Category: Research
Harvard Business Review Publishes our Opinion Article on Predictive Health Analytics
The Harvard Business Review has published our opinion article describing “How Machine Learning Is Helping Us Predict Heart Disease and Diabetes.”
ICRA 2016 Paper is Finalist for Best Paper Award
The paper “Cooperative Multi-Quadrotor Pursuit of an Evader in an Environment with No-Fly Zones”, by Alyssa Pierson, Armin Ataei, Ioannis Paschalidis, and Mac Schwager, which appeared in the Proceedings of the IEEE International Conference on Robotics and Automation (ICRA), May 16-21, 2016, Stockholm, Sweden, was a finalist for the conference Best Paper Award.
A video demonstrating the algorithm in the paper:
Clinicians and Computer Scientists Come Together to Predict Health Outcomes
Some things in life, like sunrises and sunsets, are predictable. Others, like traffic or the weather, are much harder to predict. Health outcomes tend to fall somewhere in the middle, but Bill Adams, MD, a Boston Medical Center pediatrician, and Yannis Paschalidis, PhD, a Boston University data scientist, are attempting to make more health outcomes predictable with an algorithm that utilizes electronic medical record data.
Their system, which is funded by a five-year grant from the National Science Foundation, utilizes anonymous data from BMC patients, which is stored in a database called I2B2. This data dates back to 2000 and includes diagnoses, procedures, admissions, length of stay, and basic demographic data. Adams had been using this data to study what works and what doesn’t work in terms of health outcomes for urban patients and teamed up with Paschalidis and a team of graduate students to develop and test algorithms that can identify opportunities to alter health outcomes, some of which might be missed by researchers. Currently the team is working on an algorithm to predict whether individual patients with a history of heart disease will be hospitalized within a year. In testing this algorithm, they have been able to predict approximately 80 percent of hospitalizations.
“The health care system is not very efficient,” says Paschalidis. “We spend lots of money on diseases that can be prevented. With an algorithm that can predict re-hospitalization of high-risk patients, doctors can pay more attention to those patients, and potentially prevent the predicted hospitalization. Hospitalization is very expensive, but other health care costs are modest, so predicting re-hospitalization and preventing it is better for both patients in terms of health and hospitals in terms of costs. In fact, the National Institutes of Health found that $30 billion is spent in the U.S. every year on preventable hospitalizations, so we have the opportunity to save huge amounts of money.”
The goal is to have algorithms that will run in the background when providers see patients and alert providers when something in a patient’s record suggests that he or she is at risk of a negative health outcome. It would prompt doctors to intervene during visits and case managers (if applicable) to intervene outside of doctor visits.
“While some risk factors, like smoking, are obvious to doctors, there are some, such as trends in laboratory data, that are harder to see,” says Adams. “The challenge in medicine isn’t to know that someone is high risk, but to know what type of risk they have and how to intervene. Our algorithm is a useful tool to help doctors intervene early before negative outcomes happen, instead of waiting for them to happen and then starting treatment.”
The heart disease algorithm primarily uses outpatient data to make predictions, because most long-term health outcomes are treated in outpatient settings. Currently the algorithm pulls in data from Logician, and STK, the hospital’s registration system, but soon will begin adding information from eMERGE now that the new electronic medical record system is live across the hospital. While the new system won’t change the type of data that the algorithm uses, it will allow the researchers to share their work with people across the country who also use Epic electronic medical records. It will also allow researchers to better integrate inpatient and outpatient data.
The software built on the algorithm is not in use yet, but Adams and Paschalidis expect to finish testing by the end of the year and start running focus group tests with BMC doctors next year. These groups will allow Adams and Paschalidis to refine the type of information their algorithm uncovers and how the data is presented to providers, to create a valuable tool. They also plan to expand the use of the algorithm to include diabetes patients and are in talks with the Department of Surgery to predict re-hospitalization of patients who have undergone surgery – this is an important metric for Medicare quality measures. Eventually the goal is to create an algorithm that can provide recommendations for intervention, which will involve further partnerships between providers and computer scientists.
“This is a cutting-edge approach,” says Adams. “There is general interest across the country in trying to use electronic data to predict health outcomes, but the BMC/BU team is special in that it combines the clinical expertise of the medical campus with expertise in engineering and computer science from BU. In addition, this type of project is not something generally undertaken in safety net hospitals, which makes our algorithm unique. Our goal is to make this data into something meaningful and useful for the direct care of our patients, and while we’re not there yet, I believe we will be soon.”
(The story appeared at the May 15, 2015, Volume 4, Issue 6, Boston Medical Center Brief.)
Big Data Improving Health Care
Data scientist and physician team up to reduce preventable hospitalizations
By Suzanne Jacobs, BU Research

Big Data Meets Healthcare: Bill Adams, a physician and medical informatician, and Yannis Paschalidis, a data scientist and engineer, are working together to use data from electronic health records to reduce preventable hospitalizations and cut health care costs. Photo by Jackie Ricciardi
Big Data Meets Healthcare: Bill Adams, a physician and medical informatician, and Yannis Paschalidis, a data scientist and engineer, are working together to use data from electronic health records to reduce preventable hospitalizations and cut health care costs. Photo by Jackie Ricciardi
Professor Yannis Paschalidis (ECE, SE, BME), a data scientist, has built a career on making things run smoothly and efficiently—transportation systems, communication networks, supply chains, sensor networks—and now he’s taking on perhaps his most ambitious challenge yet: the US health care system.
It all started about three years ago. Paschalidis, a Distinguished Faculty Fellow at Boston University’s College of Engineering (ENG), read in a study by the US Department of Health and Human Service’s Agency for Healthcare Research and Quality (AHRQ) that in 2006, the US spent about $30.8 billion on hospitalizations that could have been prevented through better patient care, healthier patient behavior, or improved ambulatory services.
“I was reading a lot of things about the sorry state of the health care system in the US and how inefficient it is, and I thought it’s an opportunity to do something,” says Paschalidis, who also directs BU’s Center for Information & Systems Engineering. “I thought people like me that have a quantitative, more optimization-oriented background could contribute something.”
And so, having never worked in medicine before, Paschalidis teamed up with William G. Adams, a Boston Medical Center (BMC) physician and BU School of Medicine professor of pediatrics. With a team of graduate students and nearly $2 million from the National Science Foundation, the two set out to build a piece of software that could automatically flag patients at increased risk for medical emergencies by using data from their electronic health records (EHRs). They decided to start with heart diseases, which alone cost the US more than $9.5 billion in preventable hospitalizations in 2006, according to the AHRQ study.
To understand how Paschalidis works, think of how an autopilot controls an airplane. As a plane flies, autopilot software takes in data about its position and uses that data to adjust the plane’s trajectory as necessary. It’s a constant flow of data intake, analysis, and feedback. Similarly, when Paschalidis sets out to improve, say, a network of sensors, he and his research team write computer software that takes in data about how the system is working and then finds ways to correct or improve it.
In this project, hospital patients are the systems.
Fortunately, EHRs offer plenty of data—test results, diagnoses, prescriptions, emergency room (ER) visits, previous hospitalizations, demographic information. It’s far too much for doctors and nurses to comb through manually, but enough to feed an algorithm that automatically processes the information and flags at-risk patients. The software works by sifting through records of patients who were previously hospitalized and learning which risk factor—a certain number of chest complaints or an unusual level of a particular enzyme in the heart, for example—might have been red flags. The algorithm then uses those red flags to warn of future hospitalizations.
The challenge for Paschalidis was understanding how to properly use medical data and how to incorporate this kind of software in an actual hospital. That’s where Adams comes in.
A pediatrician and medical informatician (someone who uses information technology to improve health care), Adams has spent the past 20 years thinking about how to use data from EHRs to improve patients’ health outcomes, especially among families in Boston’s urban communities. He’s also one of the lead scientists at BU’s Clinical & Translational Science Institute (CTSI), one of 60 such sites across the country that aim to accelerate medical advances by encouraging researchers in disparate fields to collaborate on medical research.
“This is a perfect example of translational research collaboration,” Adams says. “Yannis and his lab have exceptional skills in data mining that we don’t have, but we have extraordinary data and clinical expertise.”
To use that data, Paschalidis and his team first needed a crash course in medical terminology to make sure they understood what they were working with. Much of EHR data is contained in a kind of “clinical language” that only doctors understand, Adams says. Sometimes, he says, even the same term can have different meanings, depending on the context in which the doctor records it. For example, a diagnosis of hypertension (high blood pressure) can be recorded as either a diagnosis made during a visit or a problem on the patient’s problem list. Both could be recorded with the same code (ICD-9 401.9), but users would need to know to look further to decide which of the two meanings the data represents. Cleaning up “messy” data—figuring out what it means, what to use, and how to represent it in the software—is time-consuming but important, Paschalidis says. “If you fit garbage to an algorithm,” he says, “you’ll get garbage as output.”
The researchers remove any identifying information from the EHRs using open-source software from a National Institutes of Health-funded center at Harvard University called i2b2 (Informatics for Integrating Biology & the Bedside).
Once the data is cleaned up and anonymized, Paschalidis and his graduate students can enter it into their software. The algorithm they built classifies patients as either at risk or not at risk for heart-related hospitalizations within one year. An elderly patient or someone who visited the ER in the previous year, for example, might be at risk, while a younger person who hasn’t been to the hospital in a few years might not be at risk. How the algorithm will ultimately present this information to doctors is still under development.
To test the software, Paschalidis and his students collected the EHRs of just over 45,500 patients from BMC. They used about 60 percent of the records to train their so-called machine learning software, teaching it which factors had put patients at risk for hospitalizations in the past. Then, they used the remaining data to test the software’s ability to make predictions. They found that it could correctly predict up to 82 percent of heart-related hospitalizations, while falsely predicting hospitalizations in about 30 percent of patients who weren’t actually at risk. Paschalidis says that it’s possible to reduce the number of false predictions, but doing so would correspondingly lower the number of accurate predictions. A false prediction rate of 10 percent, for example, would correspond to an accurate prediction rate of 65 percent.
“In medicine, we’re constantly trying to balance between something that’s concerning and something that might be a false positive,” Adams says. In many cases, however, the recommendations that would come of a false positive—healthy eating, exercise, an extra check-in with the doctor, extra visits from a nurse—could still benefit the patient. And, Paschalidis says, preventing hospital visits that each cost thousands of dollars is worth the occasional unnecessary checkup that only costs a couple hundred dollars.
Adams and Paschalidis published their findings about the machine learning software’s success in predicting heart-related hospitalizations in March 2015 in the International Journal of Medical Informatics. Their co-authors included Professor Venkatesh Saligrama (ECE, SE); Wuyang Dai and Theodora Brisimi, ENG PhD students working with Paschalidis; and Theofanie Mela, a cardiologist at Massachusetts General Hospital.
“If coupled with preventive interventions, our methods have the potential to prevent a significant number of hospitalizations by identifying patients at greatest risk and enhancing their patient care before they are hospitalized,” the researchers write in the study. “This can lead to better patient care, but also to substantial health care cost savings. In particular, if even a small fraction of the $30.8 billion spent annually on preventable hospitalizations can be realized in savings, this would offer significant results.”
Ultimately, Adams says, having this kind of ongoing, automated analysis within electronic medical records could not only help doctors, nurses, and case managers monitor their patients more effectively, it could also elucidate disease risk factors previously undetected by doctors.
“All of us know that a serious problem like diabetes is always going to increase your likelihood of being admitted to the hospital,” Adams says, “but the trick is to determine whether it’s about the thing that’s happening to your diabetes or something else unrelated to your diabetes that has substantially increased the likelihood of being hospitalized. The machine learning software has the potential to learn new associations.” These could be associations between some clinical features that make it more likely for the patient to develop serious complications from diabetes.
In the coming year, Paschalidis and Adams will be interviewing doctors, trying to figure out how best to put this kind of predictive software to work in an actual hospital.
“I’m confident that it will work,” Paschalidis says. “The issue is, what is the best way of incorporating something like that in the practice? Will the doctors use it or ignore it?”
Eventually, Paschalidis says, he’d like to expand the software to predict other, non-heart-related hospitalizations. He’s also currently working with BMC’s surgery department on software designed to flag patients at risk for readmission within 90 days, so hospitals could perhaps monitor those patients more closely. The 90-day window is of particular interest to hospitals because Medicare doesn’t reimburse for readmissions within that timeframe.
Down the road, Paschalidis says, it might also be possible to use data from wearable technologies in addition to EHR data. The data is there, he says; it’s just a matter of getting access to it.
“We carry these smartphones and now these smart watches and all of these fitness trackers and other devices that know much more than the hospital knows about our state of health,” he says. “You now have a much richer record about the patient, and the richer the record is, the better prediction you can make.”
Throughout his career, Paschalidis has put his data analysis skills to use in a lot of different areas. For the past three years, he’s been applying those skills to developing sensor networks for “smart cities.” He says he thinks he’ll be working in health care for a while.
“I feel that health care is an important area,” he says, “and the contributions that you make are somehow more tangible in terms of the potential outcome.”
The story was originally published at BU research and was highlighted as News from the Field by the National Science Foundation.
Boston is Becoming a “Smart City” with ENG Support
IBM & IEEE recognize ECE & SE research contributions that are expected to improve urban life in Boston.
By Gabriella McNevin

Ushered in with the 21st century, are challenges that require real technological innovations. The global population is growing and, like magnets, people are moving to cities. According to the UN, by 2030, 60% of the population will live in a city, and by 2050, 70% (source). City officials are taking measures to adapt to the steadily increasing population. Today, Boston is zeroing in on population sustainability issues that threaten driver safety and drain energy: Inadequate road infrastructure and an antiquated repair system.
As part of a multifaceted collaboration to create technology to solve urban problems, the City of Boston and a Boston University-led team of researchers have developed equipment to improve the local thoroughfare, called “Street Bump.”
IBM and IEEE has recognized “Street Bump” as a significant contribution to Boston, and have presented the developers the second place prize in “IBM Students for a Smarter Planet/IEEE Smarter Planet Challenge: Student Projects Changing the World.” The team’s project, entitled,“Street Bumps and Big Data Analytics: Crowdsourcing Our Way to Better Roads,” demonstrates engineering expertise and a commitment to improving the world.
The team of researchers includes graduate students Theodora Brisimi (ECE), Yue Zhang (SE), Wuyang Dai (ECE), Setareh Ariafar (SE) and Nicholas Baladis (MIT). Professor Christos Cassandras (ECE, SE) and Professor Ioannis Paschalidis (ECE, SE, BME) are team advisors. All BU researchers are affiliated with the Center for Information and Systems Engineering.
The project focuses on an iPhone app – “Street Bump” – developed by the City of Boston to collect data on road conditions. The app is used by city employees and many citizens and was designed to facilitate crowdsourcing in collecting relevant road condition data. It uses the iPhone’s accelerometer to detect “bumps” sensed during a trip. The app then transmits the data to the City of Boston. The information can be used to alert repair crews of road damage. The algorithms developed by the BU-led team analyze the data received by the City and classifies the detected bumps into “actionable” and “non-actionable.” Severe bumps like potholes are actionable and can be prioritized in scheduling repairs.
In this work, the team collaborated with The City of Boston’s Office of New Urban Mechanics, which provided actual data from the City’s servers. Office Co-Chair Nigel Jacob and Chris Osgood have echoed the Office’s website saying, “there is a revolution going on in how cities are designed & built. This new focus on technology infrastructure and sustainable design links how a city is built with how it is managed and experienced.”
“Street Bump” is the second smart city application Professor Casssandras has advised that received national attention. The first app, Smart Parking, also won 2nd place in the “IBM Students for a Smarter Planet/IEEE Smarter Planet Challenge: Student Projects Changing the World” competition in 2011.
BU Bringham & Women’s Hospital Partnership Celebrates First Year
Joint Research Focused on Medical Imaging and Image-Guided Interventions
By Mark Dwortzan
 Researchers from Boston University and Brigham & Women's Hospital are collaborating to improve medical imaging and image-guided interventions. (Images courtesy of Brigham & Women's Hospital)
Researchers from Boston University and Brigham & Women's Hospital are collaborating to improve medical imaging and image-guided interventions. (Images courtesy of Brigham & Women's Hospital)
Boston University College of Engineering Assistant Professor Darren Roblyer (BME) and Brigham & Women’s Hospital radiologist Srinivisan Mukundan are exploring a strategy that combines a new optical imaging device developed by Roblyer with emerging magnetic resonance imaging (MRI) techniques to probe malignant brain tumors during chemotherapy treatment. Their research could enable clinicians to monitor the effectiveness of chemotherapy over the course of treatment and implement changes to chemotherapy drugs and dose levels as needed.
The project is one of five now receiving funding through an ongoing partnership between Boston University and Brigham & Women’s Hospital. On September 12 at the BU Photonics Center, Dean Kenneth R. Lutchen and Dr. Steven Seltzer, Chair of the BWH Department of Radiology, announced the second year of the partnership, which has already provided one year of seed funding to projects ranging from image-guided cancer drug delivery to early detection of heart disease.
 “The goal is to leverage synergies between Brigham & Women’s Hospital’s Radiology Department in imaging and image-guided interventions with the College of Engineering’s strengths in developing new materials and technologies as well as novel techniques for processing images and large data sets,” said Associate Professor Tyrone Porter (ME, BME, MSE), who is coordinating the partnership. “The hope is to stimulate research collaborations between the two campuses and develop a National Institutes of Health training program in clinical imaging and image-guided interventions.”
“The goal is to leverage synergies between Brigham & Women’s Hospital’s Radiology Department in imaging and image-guided interventions with the College of Engineering’s strengths in developing new materials and technologies as well as novel techniques for processing images and large data sets,” said Associate Professor Tyrone Porter (ME, BME, MSE), who is coordinating the partnership. “The hope is to stimulate research collaborations between the two campuses and develop a National Institutes of Health training program in clinical imaging and image-guided interventions.”
The brainchild of Lutchen and Seltzer, the BU-BWH partnership brings together world-class expertise and equipment from Boston University entities such as the BU Photonics Center and the BU Center for Nanoscience & Nanobiotechnology, and from the BWH Department of Radiology, home to the National Institutes of Health’s National Center for Image-Guided Therapy and the Advanced Multimodality Image Guided Operating Suite (AMIGO). Joint research between the two campuses could result in less invasive, more accurate medical imaging and image-guided interventions.
“There’s no question that in so many dimensions, imaging is at the foundation of a tremendous amount of potential breakthroughs in medical discoveries and practice, but there are huge challenges from a scientific and technical point of view,” said Lutchen. “We’ve got tons of interested students and faculty here that need and want to use imaging technologies to address interesting and important questions.”
First-round projects include the engineering of a new “molecular imaging” MRI contrast agent for detecting early calcification of the aortic valve; the combination of ultrasound and MR data to evaluate the elastic properties of tissues, which are associated with pathological indicators of disease; a clinical decision support system for patient-specific cancer diagnosis and management; and ultrasound-guided delivery of chemotherapy drug-laden nanoparticles to metastasized lung cancer cells in the brain. Applications for second-round projects are now underway.
All projects involve at least one principal investigator from each of the partnering institutions, who jointly advise a doctoral student on a project that could positively impact clinical practice. Participating ENG faculty include Professors Joyce Wong (BME, MSE), Paul Barbone (ME, MSE), Venkatesh Saligrama (ECE, SE) and Yannis Paschalidis (ECE, SE); Associate Professor Porter; and Assistant Professor Roblyer.
“The fields of biomedical imaging and bioengineering have been converging and collaborating for decades, and that collaboration continues to get closer and closer,” said Seltzer, noting a burgeoning clinical need for advanced technologies in functional and molecular imaging; information technologies ranging from data mining to image processing; and minimally-invasive diagnostic and therapeutic procedures guided by high-technology imaging techniques.
Top Ranked ENG Algorithms Could Reveal New Cancer Drug Target
by Mark Dwortzan
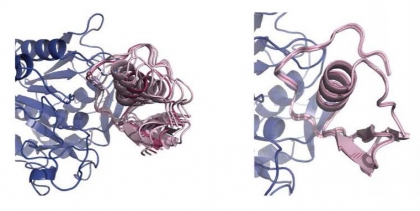
An interdisciplinary College of Engineering team has developed computational methods to predict the structures that form when two cellular proteins interact. Judged the world�s best at a major international competition, these methods have drawn more than $3 million in NIH funding.
An interdisciplinary College of Engineering team has developed computational methods to predict the structures that form when two cellular proteins interact. Judged the world's best at a major international competition, these methods have drawn more than $3 million in NIH funding.
An interdisciplinary team of College of Engineering faculty members—Professor Sandor Vajda and Research Assistant Professor Dima Kozakov (both BME), Professor Ioannis Paschalidis (ECE) and Associate Professor Pirooz Vakili (ME)—has developed a family of powerful optimization algorithms for predicting the structures of complexes that form when two cell proteins bond together—structures that, in some cases, generate erroneous cell signaling pathways that can trigger cancer and other inflammatory diseases. Recognizing the promise of these computational methods to advance new approaches to combating these illnesses, the National Institutes of Health (NIH)-National Institute of General Medical Sciences (NIGMS) recently approved a $1.6 million, five-year grant that will enable the researchers to continue refining them.
A joint effort of Boston University’s Center for Information and Systems Engineering and Biomolecular Engineering Research Center, the project combines Paschalidis’ and Vakili’s expertise in optimization and systems theory with Vajda and Kozakov’s knowledge of biophysics and bioinformatics.
“Given the three-dimensional structure of two proteins, you’d like to predict with great accuracy the structure of the complex formed once these two proteins bind,” said Paschalidis, who compares the process to characterizing all the possible structures that pairs of Lego blocks can form out of an initial set of 1,000 blocks. “Based on laws of thermodynamics, we’ve developed optimization algorithms that have succeeded in doing just that.”
Applying those high-precision algorithms to a related effort, Vajda and Kozakov are also collaborating with BU Associate Professor Adrian Whitty, Professor John Porco, Professor Karen Allen, and Research Assistant Professor Aaron Beeler (all Department of Chemistry); and Professor Gilmore (Department of Biology) to identify small molecules—potential drugs—that can disrupt protein-protein interactions (PPIs) that produce structures that may provoke illness.
Operating under a separate, four-year, $1.6 million NIH-NIGMS grant, the BU team aims to develop synthetic molecules that inhibit PPI targets at sites identified by Vajda’s and Kozakov’s innovative computational approaches—without introducing any harmful side effects. In particular, the researchers are attempting to design novel molecules that can block chronically hyperactive cell signaling pathways found in human inflammatory diseases and cancers.
Despite decades of effort by the pharmaceutical industry, it has proven extraordinarily difficult to develop oral drugs that inhibit PPIs, Vajda observed. “Current protein-based drugs can disrupt PPIs, but only on the surface of cells,” he said. “But 90 percent of PPIs occur within the cell, and these are the interactions that we’re working to disrupt.”
ENG Algorithms Judged the World’s Best
The NIH is funding the development and application of these advanced computational methods because scientists cannot easily observe the complexes formed by protein-protein interactions. Many biologically important PPIs produce fragile complexes that do not remain intact long enough to be subject to direct experimental analysis, but optimization algorithms such as those developed by the ENG team can determine the structure of these complexes with great accuracy based on the structures of the component proteins.
As the team improves its methods, they will ultimately be incorporated into Vajda’s and Kozakov’s protein-protein docking server ClusPro, a website to which any user can submit the three-dimensional coordinates of two proteins and receive a supercomputer-calculated prediction of the structure of the complex formed by those proteins. ClusPro has been used by over 3000 research groups worldwide, and generated over 100 structures reported in the scientific literature.
In a worldwide blind prediction experiment conducted by CAPRI (Critical Assessment of Predicted Interactions) in Barcelona last December, judges determined that the ENG team’s computational methods delivered the best performance in modeling selected protein-protein complexes when compared against 64 other predictor groups that combine software models with human analysis, and that ClusPro also performed better than nine other competing automated docking servers, which rely on software alone. Results of the CAPRI experiment will be published in a special issue of the journal Proteins: Structure, Function, and Bioinformatics in November.
Interdisciplinary Team Sheds Light on How Proteins Bind
Finding Could Open Up New Drug Discovery Opportunities
By Mark Dwortzan
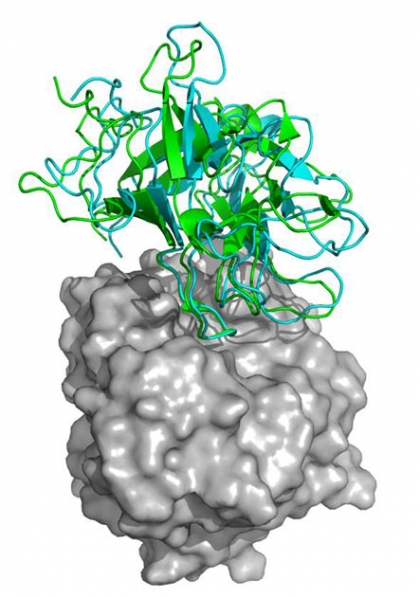
"Transient encounter complexes" of an enzyme produced by a bacterium present in the human gut binding to a fragment of a protein in turkey eggs which inhibits the enzyme.
Over the past six years, an interdisciplinary team of College of Engineering faculty members—Professor Sandor Vajda (BME, SE), Research Assistant Professor Dima Kozakov (BME), Professor Yannis Paschalidis (ECE, SE) and Associate Professor Pirooz Vakili (ME, SE)—have been developing a set of powerful optimization algorithms for predicting the structures of complexes that form when two proteins bind together—structures that, in some cases, generate erroneous cell signaling pathways that can trigger cancer and other inflammatory diseases.
Incorporated into Vajda’s and Kozakov’s protein-protein docking server ClusPro—a website to which any user can submit the three-dimensional coordinates of two proteins and receive a supercomputer-calculated prediction of the structure of the complex formed by those proteins—these algorithms have enabled more than 3,000 research groups across the globe to better understand the inner-workings of the cell and explore potential drug targets without having to run expensive, time-consuming lab experiments.
Now the research team behind these algorithms has, through lab experiments and computational analysis, obtained a sharper understanding of how two proteins come together to form a complex, and plans to apply that knowledge to boost the speed and accuracy of ClusPro’s predictions. They and collaborators from the Hebrew University of Jerusalem and the National Institutes of Health (NIH) report on this new development in a new article in eLife, an open source journal for outstanding biomedical research.
A joint effort of Boston University’s Center for Information and Systems Engineering and Biomolecular Engineering Research Center supported by a five-year, $1.6 million grant from the NIH, the project combines Paschalidis’ and Vakili’s expertise in optimization and systems theory with Vajda and Kozakov’s knowledge of biophysics and bioinformatics.
“The research was a beautiful combination of physics with mathematics,” said Paschalidis. “We leveraged techniques popular in control systems developed to describe movement of complex 3-D objects, such as a robot arm, as well as machine learning methods used to analyze large data sets.”
“Preventing proteins from binding to the wrong partners is an increasingly prominent concept in drug design,” said Janna Wehrle, PhD, of the NIH National Institute of General Medical Sciences, which partially funded the research. “These new computational methods developed by the Boston University team will help researchers quickly discover both healthy protein pairs and disease-causing pairs that we might want to break up.”
Until now, scientists were unable to characterize how protein-protein complexes form from two individual proteins—each analogous to a distinctly-shaped Lego block—because their interactions from the moment they come in contact to the moment they “snap into place” were too fast to detect. But an emerging nuclear magnetic resonance (NMR) technique has made it possible to track their rapidly changing configurations from rendezvous to docking using radio waves.
Applying this technique, the College of Engineering team determined that its protein-protein docking algorithms were already generating these exact transitional states, but labelling them as “false positives” alongside the correctly identified final protein-protein complex.
“What we have so far been calling false positives are ‘transient encounter complexes,’ temporary structures the proteins form as they ‘search’ for the one orientation that will enable them to bind successfully,” said Paschalidis.
All protein-protein encounter complexes are characterized by low energy, with the lowest energy expected to occur at the final, stable complex. By systematically analyzing the energy values corresponding to the transient complexes, the researchers found that with each successive interaction, the intersecting proteins have fewer and fewer ways to twist and turn, thereby accelerating their path to binding. This explains how two proteins can dock very quickly despite the many nooks and crannies that must line up to seal the deal.
The College of Engineering team next aims to exploit its findings to make its docking algorithms faster and more accurate. The researchers also plan to examine the implications of their work for protein-DNA and protein-small molecule interactions that are important in genetic regulation and drug discovery, respectively.
See movie of transient protein-protein encounter complexes.
BU, research universities hit by international cyber attacks
Written by Drew Schwartz
One of Boston University’s public web pages suffered a cyber attack from an unidentified, internationally-based source last week, said BU’s Information Security Team Executive Director Quinn Shamblin.
Shamblin said the attack was directed at the search bar function on one of BU’s web pages. He said the attack caused the web page’s service to slow down, but there was no indication whether the indivdiual or group responsible stole any of BU’s information.
“It [the attack] was a particular group having found a form on BU servers,” Shamblin said. “They were trying to see if they could get that form to give them information that they shouldn’t have had.”
A cyber attack is any event where an external agency or person tries to use or gain access to resources in an unauthorized way, Shamblin said. Cyber attackers usually target the intellectual property of governmental, corporate or university web pages.
After a barrage of cyber attacks hit American research universities this past summer, campuses across the nation have been forced to tighten Internet security measures, according to a July article in The New York Times. Shamblin said BU’s network occasionally such cyber attacks, and that InfoSec utilizes several defense techniques to ensure the university’s information is secured.
“We get attacks all the time because that’s just how the Internet works,” Shamblin said. “We [InfoSec] work with the FBI [Federal Bureau of Investigation] … U.S. Secret Service … local law enforcement as needed … We will call them as appropriate with full cooperation of our general counsel and appropriate other groups inside of the university.”
Shamblin said BU students and faculty should keep their computers’ operating systems updated to defend themselves against these attacks.
“We want to make sure that if somebody wants to try to get access to sensitive information — or wants to try to break into your personal machine — they have to go through multiple layers of security,” Shamblin said. “The point of it is to make it such a pain in the butt that they [cyber attackers] won’t waste their time, and they’ll go somewhere else.”
Christos Cassandras, head of BU’s Divisions of Systems Engineering said, although BU’s InfoSec department successfully stopped last week’s cyber attack, they may not always know when their system is being attacked.
“It could be that somebody had sent those malicious [programs] into your computer two weeks ago, and you still don’t know anything about it,” Cassandras said. “There are so many different ways [to execute cyber attacks] and new ones are being invented every day. It’s a little bit like the Cold War … As soon as somebody discovers a new weapon, we find out the counter to this weapon.”
Cassandras said although university officials have taken measures to ensure the safety of their servers, unattended computers at BU are highly vulnerable to attackers.
“The biggest threat, I think, is that we have a lot of computers in universities, including BU, that are sitting around in labs and doing things without continuous supervision,” Cassandras said. “During that time that the computer isn’t being supervised, someone can take over that computer.”
Ionnas Paschalidis, co-director of BU’s Center for Information and Systems Engineering, said cyber security is a growing concern for universities such as BU that are involved in classified research.
“The vast majority of research at universities eventually is being made public …. But before they publish, they don’t want their research to be made public,” Paschalidis said. “It’s a growing concern not only in universities, but throughout our society as we depend much more on services that are online … Every aspect of our lives is now connected to a network one way or the other. This creates much more serious consequences for cyber-attacks.”
Better Data Management, Lower Healthcare Costs
By Rachel Harrington
Today, people with chronic conditions like diabetes are benefitting from real-time monitoring devices like miniaturized implants, home monitoring equipment, and smartphone applications. Unfortunately, even though tracking a person’s symptoms and vitals has improved, hospitals and their medical teams are not ready to benefit from possessing so much personalized health data.
Boston University’s Professor Ioannis Paschalidis (ECE/SE)and Dr. William Adams (BMC) have teamed up with MIT’s Professor Dimitris Bertsimas to develop algorithms that can systematically process all patient data in hospital electronic medical records and personalized health records. These algorithms will be designed to classify patients based on the risk of developing an acute condition that would require hospitalization. Such information can then be used to drive preventive actions.

“What motivated us to start this particular project is the recognition that the US health care system is extremely inefficient as it is geared toward treating acute conditions,” said Paschalidis. “There are, we believe, tremendous opportunities for preventing the occurrence of these conditions and the expensive hospitalizations they cause.”
To support their work, the National Science Foundation (NSF) has awarded Paschalidis (PI), Adams (Co-PI), and Bertsimas (Co-PI) a five-year, nearly $2 million grant for the project.
By focusing on disease prevention and keeping patients out of the hospital, their work has the potential to improve a healthcare system that is often considered to be very expensive and highly inefficient.
“To that end, the meaningful use of electronic health records is seen as a key to improving efficiency,” the team wrote in their proposal.
The research will utilize Paschalidis’s expertise in data models, optimization and decision theory, but it is truly a collaborative project. Adams, for example, will work with physicians to get feedback on the outcome of the algorithms.
“The main challenge is going to be the adoption of the techniques we develop by physicians in particular and the healthcare system in general,” Paschalidis said. “Dr. Adams will serve as our ambassador to that community.”
Adams said that the Boston Medical Center has spent more than ten years “developing a robust and rich clinical informatics infrastructure for clinical care and research” and welcomes this new partnership.
“Translational science involves collaborative efforts between traditionally independent scientists,” Adams said. “This project is innovative and important in that it brings together mathematicians, engineers, clinicians, and informaticians to better understand and improve healthcare.”
As healthcare costs increase, their research may prove not only to be timely but also life-changing and cost-effective.


