lays out a roadmap on how to successfully implement this kind of program in any department (www.cops.usdoj.gov).
In conclusion, police officers are people too who experience the same kind of emotions as everyone else. The job of a police officer is rewarding, but it can also be taxing both physically and mentally. Seeking out help is no longer frowned upon. In fact, it’s encouraged. Peer support teams are an important part of this profession, and it is a movement that needs even more recognition than it is currently receiving. It is okay to not be okay. The support is out there.
References:
-https://www.theiacp.org/sites/default/files/2020-10/244736_IACP_NOSI_PeerSupport_p5.pdf
-https://cops.usdoj.gov/html/dispatch/02-2023/OSW_peer_support.html
Self-awareness approaches towards healing of stress and trauma
Life, our existence is nothing more than just a mere condition where we have the rationality and capacity to function. As we go through life, and it’s experiences we get to go through a number of stages that are supposed to teach us everything that we need to know to survive and learn how to live and how to survive in a society that continuously changes and adapts itself to new standards of life, and until death reaches us. These stages are infancy, toddlerhood, preschool years, early school years, adolescence, young adulthood, middle adulthood, and late adulthood. Yet, no one quite clearly can explain the particular events that are going to transpire in your life, and lead you through different pathways where you will encounter numerous obstacles, challenges, and experiences that will make or break you. Experiences that will activate your stress hormones and put them on a loop, sort of an overload, where you will have to know how to grasp and handle emotions, strong emotions that you will not understand clearly that can fog your mental state, as well as physical state. These experiences are led by an uncontrollable factor in everyday life, stress.
As we are all different and unique individuals, our individual experiences cannot be compared, and since that can’t happen, we don’t fully comprehend what another person goes through. Nevertheless, of the situational factor, stress is a universal factor that impacts us on a regular basis. But what is stress? The World Health Organization say that it’s “a state of worry or mental tension caused by a difficult situation…is a natural human response that prompts us to address challenges and threats on our lives. Everyone experiences stress to some degree.”. So, the continuance of this factor in human beings causes an imbalance and ir-regulation that affects the mind, brain, and body.
So, how does stress affect us? When our body is subjected to an event of experience that causes extreme stress or tension our brain secretes stress chemicals and lights the neural circuitry on fire. It sends alerts to the hypothalamus, the one designed to maintain a balanced internal state, that subsequently sends sensory signals to the amygdala. The amygdala, the processor of emotion and behavior, then processes these signals as the image, sounds, smells, taste, and touch of the moment and decides how to interpret that information and what level of danger is perceived. In their connection the autonomic nervous system, the regulator of involuntary physiologic processes, is activated, alongside with the sympathetic and parasympathetic nervous systems. Both of these in their respective ways tackle the fight, flight or freeze response of the body to the stress. Think of it as a car’s pedals that increases in force are for acceleration and decreases in force are for deceleration until to stoppage. And, these signals and responses once activates occur so quickly that the brain doesn’t even know that anything happened and that a response was emitted. Basically, as the events occur fast, the brain is not aware of the cascade of events, as it takes some time to process. So, the sympathetic nervous system stays on, continuously secreting stress hormones (for example, cortisol and adrenaline), thus impacting and aggravating the individual’s overall balance and well-being.
The physiological and psychological states of the individual continuously are being impacted to an overwhelming state, meaning that its effects on the mind, brain, and body reflect themselves, and stand in the way of completing even the simplest tasks, activities, and duties (ex. reading, studying, or working). In addition to, affecting relationships (ex. partners, family and friends), organ and system health (ex. musculoskeletal, respiratory, cardiovascular, endocrine, reproductive, and gastrointestinal systems), nervous system function (various levels of body aches and pain, vasodilation, compromised blood circulation, amongst more), use and abuse of substances (ex. cocaine, opioids, alcohol, and tobacco), anxiety, depression, and much more.
How to reduce levels of chronic long-term stress? Well, throughout time and various cultures different techniques have been established to aid in the debilitating symptoms of trauma induced stress. For example, relaxation responses are a combination of different approaches to light-up a state of relaxation through deep breathing techniques, focusing on calmness, tranquility and serenity, prayer, yoga, tai chi, and more. Another form of response is physical activity and/or movement therapy, for example, through stretching, pilaties, walking, running, swimming, aerobics, and more the body is able to reduce stress hormones and produce endorphins. In addition to, activities that make some individuals “feel alive”, such as dancing, singing, and social interactions with community members. All in all, in the battle to support the health and well-being of the individual, as well as, improve their self-esteem and self-worth.
A new type of exercise that has been found to be a link of connection between the mind, brain, body, and trauma is somatic awareness. It focuses on a bottoms-up approach towards trauma recovery, where instead of talking or exercising the emotions away this approach focuses on “how the body responds to the trauma, and how that in affects the brain” (American Congress of Rehabilitation Medicine, n.d.). Somatic therapy stretching involves intentional body movements during which one focuses their attention on the inner experience of stress, basically letting go those fight, flight or freeze responses. Because when we go through chronic long-term stress due to trauma the body disconnects from itself, and somatic therapy aids in finding calmness, grounding, balance, and it’s an overall great approach of self-care. So, through somatic awareness we get to pay attention to the different sensations and signals that our bodies send us, in addition to, movement, tensions, and breathing practices (Ucrós, G., 2023). It’s a form of understanding your personal experiences of trauma, and how your body responds to it. Practices to engage in one’s somatic awareness are mindful breathing that focus on the quality, depth, rhythm, location, and body movement; mindfulness of habitual movements where one selects a movement to explore and you notice how you feel inside while repeating the movement and connect to your emotions; body-mind centering where using movement, touch voice and mindfulness can re-pattern or re-educate the individual and their relationship with their body and emotions; and the Alexander Technique that through movement and stretching helps bring forwards the awareness of the impact of stress and trauma on the body, amongst more (Cohen, E., 2023).
The importance in assessing chronic long-term effects of stress and trauma is to prioritize the integration of the mind, brain, and body, and connect it with your spirit and ability of awareness; where therapeutic practices and life choices can be embraced in the journey to healing. There is no easy pathway towards health, balance, and resiliency; as there will always be obstacles, challenges, and two steps forward and one step back in the journey of recovery.
References:
American Psychological Association. (March, 2023). Stress effects on the body. https://www.apa.org/topics/stress/body
Cohen, E. (August, 2023). An Introduction to Somatic Stretching. Charlie Health. https://www.charliehealth.com/post/introduction-to-somatic-stretching#:~:text=The%20core%20aim%20of%20somatic,(muscle%20contraction%20and%20release).
Rousseau, D. (2023). Module 3: Neurobiology of Trauma. Retrieved from: MET CJ 720 O2 Trauma and Crisis Intervention Printable Lectures.
Ucrós, G. (February, 2023). Somatic Awareness: Learning how to read your body’s story. Woven Together Trauma Therapy. https://woventraumatherapy.com/blog/somatic-awareness-reading-bodys-story
Van der Kolk, B. A. (2014). The body keeps the score: Brain, mind, and body in the healing of trauma. Viking Penguin.
World Health Organization. (February, 2023). Stress. Web page: https://www.who.int/news-room/questions-and-answers/item/stress#:~:text=Stress%20can%20be%20defined%20as,experiences%20stress%20to%20some%20degree.
Painting Pain Away
Traumatic events alter every aspect of your life. Victims find it hard to discuss what happened to them and tend to keep things to themselves. How do we help someone heal in a unique and comfortable way? For younger victims, how do we get into their minds when they are too scared to speak?
Art Therapy is a way that victims of trauma can express themselves without words. By using art, they can express their emotions and tell their story. According to research, studies have suggested that some traumatic memories are stored nonverbally and may be retrieved through recollections of sensory, affective, visual, auditory, and kinesthetic elements (Campbell, 2016).
An example of this working successfully is “The Body Keeps The Score” by Bessel Van Der Kolk. In this book, art therapy is used to express feelings. In one chapter, a young child witnessed the terrorist attacks on 9/11. He drew the planes crashing, fire and people jumping. The boy added a trampoline at the bottom of the drawing, so next time they could jump onto that. By creating art, he was able to process the event and incorporate his thoughts on how people could be saved next time (in his mind).
Another example from this book is asking a woman to draw a family portrait. Before drawing, she stated “must have had a good childhood”, but did not remember much. The drawing she made depicted a nightmare type situation. It showed a terrified child with a reference to sexual assault. By using art, this woman was able to unpack memories she had hidden.
Using art to communicate and heal is a cost effective way of communicating feelings. It is also available to everyone as anyone can create art in their own way. I hope to see this continue to be used in not only therapy, but school settings as well.
Cite:
Campbell, M., Decker, K. P., Kruk, K., & Deaver, S. P. (2016). Art Therapy and Cognitive Processing Therapy for Combat-Related PTSD: A Randomized Controlled Trial. Art therapy : journal of the American Art Therapy Association, 33(4), 169–177. https://doi.org/10.1080/07421656.2016.1226643
Van Der Kolk, B. (2014). The Body Keeps The Score. Penguin Books.
Communities are not equipped to handle mental health problems
Based on my own personal experience, combined with what I learned from the reading as well as talking to others with experience, I feel that that those at the top have never in their lives dealt with the mental health crisis firsthand and appear to have no empathy. During the pandemic, I worked as a security professional at a hospital as well as hotels converted into housing for at risk homeless people. I don't claim to be an expert in psychology or psychiatry, but I am fairly certain that a good number of the people I witnessed (and dealt with) at the Emergency Department as well as at the hotels were either addicted to drugs or suffering from some kind of mental health condition. Due to a lack of community resources, many of these people have no where else to go, and typically end up in either the emergency room or in jail. The conditions these people live with can be very incapacitating, and without proper treatment, trauma increases.
I understand that handling this issue is not an easy one, though a good place to start would be to invest in more mental health courts. A task force looking into problem solving course found that mental health courts were effective in providing integrated services, reducing recidivism, and with due process being preserved (Orr et al., 2009). And in addition, despite initial short term costs, the long term savings created by keeping people with these conditions out of the criminal justice system more than makes up for it (Slate & Johnson, 2008). My mother worked at a high level locked psychiatric facility and found that many of the individuals had been self-medicating with street drugs to deal with their symptoms, because they had no alternative. Mental health courts offer a pathway to get off street drugs and on proper medication. Still, without additional resources within the community, there is only so much that can be done by the courts. This has been shown in states like Alaska, which have a strong lack of community services (Slate & Johnson, 2008).
There are those who might argue that these people should not be forced into treatment, saying that this "violates their civil liberties", and that they should choose to be treated. What this does not take into account is that something I learned after talking to a court officer with many years of experience in my area. She says that some individuals are so ill that they don't even realize they need help, thinking nothing is wrong with them. They don't want to do what anyone says even if it is for their own good. If we they go without treatment, they face nearly impossible odds without housing or being able to get work.
The court officer I talked to brought up another issue, government corruption. The state capital had sent billions of dollars to our area to help deal with mental health problems in our communities. Problem is, the money seems to have vanished, or rather, as she put it, was lost in transit somehow. Getting the resources needed may be next to impossible is there is no accountability in the distribution of funds.
References
Slate, R. N., & Johnson, W. W. (2008). The criminalization of mental illness: Crisis & opportunity for the justice system. Carolina Academic Press.
Orr, C. H., Hall, J. W., Reimer, N. L., Mallett, E. A., O’Dowd, K., & Frazer, A. C. (2009). America’s problem-solving courts: The criminal costs of treatment and the case for Reform. NACDL. https://www.nacdl.org/drugcourts
The Retraumatization of Sexual Assault Victims
Sexual assault has an immense impact on victims physically, psychologically, physiologically, and emotionally (Rousseau, 2024). These effects are long-lasting and oftentimes leave invisible scars on the victim that influence their ability to function throughout every day life. This trauma is not just the result of the actual act of violence; it also occurs when the victim reports the crime to legal authorities, discloses what happened to close family and friends, pursues future sexual interactions, and is close to those who remind them of their attacker.
When victims do gain the courage to report what has happened, they often encounter victim-blaming, disbelief, and general disempowerment (Feenan, 2021). Each time a victim is asked, "What were you wearing? Did you look at him a certain way? Did you drink too much? Are you known for being a risk-taker sexually? Did you yell and scream for him to stop?" they experience further heartbreak and disappointment. These questions represent an immense failure in our society which has caused people to shame rather than support victims.
Legal authorities are oftentimes the first point of contact in a victim's reporting process. Despite a more recent push for law enforcement personnel to become trauma-informed, they often fail to manage issues pertaining to sexual assault cases with grace. During police interviews, many victims express feeling as though they mirror the unequal power balance that they felt throughout their experience with their attacker (Feenan, 2021). Oftentimes, the law enforcement officers will dismiss the victim, inappropriately press them for not immediately calling 911, or belittle them for having an initial point of contact with the perpetrator in the first place (Feenan, 2021). Sadly, the mishandling of these interviews often hinders the future desires of victims to report additional sexual assaults in the future.
Additionally, the entire trial process can provoke further retraumatization. Defense attorneys will often work to intensely discredit victims in an incredibly insensitive manner (Feenan, 2021). Obviously, it is important for all people to receive a fair trial and questioning is required to allow this to happen, but victims must be treated with empathy and respect. Problematic court proceedings may be more common in situations pertaining to intimate partner violence (Feenan, 2021). This may be because some legal personnel may genuinely be unable to comprehend that a trusted spouse or partner could possibly rape their significant other.
As present and future members of the criminal justice field, we must work to do better. As human beings, we must be better. By empowering victims to speak up, they gain access to resources and support systems which can enable them to recover from immense pain and suffering. While we may not all be equipped to bear the weight of a victims journey, we can lend an ear to listen and point out useful resources. Likewise, we can push for more trauma-informed approach to handling reporting.
Resources:
Feenan, L. (2021). Factors influencing retraumatization amongst sexual assault victims: a qualitative study of the criminal justice system.
Rousseau, D. (2024, February). Module 5. METCJ725. Online.
True Crime & Retraumatization of Victims
Society has a fascination with true crime. Serial killers are typically the crime of choice. They are the embodiment of the worst depths of what humans can be capable of. Serial killers intrigue us because we can never truly figure them out. There has been a boom in podcasts, documentaries, and books delving into the cases of the worst crimes in history. This media borders on glorifying these criminals and can lead to the retraumatization of the victims and their families.
One aspect of this phenomenon is the rise of murderabilia, which is the sale of artifacts related to criminals or crimes. One famous example of this is the art of John Wayne Gacy. Gacy created art that he sold while he was in prison. The state of Illinois actually sued Gacy over this (Homepage, 2024). Up until the ‘90s, Gacy’s art hardly sold for above $250 a piece, yet recent auctions of his art have gone for up to $175,000 (Brinkhof, 2023). With the rise of popularity of true crime media, the hobby of collecting murderabilia has also gone up. Some may see this as a morbid, but harmless hobby, but the reality is that the glorification of these items can be incredibly damaging to victims.
When a victim’s family sees the art of the person who killed their loved one be fawned over by the masses, it retraumatizes them. Imagine losing a loved one, then hearing about the gruesome details of their murder from a true crime podcast. It can feel like their pain and suffering are being exploited for profit, turning their personal tragedies into objects of fascination for others.
It's important for consumers of true crime media and collectors of murderabilia to be mindful of the impact their actions may have on victims and their families. While it's natural to be curious about these dark and twisted stories, it's crucial to remember the real people whose lives were affected by these crimes.
Brinkhof, T. (2023, May 16). Murderabilia: Our morbid fascination with the garish art of American serial killers. Big Think. https://bigthink.com/high-culture/murderabilia-serial-killer-art/
Homepage. (2024, February 2). A+E Networks EMEA. https://www.aetv.com/real-crime/john-wayne-gacy-death
Mental Health Facilities Needed
We need more mental health facilities in the U.S. to prioritize the care and treatment of our growing number of serious mental health issues. The topic of mental health should be socialized clearly and more broadly to remove the still-existing negative stigma. Social media ‘influencer’ culture of the past two decades turned our society into a disposable, transient one where depth of meaning got lost and taking care of humanity became tedious and dull. Today’s society seems more keenly aware of our interconnectedness and that to take care of only our strongest members is a disservice to everyone… I hope we are seeing a return to humanity now.
We are also living in a highly mutable, borderless, boundaryless world. One where a global viral outbreak shut down economies and affected people’s health for generations to come, potentially. The impact of medications we take, vaccines or shots we receive, food and water we consume; everything we ingest can be felt and seen for years to come. The side effects of these elements can also produce general and mental health conditions like heart conditions, depression, anxiety, PTSD, and more. If this can happen to anyone, where would we go for support and help that would be a permanent or semi-permanent solution?
More state run and supported mental health facilities are needed in the U.S., especially now and especially in my home state of California where we have been seeing an increasing number of mental health issues. Policymakers need to prioritize taking care of mentally ill patients. Money is needed for research, development, treatment, outreach, and education. We put money toward other resources like technology, which is critical for society's advancement, but we are leaving our most vulnerable members unattended and untreated. Some of the downstream impacts of this ongoing neglect can range from increased homeless populations to more mass shootings.
A local mental health hospital that used to operate in my local town from the 1970’s until early 2000’s (Agnews) is still referred to on some websites as an ‘insane asylum’ or "The Great Asylum for the Insane". (Moffitt, 2021).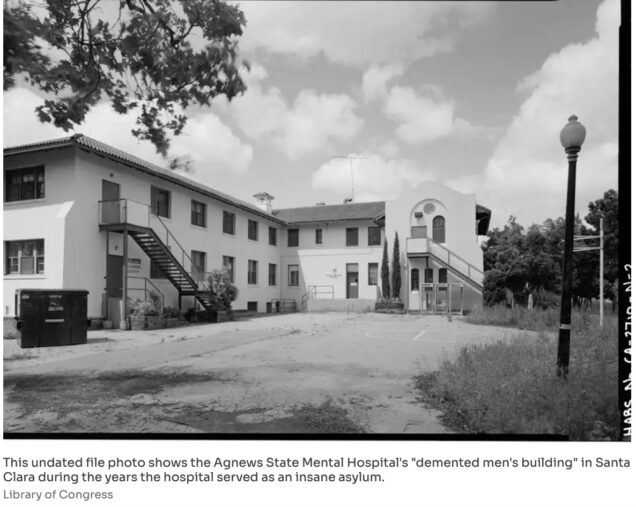 We have reached a higher-level intellectual understanding of mental illness now.
We have reached a higher-level intellectual understanding of mental illness now.
"The treatment of the insane in California dates from the earliest days of the Gold Rush. The first provisions for the insane were to lock them up with criminals in the ship Ephemia, purchased in 1849 by the City of San Francisco, and later to house them at the San Francisco marine hospital in 1850, used primarily for ailing seamen." (NPS, 2018).
This was the language of my generation and priors: “newspapers of the early 20th century routinely described [patients] as "mad," "demented" or the tabloid-friendly "lunatics."” (Moffitt, 2021). These connotations are negative and counterproductive. The slurs do not accurately describe or reflect the myriad of conditions that are identified and considered today. We have come a long way in many other advancements, it is time to progress and provide adequate support for mental health to improve our society, economy, and stability as a people.
References
National Park Service. (2018, Jan 26). Agnews Insane Asylum. https://www.nps.gov/places/agnews-insane-asylum.htm
Moffitt, M. (2021, Oct 26). A last peek inside Bay Area's abandoned 'Great Asylum for the Insane' before it disappears forever. SF Gate. https://www.sfgate.com/local/article/Abandoned-San-Jose-insane-asylum-Agnews-ruins-13527415.php
Recognizing Addiction as a Disease in the Criminal Justice System
Our society's view on crime tends to focus on incarceration rather than rehabilitation. Why is that the case? Additionally, the focus is largely on retribution rather than finding the root causes of a particular crime. We prioritize policies and structures that are tough on crime, but there is a lack of policies that address the drug subculture that exists within the criminal justice system. At the forefront of the criminal justice system is the goal of protecting the public's general welfare. Nevertheless, aren't nonviolent drug offenders part of that population? If so, have we failed them in a sense?
The opioid epidemic has affected the entire country. The Centers for Disease Control and Prevention stated that the number of people who died from a drug overdose in 2021 was over six times the number in 1999. The number of drug overdose deaths increased by more than 16% from 2020 to 2021 (2023). These staggering numbers show that drug usage in our country is only getting worse as the years progress. As it relates to incarceration rates, those who suffered from addiction and committed crimes relating to drugs or alcohol made up 85% of the nation's prison population (Rousseau, 2024). That means the majority of our incarcerated population has committed their crimes due to their disease of addiction. When you think of this population behind bars who are suffering from addiction, keep in mind that being behind bars does not aid the individual in recovery, either, as many inmates still find ways to smuggle substances into prisons (Rousseau, 2024). Even while incarcerated, without being given the proper treatment, those suffering will go to extreme lengths to fuel their addiction because the pain of withdrawals is too intense.
To put it quite bluntly, those who have committed offenses related to drugs get very little help, if any, while incarcerated. Unfortunately, for over 30 years now, conservative policies have dominated how CJ professionals approach people with an addiction within the criminal justice system. These conservative policies have most notably included the use of mandatory minimum laws. Still, critics argue that these laws do nothing but target minority populations and have only contributed to the issue of overcrowding in U.S. prisons (Rousseau, 2024). There are also exceptionally high rates of recidivism for drug-related offenses. The National Library for Medicine states that illegal drug use increases the likelihood of continued involvement in criminal activity, with high rates of relapse and recidivism found among drug-involved offenders; 68% of drug offenders are rearrested within three years of release from prison (Belenko et al., 2013). Most of those who fall into this pattern come from marginalized communities and have no way of receiving any treatment for their struggles.
Yet, there is still scrutiny surrounding non-violent drug offenses. Instead of formulating new policies that would help to ensure that these individuals receive adequate treatment to not only be functioning healthy members of society but while doing so, this would work towards improving the recidivism rates in this country and help to alleviate the opioid epidemic. It should be a goal to move towards a system that recognizes addiction as a disease rather than a choice. In doing so, we can aim towards providing these individuals with the necessary tools and resources to fight their disease.
I will never condone crime or violence in any way. This post is, in essence, not to perpetuate a debate regarding dismantling the criminal justice system and its structure but rather to improve it while giving these individuals who suffer from the disease of addiction a second chance at life. Creating a unified approach within our system so those from the lowest and highest levels are educated on addiction and can come from a viewpoint that is more sustainable to view it as a disease.
References
Belenko, S., Hiller, M., & Hamilton, L. (2013). Treating substance use disorders in the criminal justice system. National Library for Medicine.
Centers for Disease Control and Prevention. (2023, August 8). Understanding the opioid overdose epidemic. Centers for Disease Control and Prevention.
Chapter 55 Data Visualization. The Massachusetts Opioid Epidemic. (2016). https://chapter55.digital.mass.gov/
Rousseau, D. (2024). Module 2 Lecture Notes: Thinking Like a Forensic Psychologist. Boston University.
How Mental Health Hinders Cops and How We Can Best Aid It
Police officers choose to take part in an extremely traumatic career path because of a calling. What we are just not beginning to understand is exactly how traumatic the path is. There have been a number of studies in fairly recent years about the damage that trauma can do to police officers that are constantly thrown into stressful and harmful environments.
The first big study was done in 1999 by Stevens and Long. They found that 12-35% of their participants exhibited PTSD behaviors or do have been diagnosed with PTSD (Craddock & Telesco, 2021). They also found that over 20% of participants suffer from sleep issues including nightmares (Craddock & Telesco, 2021). We are aware of the lasting damages done by getting a lack of adequate sleep, especially when it comes to split-second decisions that are required when in law enforcement.
As the years progressed, police officers were shown to have increased levels of substance abuse and suicide than that of the general population. One of the most traumatic experiences for police officers were for those involved in the September 2001 attacks. There have been numerous follow-up studies done on them and found that they had higher than average PTSD symptoms than other cops across the country (Craddock & Telesco, 2021). They also, if they were physically able to, went back to work which would compound their already experienced stressors into more as more situations arose.
In the research conducted by Tina B. Craddock and Grace Telesco in 2021, they had many research questions and hypotheses they were searching for answers of, but their findings were interesting.
They found that the longer someone is in law enforcement, the worse that their mental health and physical health is (Craddock & Telesco, 2021). These are exacerbated by the decreased perceptions of law enforcement is today's society. Their symptoms of their decreased mental illnesses could present as more violent towards civilians or prisoners they interact with, rash decisions, and increased aggravation and possible violence towards family. These are many things that make a cop unfit for duty. They did not find a correlation between increased years on the job and increased alcohol abuse.
When it comes to aiding the police officers who are suffering from increased mental health disorders, we need to put as many tactics in action as possible. The main tactic is to have places where officers feel safe talking about their experiences (Buckhannon, 2023). This, even though a great idea, is easier said than done. A lot of police officers do not want to be involved with therapy of any kind due to its perception of being broken or weak. Instead of having a therapist at the station or that works with police officers, I think there needs to be a public hangout where police officers can meet up with each other and talk like friends. Some of the best therapy is hanging out with people that understand what you've been through and who you can blow off steam with. On a policy level, there needs to be mandated mental health care provided for police officers if they choose to take them up on the service. With this, there needs to be an additonal budget allotment so that the police officers do not see it as taking away other resources that they could be having. These are just limited examples of all of the things that need to be done to ensure that our police force works at their highest capacity. Until law enforcement, policy makers, and the government all work together to attack this threat to our law enforcement officers, this pandemic will continue to evolve and will continue to harm people in law enforcement, their families, and the communities as a whole.
References:
Buckhannon, C. M. (2023, April 4). How to help officers’ traumatic stress. Police1. https://www.police1.com/wellness-week/articles/how-to-help-officers-traumatic-stress-8tk6JlkiiOForRYE/
Craddock, T. B., & Telesco, G. (2021, November 9). Police stress and deleterious outcomes: Efforts towards Improving Police Mental Health. Journal of police and criminal psychology. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8575544/