Home
Tetris for Trauma – Unconventional Approaches to Trauma Prevention
When looking for a blog post subject, I decided that I wanted to learn more about the latest updates in trauma care. As we have seen in class and in our readings, trauma care has changed significantly over the last few decades. For example, in van der Kolk’s book The Body Keeps the Score: Brain, Mind and Body, he discusses an old belief that in the case of father-daughter incents, “incestuous activity diminishes the subject's chance of psychosis and allows for a better adjustment to the external world”. This is clearly not an opinion that we would take today and demonstrates the progress made in psychological research.
So what are some of the newer ideas about trauma? One of the ones that caught my attention was playing “Tetris” as a potential trauma prevention. This idea was presented in the article “Can playing Tetris help prevent PTSD if you’ve witnessed something traumatic?”(Bressington & Mitchell, 2024). It seems to have first been proposed in 2009 by Oxford University psychologists. They suggest that playing a visuospatial game like “Tetris”, within 30 minutes after a traumatic event may disrupt the formation of sight and sound memories related to the traumatic event. This is because trauma flashbacks are sensory-perceptual, visuospatial mental images. Therefore, when a visuospatial game like “Tetris” is played within the time usually reserved for memory consolidation, it fights for the brain’s resources and leads to reduced flashbacks (Holmes et al., 2009).
While this research was done over a decade ago, more recent research has also shown success in using “Tetris” to prevent PTSD flashbacks as well as potentially reducing depression and anxiety in combat veterans (Butler et al., 2020). Additionally, in a randomized controlled trial, “Tetris” was found to be an effective intervention to reduce intrusive memories overall and lead to declined intrusive memories for emergency department patients who had experienced motor vehicle crashes. Patients found this intervention easy, helpful, and minimally distressing (Iyadurai et al., 2018). Another study suggested the use of “Tetris” and other verbal word games to reduce intrusive memories (Hagenaars et al., 2017).
Although this research has not been implemented into most people’s mental health practices in the medical community, it is frequently offered as advice to people seeking help after a traumatic situation on Reddit. An example presented in the Bressington and Mitchell article is from a Reddit poster in Sydney, Australia looking for advice on dealing with a traumatic situation (saltyisthesauce, 2024). Additionally, if you just type in “Tetris for PTSD” in the Reddit search, numerous posts advocating for “Tetris” playing can be found, especially for visually disturbing traumatic situations. While obviously, this is not research and not normally something I would cite, for this blog post in exploring the topic, I thought it would be worth noting as it demonstrates that the idea has spread outside of the research world and has some acceptance in the general public.
For my own opinion on the subject, I really like the idea of “Tetris” as a potential trauma prevention. One of its main draws is its accessibility. “Tetris” is freely available to anyone who owns a phone or computer. This makes it much more accessible than most trauma treatments such as medications or therapy. This also means it is more accessible financially and for groups who may not traditionally utilize healthcare. Additionally, it presents a way to prevent PTSD in the first place, as its mechanism of action is to interrupt memory formation instead of responding to the trauma after the fact. This could have important implications for the future of trauma research as preventing trauma from occurring is better than having to deal with the side effects after the fact. Therefore, after a traumatic event, the idea of playing “Tetris” presents an easily actionable, potentially beneficial, step instead of ruminating about the traumatic event. I’m excited to see future research on this topic and hope to see more unconventional PTSD treatments like it in the future.

Citations
Bressington, D., & Mitchell, D. A. (2024, April 15). Can playing Tetris help prevent PTSD if you’ve witnessed something traumatic? The Conversation. http://theconversation.com/can-playing-tetris-help-prevent-ptsd-if-youve-witnessed-something-traumatic-226736
Butler, O., Herr, K., Willmund, G., Gallinat, J., Kühn, S., & Zimmermann, P. (2020). Trauma, treatment and Tetris: Video gaming increases hippocampal volume in male patients with combat-related posttraumatic stress disorder. Journal of Psychiatry and Neuroscience, 45(4), 279–287. https://doi.org/10.1503/jpn.190027
Hagenaars, M. A., Holmes, E. A., Klaassen, F., & Elzinga, B. (2017). Tetris and Word games lead to fewer intrusive memories when applied several days after analogue trauma. European Journal of Psychotraumatology, 8(sup1), 1386959. https://doi.org/10.1080/20008198.2017.1386959
Holmes, E. A., James, E. L., Coode-Bate, T., & Deeprose, C. (2009). Can Playing the Computer Game “Tetris” Reduce the Build-Up of Flashbacks for Trauma? A Proposal from Cognitive Science. PLoS ONE, 4(1), e4153. https://doi.org/10.1371/journal.pone.0004153
Iyadurai, L., Blackwell, S. E., Meiser-Stedman, R., Watson, P. C., Bonsall, M. B., Geddes, J. R., Nobre, A. C., & Holmes, E. A. (2018). Preventing intrusive memories after trauma via a brief intervention involving Tetris computer game play in the emergency department: A proof-of-concept randomized controlled trial. Molecular Psychiatry, 23(3), 674–682. https://doi.org/10.1038/mp.2017.23
saltyisthesauce. (2024, April 13). What just happened at Bondi junction? [Reddit Post]. R/Sydney. www.reddit.com/r/sydney/comments/1c2uo3p/what_just_happened_at_bondi_junction/kzd8t6u/
Culinary Therapy (a.k.a. Cooking Therapy)
While the notion of food as therapy may conjure imaginings of your favorite pint of ice cream and a spoon, culinary therapy is, in fact, a therapeutic technique that can help patients with relationship, psychological and behavioral disorders. Dr. Michael Kocet, chair of the Counselor Education Department for the Chicago School, defines culinary therapy as “the therapeutic technique that uses arts, cooking, gastronomy, and an individual’s personal, cultural, and familial relationship with food to address emotional and psychological problems faced by individuals, families, and groups. Culinary therapy involves an exploration of an individual’s relationship with food and how food impacts relationships, as well as psychological well-being and functioning.” (Vaughn, 2017)
Cooking as a modality for therapy can also be used in a less clinical format. In a separate article on cooking therapy, Debra Borden, licensed clinical social worker, uses cooking practices with clients to connect them with the specific “opportunities and assets” that cooking offers, namely: “metaphor, mindfulness, and mastery. The metaphors are sometimes obvious—there’s nothing subtle about kneading frustrations into bread dough—but Debra specializes in encouraging patients to see each act and ingredient as symbolic of something deeper, a kind of concentration that encourages that second M, mindfulness. And if you can pay attention to the metaphors and learn something new about yourself you get that sense of mastery: a little thrill of accomplishment that reinforces your belief in your own competence and skill.” (Romanoff, 2021)
While practitioners of culinary therapy have varying approaches, the tasks and activities associated with meals: planning, preparing, serving, eating and clean-up each serve as opportunities to re-instate routine, order, even social reintegration and trust for the individual, a family, or other group.
Behavioral scientists continue to explore and validate cooking interventions for positive psychosocial outcomes. A 2018 Health Education & Behavior Journal article, Psychosocial Benefits of Cooking Interventions: A Systematic Review, documented and research-validated positive outcomes that include:
- Confidence and Self-Esteem: “participation in baking sessions led to improved self-esteem, primarily as a result of increased concentration, coordination, and confidence.”
- Socialization: “There was some evidence that socialization benefits might extend beyond the cooking interventions, as some participants continued to report improved social interactions at home and with family, and they continued to prepare meals as household teams even 6 months later.”
The researchers concluded, “Despite varying types of measurement tools and different patient populations, these studies reported a positive influence associated with participation in cooking interventions on psychological outcomes, including self-esteem, social interaction, as well as decreased anxiety, psychological well-being, and quality of life.” (Farmer, Touchton-Leonard, & Ross, 2018)
A specific study of meal preparation and cooking group participation concluded “that meal prep and cooking groups may be significant for helping psychiatric clients achieve and maintain appropriate mood and hygiene for independent living skills.” (Garcia & Privott, 2023)
Whether the therapy is individual or group-oriented, meal preparation and food-oriented tasks can be an effective therapeutic modality to improve psychological, behavioral, and relationship / social disorders.
References
Farmer, N., Touchton-Leonard, K., & Ross, A. (2018). Psychosocial Benefits of Cooking Interventions: A Systematic Review. Health Education & Behavior, 167-180.
Garcia, A., & Privott, C. (2023). Meal Preparations and Cooking Group Participation in Mental Health: A Community Transition. Food Studies: An Interdisciplinary Journal, 85-101.
Romanoff, Z. (2021, June). I Hired a Cooking Therapist to Deal With My Anxiety. bon appetit, pp. https://www.bonappetit.com/story/cooking-therapy.
Vaughn, S. (2017, October). From cooking to counseling. Retrieved from The Chicago School: From the Magazine | Insight: https://www.thechicagoschool.edu/insight/from-the-magazine/michael-kocet-culinary-therapy/
Trauma in the Texas Juvenile Justice System and two Great Therapeutic Programs
Trauma in the Texas Juvenile Justice System
It is widely recognized that children incarcerated in the Texas Juvenile Justice System have often experienced significant trauma before their admission to state schools, halfway houses, and probation systems. The Texas Juvenile Justice Department (TJJD) aims to "create an environment where we can help them learn to make decisions, manage their emotions and reactions to stress, and take responsibility for their lives and decisions—in other words, to correct" (Texas Juvenile Justice Department, n.d.). This approach is embodied in the Texas Model.
Many children in the system have faced adverse childhood experiences (ACEs), which may include having one or both parents incarcerated, being victims of sexual assault, experiencing aggravated assault, death, and various forms of family violence. Most, if not all, of the children incarcerated have at least four ACEs. ACEs are defined as Adverse Childhood Experiences. According to Module 2 of Professor Rousseau’s course, the following ACEs categories are included:
- Alcoholism and alcohol abuse
- Chronic obstructive pulmonary disease
- Depression
- Drug use
- Heart disease
- Liver disease
- Risk of partner violence
- Smoking
- Suicide
- Overall decline in quality of life (Rousseau, n.d.)
Statistics from the Texas Juvenile Justice Department and the Centers for Disease Control and Prevention (CDC) indicate that individuals with just one ACE have a 200% to 500% increased chance of attempting suicide. With four ACEs, the risk increases to 2400%, and with seven ACEs, it rises to a staggering 5100% compared to those with no ACEs. In the Texas Juvenile Justice System, "fifty-two percent of our youth in secure facilities have four or more ACEs,” according to a conservative estimate. Breakdown statistics show that about 50% of boys and 87% of girls in the system have four or more ACEs, with 47% of girls having seven or more (Texas Juvenile Justice Department, n.d.).
Given these statistics, it is crucial for the Texas Juvenile Justice Department to focus its correctional and educational efforts on behavioral and mental healing. While it is important to hold these children accountable for their actions, this should be done within a trauma-informed, healing environment. Texas should prioritize rehabilitation through trauma-informed care over punitive measures.
Trauma-informed care in the Texas Juvenile Justice System is essential. Rousseau (n.d.) emphasizes that “Trauma-informed care needs to build on practices, skills, training, and strategies that directly affect the entire juvenile justice continuum of care.” Texas screens incoming child offenders for ACEs to ensure appropriate placement in TJJD facilities.
Here are some examples of trauma therapy programs currently used in TJJD to address behaviors and educate families on coping with past traumatic experiences:
- Aftercare Management
- Anger Management/Conflict Resolution
- Animal/Equine Therapy
- At-Risk Programs
- Border Children Justice Project
- Cognitive Behavioral Therapy/Treatment
- Community Service/Restitution
- Counseling Services
- Drug Court
- Early Intervention/First Referral
- Educational Programs
- Electronic/GPS Monitoring
- Experiential Education
- Extended Day Program/Day Boot Camp
- Family Preservation
- Female Offender Programs
- Gang Prevention/Intervention
- Home Detention
- Intensive Case Management
- Intensive Supervision
- Life Skills Programs
- Mental Health Services
- Mental Health Court
- Intellectual Disabilities Services
- Mentoring
- Parent Training (for parents)
- Parenting (for juveniles)
- Runaway/Truancy Programs
- Sex Offender Treatment
- Substance Abuse Prevention/Intervention
- Substance Abuse Treatment
- Victim Mediation
- Victim Services
- Vocational/Employment Programs (Texas Juvenile Justice Department, 2024).
This blog will focus on two programs that require additional funding and have shown success with youthful offenders. I will reference a 2024 TJJD findings report from an investigation conducted by the U.S. Department of Justice Civil Rights Division and the U.S. Attorney’s Offices for the District of Texas. Despite numerous issues within TJJD facilities, efforts are being made to address these problems. The Office of the Inspector General has been established to address criminal acts occurring in TJJD facilities. Access points into and out of the facilities have been taken over to control contraband and improve safety. However, staff violations of rules and policies remain a concern.
The TJJD has reintroduced the BARK therapy program, which involves TJJD becoming a foster home for dogs. According to Woodard (2024), the Gainesville State School Superintendent acknowledges that most juvenile offenders come from traumatic environments. He emphasizes that the TJJD system refers to offenders as "adjudicated" rather than "convicts," recognizing their victimization. The program currently includes sixteen children and six dogs. It teaches offenders to care about something other than themselves and promotes discipline. A quote from a participant reflects the program's impact: “When I first got him, he was kind of shaken up because of where he came from. And I felt that same way – we had that same connection” (Woodard, 2024). Another participant noted, “They say a dog is a man’s best friend and I agree... If I feel down, he will come around and help me out” (Woodard, 2024). The BARK program is noted for having the fewest incidents on campus, indicating its effectiveness in trauma-informed rehabilitation.
Another notable trauma-informed program is the equestrian program formerly located at Tornado Ranch. Known as Trauma-Focused Equine Assisted Psychotherapy or Trauma-Informed Equine Assisted Learning, this program was discontinued due to financial constraints, resources, and departmental priorities. Like the BARK program, it allowed youths to establish empathy, discipline, and love by caring for rescue horses. The program helped participants resolve personal traumas and improved their understanding of themselves and others. The reintroduction of this program would benefit the TJJD system (TJJD, 2018).
To ensure that these children become productive members of society, it is essential to secure funding for these programs. A just society requires a trauma-informed correctional system that supports all its members.
References
Rousseau, P. (n.d.). Module 2: Adverse Childhood Experiences. [Course material].
Texas Juvenile Justice Department. (n.d.). Program Registry - Public Access. Retrieved from https://www2.tjjd.texas.gov/programregistryexternal/members/searchprograms.aspx
Texas Juvenile Justice Department. (2024). [Report].
Centers for Disease Control and Prevention. (n.d.). Adverse Childhood Experiences. Retrieved from https://www.cdc.gov/violenceprevention/aces/index.html
U.S. Department of Justice. (2024, August 2). Homepage. Retrieved from https://www.justice.gov/
Woodard, T. (2024, May 20). This high-security juvenile detention center in North Texas just became a foster home for dogs. WFAA. https://www.wfaa.com/article/features/originals/high-security-juvenile-detention-center-texas-became-foster-home-for-dogs/287-7eaf7654-3128-4eaf-8a92-f22892a49dde
Texas Juvenile Justice Department. (2018, September 22). Tornado Ranch has ramped up in the past six months. Facebook. https://www.facebook.com/TexasJJD/posts/tornado-ranch-has-ramped-up-in-the-past-six-months-and-now-serves-10-youth-who-p/2147383878916782/?locale=hi_IN
How Safe Is Our World Today, Really?
I have noticed increased vigilance amongst the population, increased reporting of crimes and headlines in newspapers, increased interest in true crime, crime documentaries/films, and a general public intoxication of crime. Why people have become so enamored with genres such as true crime, I don't think is necessarily a modern phenomenon -- I mean, take a look at the sheer popularity of Agatha Christie's books, with her first book being published in 1920 (Britannica, 2024).
If we take a look at data from the FBI's Crime Data Explorer (https://cde.ucr.cjis.gov/LATEST/webapp/#/pages/explorer/crime/crime-trend), we can see some really interesting things. For example, if we look at the rate of violent crime offenses by population (in the U.S.), we are met with data that suggests that 2022 is one of the "safest" years.
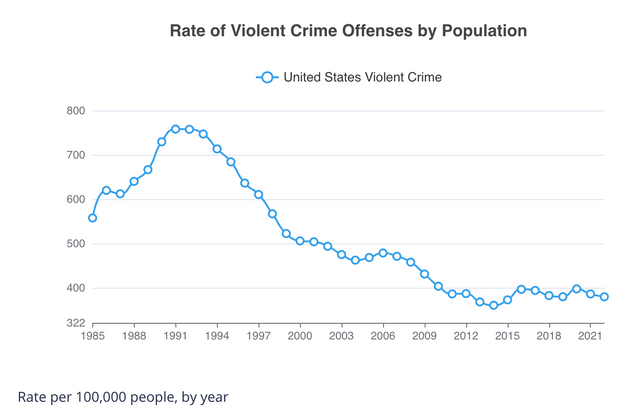
Despite these reassuring statistics, according to the Lloyd's Register Foundation World Risk Poll (2021), 39% of Americans surveyed feel less safe than they did five years ago. As well as that, 26% of Americans felt very worried about violent crime causing them serious harm, which was an increase from 22% in 2019. So, despite there being evidence from the FBI that 2021 and 2022 are significantly safer than other years, in regards to violent crime, individuals feel less safe compared to 5 years ago (2016), which was more unsafe than 2021. In 2016, the FBI reported there to have been a rate of 397.5 violent crime offenses per 100,000 compared to 387 in 2021.
So, even though the world is safer than it previously was, people still are more concerned about their safety. This feeling of unsafety could be a result of the COVID-19 pandemic, which, for many individuals, led to long-term health consequences or mental health consequences. However, this perception gap (Ropeik, 2011) between the likelihood of violent crime and the perceived fear of violent crime existed long before the pandemic. Many individuals chalk this perception gap up to the media, the increased reporting of violent crimes, and the idea of "if it bleeds, it leads" - a term coined by William Randolph Hearst at the end of the 1890s.
Surveys such as the Figgie Report on Fear of Crime (Research and Forecasts Inc, 1980) suggest that the fear of crime was also pervasive in the late 70s/80s, with 4 out of 10 Americans being highly fearful of becoming victims of violent crime. However, as we can see from the FBI UCR data above, the 80s into the mid-90s was a time where the rate of violent crime offenses were significantly higher, meaning perhaps Americans' fear at the time was more based in true likelihood rather than perceived likelihood.
If we consider comparing violent crime to another type of crime, such as property crimes, we are met with starkly higher rates of offenses than that of violent crimes. All property crimes include arson, burglary, larceny-theft, and motor vehicle theft, and all violent crimes include homicide, rape, robbery, and aggravated assault. In 2022, the rate of property crime offenses was 1,954.4 per 100,000 people, compared to 380.7 per 100,000 people for violent crimes. Despite more offenses of property crime occurring per year in the United States, it is given less media attention. In Michael O'Hear's statistical overview of media coverage in Milwaukee, Wisconsin (2020), he compared the offenses noted on the front page of the Journal Sentinel and WTMJ.com to offenses reported to police in Wisconsin.
[Will try to re-insert media; had issues trying to attach the pie charts]
Theft and burglary accounted for 62% of the crimes reported in Milwaukee County and 68% statewide. This starkly contrasts the reporting of these two crimes, accounting only for 3% of the Journal Sentinel stories and 22% of the stories reported on WTMJ.com. O'Hear also made an interesting realization that the media placed a stronger emphasis on crime with female victims and young victims, which, according to the data relating to homicide victims in Milwaukee, was disproportionate to the actual patterns.
Works Cited
Britannica, T. Editors of Encyclopaedia (2024, February 16). Agatha Christie. Encyclopedia Britannica. https://www.britannica.com/biography/Agatha-Christie
FBI Crime Data Explorer, UCR https://cde.ucr.cjis.gov/LATEST/webapp/#/pages/explorer/crime/crime-trend
Lloyd's Register Foundation. (2021). World Risk Poll, Gallup Data. Retrieved from https://wrp.lrfoundation.org.uk/a-world-of-risk-country-overviews-2021/
Ropeik, D. (2011, February 3). The perception gap: An explanation for why people maintain irrational fears. Scientific American Blog Network. https://blogs.scientificamerican.com/guest-blog/the-perception-gap-an-explanation-for-why-people-maintain-irrational-fears/
Research and Forecasts Inc. (1980) Figgie Report on Fear of Crime - America Afraid, Part One - The General Public. https://www.ojp.gov/ncjrs/virtual-library/abstracts/figgie-report-fear-crime-america-afraid-part-one-general-public
Michael O'Hear, Violent Crime And Media Coverage In One City: A Statistical Snapshot, 103 Marq. L. Rev. 1007 (2020).
Available at: https://scholarship.law.marquette.edu/mulr/vol103/iss3/14
Mental Illness In Women Offenders
The national female incarceration rate is rising at a dramatic rate as compared to male offenders (Rousseau, 2024). However, there is seemingly less of a focus on treating the unique issues that come with female offenders. Correctional institutions have been used to treat female offenders with severe mental illness, who are not receiving the appropriate treatment for their diagnoses, calling for an immediate reform in our system to incorporate gender responsive mental health programming in our corrections departments.
Prisons have been commonly used as an alternative to a mental health facility for female offenders, however, these two types of institutions are incomparable in treatment needs. Placing mentally ill women in prison means that they must acclimate themselves to the regimentation and unquestioning obedience that keep prisons running smoothly, however, the behaviors required are simply beyond the abilities of most seriously mentally ill women (Lord, 2008). In a study by Janet Warren, clinical associate professor of psychiatric medicine at University of Virginia, her findings included that women inmates in her sample as more like women who were receiving inpatient or outpatient mental health treatment than to women in the community (Lord, 2008). The rate of PTSD among women in prison is believed to be twice the size of that among women in general population. Furthermore, the most common pathways into crime for women are based on survival of abuse and poverty and substance abuse (Rousseau, 2024). Warren found that there were two major clusters of diagnoses that the sample of female inmate’s personality disorders fell into, including tumultuous relationships, impulsivity, recklessness, susceptibility to substance abuse, and abuse in one cluster and suspiciousness, social awkwardness, and overly dependent attitudes and behaviors in another (Lord, 2008). These diagnoses are believed to be present prior to incarceration, and contribute to the behaviors that lead to incarceration, causing an immediate need for mental health treatment.
A prominent issue for incarcerated female offenders with mental illness is self-harm activities. Some mentally ill women self-harm exclusively, and some go between self-harm and violence, and if one woman self-harmed, others often followed because the nature of relationships between women cued much of their behavior, both positive and negative (Lord, 2008). Women offenders will use anything in reach to self-harm, such as screws, plastic, paperclips, staples, and anything else they may have access to. Most women offenders who self-harm during incarceration begin their self-harm behavior long before they get to prison. Most began to cut or swallow when they were young teenagers, often in juvenile facilities, on observing another girl cut or self-harm (Lord, 2008). Although some prisons punish self-harm, most prisons punish the behaviors associated with self-harm, however, cell confinement seems to result in yet more self-harm (Lord, 2008).
Many prisons create programs for mental health; however, they fail to create a therapeutic environment in doing so because ultimately, prisons operate on the basis of power and control. Prisons are not the best places for the mentally ill to develop a sense of autonomy or to experiment with new interpersonal skills (Lord, 2008). Prison is difficult for any offender, however mentally ill women offenders struggle greatly due to the lack of connection and relationships, such as with their family members. This issue is especially prominent with the lack of physical contact with their children specifically, and being unable to contact those they formed relationships with during incarceration upon release, leaving mentally ill female offenders isolated and lonely both inside and outside correctional institutions (Lord, 2008).
We must do what we can to address these disparities in mental health treatment for mentally ill female offenders, as prison is not always the answer to rehabilitation in these cases. Other interventions must be implemented to fully address and treat mental illness specific to the diagnoses commonly seen in justice involved women. “It is not that we do not know how to create meaningful changes to our prison and mental health systems, it is that we do not have the will to do so. It is far easier to put people who are dangerously ill behind walls and fences; in that way, we will never have to acknowledge their suffering” (Lord, 2008).
References:
Lord, E. A. (2008). The challenges of mentally ill female offenders in prison. Criminal Justice and Behavior, 35(8), 928-942.
Rousseau, D. (2024b). Treating women offenders [Lecture]. Boston University, Forensic Psychology. Blackboard: https://onlinecampus.bu.edu/ultra/course
To Name or Not to Name?
Hello All,
I am using one of my blog posts to start a discussion on an issue that Dr. Silver briefly touched on during our last live class session during his presentation. The topic that I am going to explore revolves around feelings and rationales for/against using the names of mass murderers when discussing their crimes. Dr. Silver, for example, made a conscious effort not to mention the names of the killers he discussed unless it was necessary to identify a particular event. As a research assistant during my time as an undergrad, we primarily used the initials of the domestic terrorists central to our research. In preparing to write this blog post, I sent a text message to the professor with whom I performed research and asked him the thought behind using an offender's initials. His reply: "...I guess for me, it started after Columbine upon learning the shooters wanted to be famous" (Pete Simi). While I understand the thought behind Dr. Simi's rationale, in the context of academic research, I still feel it most appropriate to refer to offenders initially using their first and last names.
In contrast to my undergrad experience, now working with individuals on death row, I better understand the settings in which it is undoubtedly most appropriate to forego mentioning their names. In my interactions with offenders, I use their names. Typically, offenders ask that I use their first names instead of "Mr." However, on and leading up to execution dates, I often interact with the families of the victims of the offender's crimes. I have come to learn that, collectively, victims' families would prefer not to hear the names of the offenders.
I do find it somewhat puzzling that victims' families want to avoid hearing the offenders' names, but they often elect to witness their executions. Frequently, during an execution, offenders will speak-- either informally or formally by way of their final statements. I am curious to her your thoughts on this. Are you surprised that victims' families report not being able to stomach hearing the names of offenders but still elect to watch them die? I fall on what I assume is the less common side of the argument-- I see no issue with researchers, speakers, and news reports using the names of offenders, so long as the actual context of their message does not glamourize or praise the offender's actions.
Trauma and its impact on our body
Trauma and how trauma impacts the brain is something that I find interesting. In my previous semester, one of the books I had read dealt specifically with how trauma impacts our brain and our body. One thing that I think is incredibly interesting, is that they found that part of your brain essentially shuts down when you have a flashback or memory of a traumatic event. The idea that an event can be so distressing and traumatic that it shuts down part of one of the most important organs that is responsible for keeping us alive. This is something that I would want to research further in the future and learn more about. Knowing that trauma can stunt our brain function, as well as be the source of multiple different illnesses and stressors makes me wonder if, as more research comes out as our technology advances, if there will be different and more ways that come out for treating trauma.
DER, K. B. V. (2015). Body keeps the score brain, mind. PENGUIN Books.
Misinformation of crime through social media
Today, information is obtained from more than just the local newspaper. News has become available in real-time at the tap of a button, through news apps, social media, live streams, and more. While society adapts to our widespread availability of information, it is critical that we recognize the pitfalls that misinformation in media may play in the criminal justice system.
In recent years, the frequency of mass killings has increased significantly. Specifically, 78 mass shootings occurred in the United States between 1983 and 2012 (Bartol & Bartol, 2021). In contrast, the Gun Violence Archive recently reported that approximately 650 mass shootings occurred in 2023. And while many serious crimes are cause for concern, multiple murder crimes like mass shootings can have profound effects on both the victims and their community. This is when our avid use of social media may pose an issue.
On October 1, 2017, a gunman began shooting at thousands of concertgoers during a country music festival in Las Vegas, Nevada (Blankstein et al., 2017). In the end, over 50 were killed and over 500 left injured (Blankstein et al., 2017). This incident would later become the country's deadliest mass shooting (Blankstein et al., 2017). As the shooting progressed, social media became flooded with misinformed reports of multiple shooters along the Las Vegas Strip. Local police officials later confirmed that the shooting was a single event, in only one area, executed by a sole gunman (LVMPD, 2018). In the midst of social media's instant reach, misinformation can quickly spread and induce even more hysteria or fear. Dr. James Alan Fox, a Northeastern criminology professor, raises a thought-provoking point: "In the face of hyperbolic media coverage and public fear, we tend to embrace easy solutions and quick fixes that don’t necessarily work and sometimes make matters worse" (SCCJ, n.d.).
Because of the prevalence social media has, we should consider how powerful posting may be to those involved, those waiting to hear news, and those who may have experienced similar trauma. Following a mass killing, social media may buzz for weeks or months about the perpetrator, their motive, resharing newly discovered materials on these individuals, and so on. Understandably, an involved individual may experience retraumatization or face difficulty moving forward during a social media frenzy. So, as we become engulfed in learning more about the how's or why's of these crimes, we must also be extremely sensitive to the impactful nature of them.
References
Bartol, C. R. & Bartol, A. M. (2021). Criminal behavior: A psychological approach (12th ed.). Pearson.
Gun Violence Archive. (2023). GVA - 10 Year Review [Data set]. Gun Violence Archive. https://www.gunviolencearchive.org/
Las Vegas Metropolitan Police Department (LVMPD). (2018). LVMPD Criminal Investigative Report of the 1 October Mass Casualty Shooting. LVMPD.
School of Criminology & Criminal Justice (SCCJ). (n.d.) Mass Killing Database. Northeastern University. https://cssh.northeastern.edu/sccj/mass-killing-database/
Correcting Behavior, Causing Trama
Mental illness is becoming an increasingly important aspect of the criminal justice system, particularly as it pertains to the corrections facilities many mentally ill people find themselves in. Due to the deinstitutionalization movement, many mentally ill individuals “are now living in the community and lack the kind of support services and job opportunities they need to stay out of trouble” (Kupers, 1999, p. 13). This leads to them becoming involved in the corrections system. Once they enter the system, many mentally ill inmates suffer greatly due to the conditions that prisons facilitate. Inmates may find themselves feeling stigmatized for becoming incarcerated, feeling afraid for their future, and feeling ignored by corrections staff (Kupers, 1999; Hayes, 2010). These factors work to make the symptoms of mental illness worse and can lead to significant trauma among mentally ill inmates, even leading some inmates to have mental breakdowns (Kupers, 1999). Additionally, the lack of awareness among correctional staff of the different types of mental illness and their presenting symptoms can lead to issues later on. For example, some inmates with mental illness may have a hard time understanding and complying with correctional officers’ orders and might be punished for it (Kupers, 1999). These officer-inmate interactions can even become deadly (Kupers, 1999).
Because of these factors and adverse conditions, “suicide continues to be a leading cause of death in jails across the country,” according to a study conducted by the Hayes with the National Institute of Corrections (2010, p. 1). Most citizens of the United States approach incarceration with an “out of sight, out of mind” mindset, but inmates are still people and are worthy of proper care and respect. As such, it’s increasingly important that steps be taken to prevent this high number of suicides in the corrections system. The Suicide Prevention Resource Center (2011) identifies the training of correctional staff to recognize the warning signs of suicide to be a point of improvement. Other places to improve include 1) initial screenings of inmates for suicidal ideation, 2) implementation of suicide-resistant housing cells and infrastructure, 3) comprehensive observation and treatment plans, and 4) increased lines of communication between inmates, care teams, and correctional staff (Hayes, 2010).
These are all great steps to take, but I believe that we need to address the underlying conditions of prison culture and our society as a whole. Educating correctional staff on the different types of mental illness and their symptoms could work to decrease stigma and lead to better staff-inmate interactions. Additionally, it may be more helpful to implement policies that would prevent mentally ill people from ending up incarcerated solely because of the symptoms they present. As mentioned before, many of these inmates were people who would have been in a mental facility prior to the deinstitutionalization movement. More focus on increasing access to mental health support and services would be beneficial and may lessen the burden on the corrections and legal systems. If this is truly a mental health issue, we need to be treating it as such.
References
Hayes, L. (2010). National Study of Jail Suicide, 20 Years Later. National Institute of Corrections. https://nicic.gov/resources/nic-library/all-library-items/national-study-jail-suicide-20-years-later
Kupers, T. (1999). The mentally ill behind bars. In Prison madness: The mental health crisis behind bars and what we must do about it. Jossey-Bass, Inc.
Suicide Prevention Resource Center. (2011). The role of corrections professionals in preventing suicide. U.S. Department of Health and Human Services, Substance Abuse and Mental Health Services Administration (SAMHSA). https://www.insideprison.com/preventing-suicides-correctional-officers.pdf
Stop Glorifying Killers
Streaming services such as Netflix have been dramatizing multiple serial killers such as “Monster: The Jeffrey Dahmer Story” and “Extremely Wicked, Shockingly Evil and Vile,” a series about Ted Bundy’s life. Although these docuseries are supposed to give us insight into what took place, most audience viewers flip the narrative and boast about how “attractive” Bundy was or how they “feel bad” for Dahmer. No one seems to be discussing their victims, survivors, or the families of the victims. The trauma, PTSD, and grief that they must be experiencing while their stories are being televised for everyone to see. They continuously have to experience these popular actors portraying the person who has caused them harm in their lives by winning prestigious awards, getting continuous praise, and developing a fan base for the perpetrator.
Glorifying killers need to stop. Individuals such as Ryan Murphy need to take into consideration the people who were heavily affected by such tragedies. Murphy is best known for his writing, directing, and production of various popular television shows. With a lot of popularity under his belt, he decided to take on a new project: Jeffrey Dahmer. After the release of the docuseries, those affected by Dahmer came forward to give their take on the series. Isabell Lindsey, sister of victim Errol, was interviewed by the Hollywood Reporter when the docuseries debuted. Lindsey stated, “It brought back all the emotions I was feeling back then,” stating how traumatizing it was to have to relive it over again numerous times. She went further to state how Netflix or Murphy did not even reach out to her about the docuseries, “I feel like Netflix should’ve asked if we mind or how we felt about making it. They didn’t ask me anything. They just did it. I could even understand it if they gave some of the money to the victims’ children. The victims have children and grandchildren. If the show benefited them in some way, it wouldn’t feel so harsh and careless. It’s sad that they’re just making money off of this tragedy. That’s just greed” (Strause, 2022).
The casting of these killers is usually young and attractive. This captures a lot of young audiences’ attention. Such as Zac Efron who portrayed Ted Bundy and Evan Peters as Jeffrey Dahmer. Peters has worked with Murphy on different television shows such as American Horror Story. Peters has become known as a “heartthrob” and catches a lot of attention from young women. In season one of American Horror Story, Peters also played a character who committed a school shooting that was very similar to what happened during the Columbine Massacre. This episode was aired in 2011, just a year before the Sandy Hook massacre. Adam Lanza killed 26 people in 2012 and was known to be obsessed with Columbine. What was the purpose of truly airing this episode on television? Imagine being a victim of Columbine and seeing a dramatization of your tragedy being broadcasted for everyone to see? Audience’s will have their interest peak and will start to research the depiction of this. People already are idolizing Eric Harris and Dylan Klebold by dressing up as them for Halloween and essentially using them as inspiration to commit their own crimes. By doing so, the victims, survivors, and/or loved ones are not safe from the constant exploitation of what these killers have done to them and the rest of their lives.
The idolization of killers has been easier than ever due to the rise in curiosity and psychology behind “why they do it.” Documentaries are solely based on the perpetrator and not the victims. It is devastating to see how the stories can capture a lot of sympathy for the murderer, but viewers forget that this is about the victims. Having their stories displayed on different screens in people’s living rooms only for the audience to sympathize with the killer must be devastating. They do not think about the pain and trauma that the victims, loved ones, and survivors must be going through seeing their stories be streamed for everyone to see. Their stories are an open book at the touch of our fingertips. Worst of all, they have to witness it all unfold again. Reliving the horrible acts bestowed onto them only for them to realize, no one is talking about them, they are talking about the murderers.
Strause, J. (2022, September 28). Jeffrey Dahmer Victim’s family speaks out about the Netflix series. The Hollywood Reporter. https://www.hollywoodreporter.com/tv/tv-news/jeffrey-dahmer-netflix-tv-show-victim-family-speaks-out-1235228196/