Home
Family Trauma, Media and Police Interactions
Police interactions with the public have always been a highly conversed issue. Recently, due to events in the United States, there has been an increase scrutiny in regards to police interactions with the public. The media and the general public have been quick to glorify the notion that police are under-trained and not equipped to effectively deal with the public. One negative interaction with the public can ultimately affect the public’s perception of a police service.
Recently in the Region of Peel (region directly west of Toronto, Canada) officers have been scrutinized for their interaction with D’Andre Campbell, a 26 year old man. Officers responded to a home for the report of a domestic incident. This incident then escalated to the point where two officer’s tasered Campbell, this was then followed by one of the officers discharging his firearm multiple times. Campbell was pronounced dead at the scene. (CBC News, 2020).
Immediately after this incident, Campbell’s family called for more mental health training:
“According to the family, D'Andre Campbell was the one who called police to the home Monday. They said he had mental health issues and that police have been to the home numerous times in the past, so they should have known they were dealing with a mental health patient.” (Tong, 2020).
This statement led to immense media coverage on the issue, and the family appeared devastated and traumatized due to the interaction. The investigation is still on going and the Special Investigations Unit (SIU, civilian police oversight agency) has not yet released a report on their findings. The Toronto Star had been faulted for releasing a news article which stated Campbell as “unarmed.” (Yun, 2020). This news source attempted to scrutinize the officer’s for their interaction with a black man, and had to post a correction notice to their news article.
It is understandable for the public and family to be upset in regards to what has happened. However, it is unacceptable for media outlets to attempt to capitalize on the trauma that a family has experienced, and sway public opinion towards statements which are contradictory to facts. For example, in the City of Toronto, Toronto Police responded to approximately 1.8 million calls for service in 2016. Officers made approximately 9,000 mental health act apprehensions and 28,000 arrests. The SIU investigated 1 incident for every 27,729 contacts that police had with the public, and use of force was only required in a total of 3.9% of the services total arrests. (Vigilis, 2017). This shows that despite how the media wants to portray incidents, police are doing a relatively good job in deescalating situations and peacefully resolving incidents.
References:
CBC News. (2020, April 8). Man fatally shot by Peel police in Brampton identified as D'Andre Campbell. CBC News. Retrieved from https://www.cbc.ca/news/canada/toronto/brampton-shooting-d-andre-campbell-1.5527245
Tong, T. (2020, April 7). 'He was already on the floor': Family looks for answers after Ontario man shot dead by police. CTV News. Retrieved from https://toronto.ctvnews.ca/he-was-already-on-the-floor-family-looks-for-answers-after-ontario-man-shot-dead-by-police-1.4886751
Vigilis, S. (2017). Corporate Risk Management Annual Report. Retrieved from http://www.torontopolice.on.ca/publications/files/reports/crm2016annualreport.pdf
Yun, T. (2020, April 9). Peel police chief offers condolences after man fatally shot by police, acknowledges ‘issues of trust in policing.’ Toronto Star. Retrieved from https://www.thestar.com/news/gta/2020/04/09/peel-police-chief-offers-condolences-after-man-fatally-shot-by-police-acknowledges-issues-of-trust-in-policing.html
Post Traumatic Stress Disorder and Post Incarceration
Post Traumatic Stress Disorder and Post Incarceration
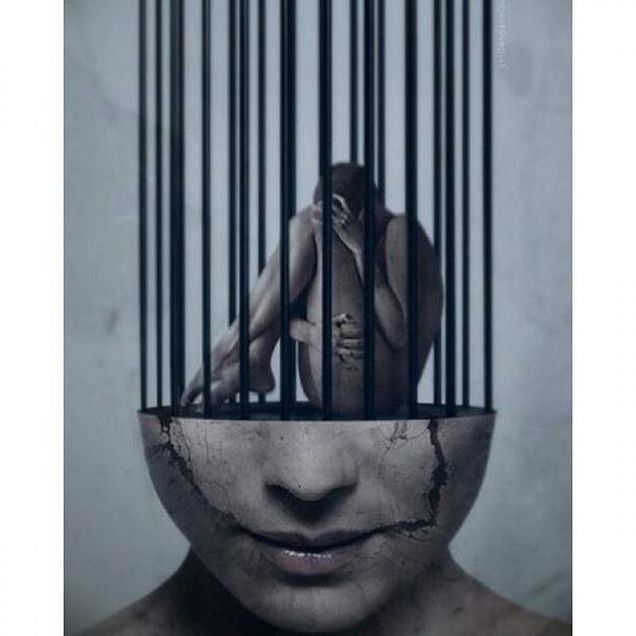
People enter into the prison system beaten battered and bruised by life. Trauma isn’t new for them. With little care and resources within many states, jails and prisons are the largest mental health providers in many counties and states (Rousseau, 2020) The trauma that is survived for many will become a form of PTSD-Post traumatic stress disorder.
“a condition of persistent mental and emotional stress occurring as a result of injury or severe psychological shock, typically involving disturbance of sleep and constant vivid recall of the experience, with dulled responses to others and to the outside world.” (OXford)
Of the 10.3 million prisoners worldwide approximately 750,000 are likely to have a clinical diagnosis of PTSD. (Branyi, Cassidy, Fazel, Priebe, & Mundt, 2018). PTSD conditions can often go unnoticed and may lay dormant for years before a life situation triggers it to the surface. The prison systems breed traumatic events, stressors, fear and psychological harm. Prison adversely impacts self-esteem, self worth, cognition and the human spirit. (Flood, 2018) While incarcerated many painful and devastating past memories may often be awakened due to the harsh conditions of a dehumanizing, uncaring lifestyle that prison life offers. These memories of past traumatic experiences, may cause a person to undergo crippling emotional reactions and pain. (Thomas, 2019)
Being incarcerated in general is traumatizing, the inhuman treatment, lack of compassion and suffrage of the daily routine is most difficult to survive but then you add past trauma coming to surface and living in repeated trauma daily. It is no surprise that each year more than 700,000 people leave prison having undergone a traumatic experience. When emerging from the prison system, many will return to society undiagnosed and untreated. (Flood, 2018)
Many will enter society unaware that they are institutionalized. “Institutionalization is used to describe the process by which inmates are shaped and transformed by the institutional environments in which they live.” (Rousseau, 2020) When a person enters the prison system they are required to conform to the everyday occurrence, if not they will be forced to obey the norms of the prison system. One must incorporate the norms of prison into their way of thinking and behaving. Prison is it’s own society with its own set of rules and protocol. The way you feel, the way you act, the way you interact needs to fall into step with the prison norms. This personal transformation is called ‘Institutionalization” It happens differently for each individual. The longer the person is sentenced, the more significant the transformation, weather consciously or unconsciously they are becoming ‘institutionalized”. It may happen over time or after several altercations/penalties. It is a forced conformity into an environment that has no privacy, no compassion, where you are deprived of emotion, touch, while controlled and dehumanized. (Rousseau, 2020)
It goes without saying that when a person is released life is no longer the same. You couple that with the loss of self identity, being labeled as a criminal, stigmatized as a felon, denied by society and you have a challenging transition into society. Support network through Reentry agencies provides a safe space for post-incarceration adjustment to take place. It allows people a chance to reacclimate into an environment where they have no judgement (Flood, 2018). Prison reentry programs provide a sense of belonging, structure and support for people coming out of prison. A program offers compassion, empathy and they are being treated as a human being. Again they are going through an adjustment to a new norm. A new sense of worth. The support of others is critical at this time.
As people find their way back into society's norms some may need something that has a meaning for them. They may choose to go into a field of work that allows them to help the next person. Thus giving them a sense of value and purpose. For others, being the voice for the ones left behind allows them to share their stories to educate and bring change for the ones left behind. (Flood, 2018)
PTSD is often a part of people’s lives and increases during release. Therefore, It is important as a community to open our hearts and minds to people who are returning to their communities. Support systems and compassion can make the difference between success and recidivism.
References
Branyi, G., Cassidy, M., Fazel, S., Priebe, S., & Mundt, A. P. (2018). Prevalence of Posttraumatic Stress Disorder in Prisoners. Epidemiologic reviews, 40(1), 134–145. https://doi.org/10.1093/epirev/mxx015
Flood, F. (2018). Reframing Trauma: The Transformative Power of Meaning in Life, Work, and Community. Journal of Psychiatry and Psychiatric Disorders, 02(05). doi:10.26502/jppd.2572-519x0052 Retreived from http://www.fortunejournals.com/articles/preframing-trauma-the-transformative-power-of-meaning-in-life-work-and-communityp.pdf
Post-Traumatic Stress Disorder: Definition of Post-Traumatic Stress Disorder by Oxford Dictionary on Lexico.com.(n.d.). Retrieved from https://www.lexico.com/definition/post-traumatic_stress_disorder
Rousseau, D. (2020) Lecture notes, Module 6: Trauma and the Criminal Justice System Retrieved from: https://onlinecampus.bu.edu/bbcswebdav/pid-7783372-dt-content-rid-37966315_1/courses/20sum1metcj720so1/course/module6/allpages.htm
Thomas, Liji. (2019, February 27). Prisoner Post Traumatic Stress. News-Medical. Retrieved on June 15, 2020 from https://www.news-medical.net/health/Prisoner-Post-Traumatic-Stress.aspx.
Strategies of Self-Care in Trauma
Strategies of Self-Care in Trauma

Trauma is collective to more than fifty per cent of the population, with a large per cent of traumatic events leading to mental disorders such as PTSD, depression, as well as inter-relation problems (Dorothy, 2017). Due to the intensity of the consequences of trauma, individuals experiencing this ordeal are advised to practice self-care to enhance their wellbeing. Self-care improves recovery through enhancing positive relationships and interactions between the patient and care providers. The paper will evaluate strategies for self-care to individuals experiencing trauma.
Self-Care Strategies
Self-care strategies can be grouped into three strategies; physical, relational, plus cognitive (Patricia et al., 2013). Physical strategies include physical exercises such as running, dance, and yoga, among others. These strategies are aimed at providing progressive relaxation methods to enable the patients to focus on something different. During exercise, there is deep breathing, exhaustion, and relaxation of muscles which gives an individual a new experience of thoughts, besides the traumatic ones. If an individual does not like exercises, one can go shopping, cook, or having an undisturbed sleep. The practices help in dealing with intense feelings plus emotions.
Relational strategies involve building trusting relationships among friends, peers, workmates, romantic partners, supervisors, or therapist (Patricia et al., 2013). Genuine relationships provide physical, emotional, and cognitive support. When a traumatic individual is in a relationship, they trust the people with their fears by confiding their feelings and emotions. Some individuals can become closer to their pets and spend more time with them. When among friends, activities such as cooking or exercising together help the victim to become more aware of themselves to find the courage to face their ordeal. It is in such relationships that people find a reason to laugh and get rid of stressors. Reading, meditating, and doing assignment are some of the relational activities that can help an individual to move out of the norm. Cognitive strategies include the use of premeditated distractions like movies and listening to music to distract one’s mind from stressors. Cognitive strategies limit the mind from traumatic experiences (Patricia et al., 2013). When among friends, one can focus on different topics that are unrelated to traumatic experiences. Some individuals may prefer meditation practices to remain present and calm their mind from deep thoughts. Others focus on concentrating on the positive occurrences in life to cheer them up. Other individuals focus on prayers and worship for spiritual nourishment to enable them to stay positive.
The overall strategies can be combined into one common group of stress management. An individual with experience in trauma needs to exercise stress management to prevent relapse (Alexis et al., 2019). Such individuals can find where their strengths lie and focus on it to remain positive. The activities, as mentioned above, act as boosters for tolerance, relaxation of the mind and discharge of negative energy. One can quickly recover from the trauma, minimize the possibility of burnouts, and releasing excessive energy that can lead to stress.
Conclusion
Self-care is vital to healing from trauma. It is an individual effort to ensure that all stressors are eliminated to avoid traumatic experiences. An individual can use friends, relatives, coworkers, and partners to confide on their emotions and stressful feelings that might lead to trauma. For an active recovery, self-care is an impetus to therapy and self-recovery. As such, care providers should focus on self-care more than therapeutic activities to enhance positive feelings.
References
Alexis, G. et al. (2019). Integrating self-care into clinical practice with trauma clients. Journal of Human Behavior in the Social Environment, 29(1): 48-56, doi:10.1080/10911359.2018.1473189
Dorothy, E. (2017). Optimizing Empathy: Physician self-care as a crucial component of trauma-informed treatment. Journal of Lifelong Learning Psychiatry, 15(4): 432-434. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6519522/
Patricia, J. et al. (2013). Developing Self-Care Practices in a Trauma Treatment Course. Journal of Social Work Education, 50(3): 440-453. http://dx.doi.org/10.1080/10437797.2014.917932
Self-Care Image retrieved on June 15, 2020, from: http://www.empowerireland.ie/uncategorized/self-care-in-social-care-vicarious-trauma-vicarious-resilience-and-self-compassion/attachment/highway-signpost-self-care/
Children with Adverse Experiences
Childhood trauma is much more common than we perceive. Each year millions of children across the United States experience some sort of trauma whether it is child abuse, neglect, exposure to violence, family alcohol or drug abuse, or poverty. It is great that we as a society know about the millions of children exposed to trauma, but what about the millions we do not know about? It is essential that we understand how childhood adversity creates negative, long-term effects on the child's mind and body. Turning a blind eye to childhood adversity has caused our nation to pay a tremendous human price, societal price, and economic price for the degree of childhood adversity and resilience our children experience.
In this article, the Lucile Packard Foundation for Children’s Health touches on the connection between brain structure and early experiences of trauma. The prefrontal cortex does not fully develop until about the age of 25 (Rousseau, 2020). The prefrontal cortex is responsible for a variety of complex cognitive behavior such as planning, personality expression, decision making, and moderating social behavior (Rousseau,2020). When an individual experiences trauma it causes developmental issues in the prefrontal cortex. Childhood adversity leads to the inability to self regulate emotion and disrupts healthy development in adulthood (Children Health, 2017). It also causes behavioral, emotional, school, and health problems during childhood and adolescence (Children Health, 2017). There is an 80% likelihood that if exposed to one of these categories as a child, an individual will experience alcoholism and alcohol abuse, chronic obstructive pulmonary disease, depression, drug use, heart disease, liver disease, risk of partner violence, smoking, suicide, and overall a decline in a healthy and robust quality of life (Rousseau, 2020).
Unlike many articles on Childhood adversity, the Lucile Packard Foundation for Children’s Health discusses the connection between resilience and children with adverse experiences. Resilience is defined as an adaptive response to hardship. In other words, a child's ability to recover and cope with adverse experiences. Many researchers do not touch on the topic of resilience, however it may play a major role in adverse childhood experiences. The Lucile Packard Foundation for Children’s Health explains that resilience involves a combination of internal and external factors (Children Health, 2017). Understanding the factors involved with resilience and how resilience is strengthened contributes to allowing society to better support a child recovering from trauma.
As mentioned previously, each year millions of children across the United States experience some sort of trauma. The Lucile Packard Foundation for Children’s Health does not simply discuss the adverse childhood experiences, but policy implications designed to help to prevent ACEs, as well as to ensure early identification and intervention for parents and children affected by trauma (Children Health, 2017). In the end, the Lucile Packard Foundation for Children’s Health demonstrates how developing policies and program options to help prevent, interrupt, and mitigate the effects of childhood adversity contributes to our ability to protect these children.
References :
“Childhood Adversity and Resilience Summary.” Kidsdata.org, 2017,
www.kidsdata.org/topic/95/childhood-adversity-and-resilience/summary?gclid=EAIaIQo
bChMIt7GbiqWF6gIVB0WGCh0zRAV0EAAYASAAEgIzWfD_BwE.
Rousseau, D. (2020). Module 2: Childhood Trauma. Retrieved from
https://onlinecampus.bu.edu/ultra/courses/_65989_1/cl/outline
Treatments for Trauma
There are a variety of treatments available for those who suffer from trauma. The three most common treatments are therapy, medications and holistic treatments. Forms of therapy can include cognitive behavior therapy, exposure therapy and eye movement desensitization and reprocessing. Medication can include anxiety medications, anti-depressants, and mood stabilizing medications. Some holistic treatments for someone who has experienced trauma can include meditation, yoga, acupuncture and other forms of physical activity.
While some individuals may prefer medications to help them overcome a past trauma, others may choose a form of therapy. Cognitive behavioral therapy (CBT) is a form of psychological treatment that has been demonstrated to be effective for a range of problems including depression, anxiety disorders, alcohol and drug use problems, and mental illnesses. CBT is conducted by repeatedly exposing patients to the stimulus they fear without bad things actually happening. Over time the patient will gradually become less upset or fearful, and the bad memories will then be associated with “corrective” information of being safe (van der kolk, 2015). In Professor Rousseau’s lecture she discusses how CBT helps patients unlearn their negative reactions to thoughts and replacing them with new emotional and behavioral responses in situations they find challenging (Rousseau, 2020). The goal of cognitive behavior therapy is to teach people that while they cannot control every aspect of the world around them, they can take control of how they interpret and deal with things in their environment.
Exposure therapy is great option for veterans or sexual abuse survivors. This form of therapy helps victims overcome whatever fear or trauma they are experiencing. The four stages of exposure therapy are: education, breathing, real world exposure and talking through the trauma. I believe each stage serves a different purpose and allows the patient to not only talk through their trauma, but also learn techniques on how to overcome their trauma (Rousseau, 2020). Although being exposed to their fear or trauma can be very challenging, it is done in a safe and controlled environment, to allow the patient to feel as comfortable as possible, but also getting them outside of their comfort zone, and become comfortable with being uncomfortable.
The last therapeutic approach that can help with trauma is Eye Movement Desensitization and Reprocessing (EMDR). EMDR is a form of psychotherapy that is often used to treat Post Traumatic Stress Disorder. It incorporates methods from Cognitive Behavioral Therapy (CBT) in addition to adding bilateral stimulation through Rapid Eye Movements (REM) (Roussea, 2020). When REM is incorporated into therapy, the patient will bring forth the traumatic memory as they recall how they are feeling. EMDR’s focus is to regulate the memory but also restore the memory throughout the patient’s body and mind (van der Kolk, 2014, pp 258). EMDR consists of eight different phases including history taking, preparation, assessment, desensitization, installation, body scan, and reevaluation (Rousseau, 2020). Without discussing each of these phases in detail, the individual ultimately brings up the negative memory and discusses surrounding emotions, senses, and negative beliefs that they experienced.

Many studies have found that both CBT and EMDR therapy are the most effective therapies for treating patients with PTSD associated trauma. I believe that EMDR is a great option for many patients who have been exposed to trauma because I believe that its eight-phase system is well thought out and each phase holds a specific purpose. While a form of therapy may not be the best option for you, there are many other ways to help assist you overcome trauma.
Rousseau, D. (2020). Module 4.6. [Lecture Notes]. Boston University. https://onlinecampus.bu.edu/ultra/courses/_65989_1/cl/outline
Van der Kolk, B. (2014). The Body Keeps the Score. Penguin Books.
Protesting and The Vicarious Trauma That Can Result From It.

In this day and age we as a nation are facing unprecedented times. From the spread of a new virus which is causing many unforeseen deaths to the protests, riots, and violence taking place due to the alarming death of George Floyd, it appears to be one traumatic event after another. The death of George Floyd has brought out numerous people around the world to stand up for the injustice and racism that took place. Many people questioned why now? Why such a large body of people for George Floyd? He is not the first African American to die in police custody. Frank Leon Roberts, an activist who teaches a course on the Black Lives Matter movement at New York University mentions that there are a number of different factors that can answer those questions.
Floyd’s death was particularly “gruesome, obvious, and clearly recorded on video as opposed to previous instances of police violence where there was partial view of what happened, or the police officer says they made a split-second decision because they feared for their life”. Floyd’s death comes during a pandemic and high unemployment, Roberts states “the US’s 13% unemployment level means that more people than usual can protest and campaign without juggling work commitments”. Floyd’s death also came shortly after the deaths of Ahmaud Arbery and Breonna Taylor and is considered the last straw. Also, the action of the police which forcibly removed peaceful protesters from a square outside of the White House can be considered another reason why many people come out to protest (Cheung, 2020).

George Floyd protests on May 31, 2020
When we look at media outlets during the last three weeks we see protests all over the U.S. both peaceful and violent. The violent protests depict by both photographs and videos a sense of fear, outrage, sadness, and disgust to the viewer. Watching these photographs and videos of real-life violence can cause vicarious trauma for many people both adults and children. Some who may have been personally affected by these experiences in the past and are reliving them again today.
The experience of trauma does not need to be direct to have an impact on us. Just being witness to trauma in this course can be challenging (Rousseau, 2020). Vicarious traumatization has been known to affect mental health providers, first responders, medical professionals, and other professionals who are exposed to trauma daily. Yet, according to the U.S. Veterans Administration, research generally finds an association between watching media coverage of traumatic events and stress symptoms. Research also found that traumatic materials in the media can lead observers to experience anxiety, difficulties in coping, immense fear, and feelings of helplessness, especially in children (USVA, 2020).

Dr. Stephanie Moulton Sarkis, a Tampa-based therapist and expert in the psychological effect of trauma, mentions that “a lot of people are reporting having nightmares about being abused by police right now.” This is proving to be true amongst many therapists. Dr. Sarkis continues to state that during this time she has seen patients that who have been victims of domestic violence and have say that watching footage is bringing up issues relating to when they have been victimized (Seitz, 2020).
These protests, riots, and violence that is taking place are causing vicarious trauma to both citizens and law enforcement officers. According to a study published by the Pew Research Center, more than three-quarters of U.S. law enforcement officers say they are reluctant to use force when necessary, and nearly as many (72%) say they or their colleagues are more reluctant to stop and question people who seem suspicious as a result of increased scrutiny of police stemming from the death of Michael Brown in 2014 (Madhani, 2017). These same effects can be expected from the death of George Floyd. It effects everyone’s day to day lives.
The media is something we can not get away from. News is presented to us through so many platforms like television coverage, social media, the internet, radio, and newspapers. There is no way to eliminate the news and the vicarious trauma it brings. You have to try to come to an understanding that bad things happen in this world and sometimes to specific individuals. Limit yourself to what you view and protect yourselves from the trauma it may bring by identifying any warning signs and talking about your feelings with a professional, friend, or loved one. This can be a start to addressing the symptoms of vicarious trauma.
Reference
Cheung, H. (2020, June 8). George Floyd death: Why US protests are so powerful this time. Retrieved from https://www.bbc.com/news/world-us-canada-52969905
Madhani, A. (2017, Jan. 11).'Ferguson effect': 72% of U.S. cops reluctant to make stops. Retrieved from https://www.usatoday.com/story/news/2017/01/11/ferguson-effect-study-72-us-cops-reluctant-make-stops/96446504/
Rousseau, D. (2020). Module 1: Introduction to Trauma. Retrieved from https://onlinecampus.bu.edu/webapps/blackboard/execute/displayLearningUnit?course_id=_65989_1&content_id=_7783428_1&framesetWrapped=true
Seitz, M. (2020, June 9). The Quiet Trauma of Watching Police Brutality on Our Screens. Retrieved from https://www.vulture.com/2020/06/police-brutality-footage-vicarious-trauma.html
U.S. Department of Veterans Affairs. (2020). Retrieved from https://www.ptsd.va.gov/professional/treat/care/toolkits/provider/workingWithTraumaSurvivors.asp
I HAVE A DREAM

Joe Palczynski: One Failure of the Mental Health System
In March 2000, the Dundalk neighborhood of Baltimore, MD was terrorized by a string of spree murders and subsequently, a fugitive manhunt, hostage situation, and one of the country’s longest one-man standoffs. I lived in Dundalk and was seven years old in March 2000. My memory of those few weeks has remained vivid for twenty years. Something that was once a personal source of confusion and trepidation has become a paradigm for the broken mental health system in this country. Joe Palczynski, Dundalk’s spree killer, is just one of the endless individuals who was failed by the mental health system and went on to live a life plagued by the correctional system.
Despite growing up in a loving household free from abuse, Joe Palczynski’s tendencies suddenly turned violent and unpredictable in his teenage years, just days after a severe head injury. Palczynski’s family immediately took action to have him hospitalized and evaluated. Nevertheless, he was not given sufficient treatment, experiencing years of constant medication changes aimed at treating bipolar disorder, which were never quite successful. Over the next decade, Joe attacked seven teenage girls and found himself in his first standoff situation in Idaho after a string of assault and battery incidents. Despite all of these run-ins with the correctional system, Joe Palczynski’s mental health was never the focus, even though his behavior had a clear origin. Palczynski never received any significant inpatient treatment, counseling, or a consistent medication regimen. His bipolar disorder was never properly treated and, thus, his violent tendencies continued. This culminated in 2000 when Palczynski kidnapped his ex-girlfriend, Tracy, and murdered the three individuals who were attempting to provide her a safe-haven from his violence. Over the next few weeks, his behavior became more unpredictable and dangerous. He held Tracy captive before deciding to run from the police, murdering a pregnant woman and injuring her toddler during a carjacking. He went on to kidnap another individual, forcing them to drive him back to Dundalk, where he ultimately arrived at the home of Tracy’s family. Twenty days after he kidnapped Tracy, Joe took her family hostage in their own home. After four days of this standoff, in which Joe’s only demand was for the police to hand over Tracy, the family escaped by placing sedatives in his food. The Baltimore police ultimately ended this month of terror by shooting Palczynski twenty-seven times. Officers involved described Palczynski as “unpredictable and prone to severe mood swings” saying “he could be docile at times…then his rage would go off the charts” (Apperson, 2000). Joe was repeatedly characterized as having “previous run-ins with the law- many of them driven by mental illness” (Apperson, 2000).
Palczynski, often referred to simply as “a former convict with a history of mental illness,” is tragically not a unique case (Clines, 2000). “At any given time, 3.9 million [Americans with severe mental illness] go untreated…As a result, incarceration has become the norm for those with severe mental illness. Forty percent of them are incarcerated at some point in their lives” (Snook, n.d.). Joe Palczynski suffered from untreated bipolar disorder, believed to have been the result of severe head trauma experienced during an automobile accident as a teenager. Since this onset, Joe spent brief periods in mental health facilities and years in and out of prison, usually due to domestic abuse incidents and other violent behavior. With proper support and treatment, those with serious mental illness are no more violent or dangerous than any other individual; however, untreated “mental illness is associated with increased risk of violent behavior, with most of the evidence [pertaining] to bipolar disorder” (Volavka, 2000). This fact does not excuse violent or criminal behavior, but does provide a clear explanation and solution. Joe Palczynski’s history of undesirable behavior had a clear link to his bipolar disorder. The root cause of his criminal and violent actions- his mental health- was not properly addressed or treated for over a decade, despite a diagnosis and acknowledgment by both law enforcement and mental health professionals. “Individuals with psychiatric diseases…like bipolar disorder are ten times more likely to be in a jail or prison than a hospital” which, in cases like Palczynski’s, leads to spiraling mental illness and escalating criminal behavior (Snook, n.d.). The tragedies and violence that took place in Dundalk in March 2000 seemingly were preventable, if only the mental health system did not fail to provide the treatment Joe Palczynski required.
Apperson, J. (2000). Police reveal tale of terror. The Baltimore Sun. https://www.baltimoresun.com/news/crime/bal-pal14-story.html
Clines, F.X. (2000). Suspect’s death ends siege; hostages are safe. The New York Times. https://www.nytimes.com/2000/03/22/us/suspect-s-death-ends-siege-hostages-are-safe.html
Snook, J. (n.d.). America’s crime problems being fed by a broken mental health system. Treatment Advocacy Center. https://www.treatmentadvocacycenter.org/fixing-the-system/features-and-news/4112-americas-crime-problems-being-fed-by-a-broken-mental-health-system
Volavka, J. (2013). Violence in schizophrenia and bipolar disorder. NCBI. https://www.ncbi.nlm.nih.gov/pubmed/23470603
Sexual Abuse in the Military
When it comes to sexual abuse I always lean towards the military. I have been serving for over 6 years and sexual abuse is something I have seen first had as well as experienced in the military. I have had many soldiers come up to me telling me they needed to talk because something had happened from both genders. Sexual assault over the years has only risen in the military among all branches, the statistics show that the under reporting rate, as well as the reporting rate is rather high. The actual number of reported incidents of sexual assault has also increased in the past two years, up 26% from 4,794 to 6,053(Kime, 2019). Showing that only a third of all cases are reported, most woman don't report because 43% them stated that they had a negative experience when doing so.
Females and males in the military fear reporting because of the shame of what their peers, or commanding officers will say. I know as the years have progressed sexual offenses of any kind are not tolerated and more offenders have been punished. But the stigma of the military is that we are built tough, for any gender it is a very hard topic to come out and say that something of that nature has happened it is almost embarrassing.
Being someone who was once sexually assaulted in the military I honestly didn't want to tell anyone after it happened I was afraid of what people would say. But if it wasn't for my battle buddies they gave me the strength to stand up and say something. It was not a easy task and for the longest time I believed it was my fault, it took over a year before I trusted anyone again. But from it I learn all the right words and actions to take in case it ever happened to any other soldier.
Alcohol plays a major role almost 62% of assaults geared from it, many junior enlisted men and woman are at higher risk for sexual assault. For many people they may not understand why but for the ones who are in or served we understand how hard it is when you start out. It is just like any job you want to put your best foot forward, and your afraid of failure. The same goes in the military you want to show everyone including your family that you can do this, and sometimes you are placed in a situation as a young soldier that you don't know how to get out of. Unfortunately it is still happening to this day with no end in sight.
There are many treatments that help sexual assaulted victims because frankly many of them experience (PTSD) Post Traumatic Stress Disorder, social awkwardness, depression, or suicidal thoughts. It is a hard road for anyone to have to deal with if you do not have the proper support chain to help you get through it. I am blessed to have had that chain, and now am the support for others it is a rather rewarding feeling. Even though it came with terrible circumstances it helped me to understand psychology and respect it so much more.
It is often said that a sexual assaulted victim is victimized twice once by the criminal justice system and the other by the perpetrator(Bartol & Bartol, 2021). Self blame is also very real and one that took me so long to get over, but once I realized that I was not the problem I was able to become a advocate for others in the military for many that is not the case.
Bartol, C. R., & Bartol, A. M. (2021). Criminal behavior: a psychological approach. Boston: Pearson.
Kime, P. (2019, May 2). Despite Efforts, Sexual Assaults Up Nearly 40% in US Military. Retrieved from https://www.military.com/daily-news/2019/05/02/despite-efforts-sexual-assaults-nearly-40-us-military.html
Trauma Related to Drug Abuse
One day while at work I was standing in a lobby when I noticed a woman in her early 30s who was rushing through the door and appeared panicked. As she passed through the lobby she began crying, short of breath and fell to the ground while talking on her cell phone. When she fell I ran over to her to provide assistance in any way I could. I asked her if she was okay and if there was anything that I could do to help her. She looked at me with tears in her eyes and told me that a family member had just overdosed on heroin. At first I was shocked and felt so bad for her and then tried to help her back to her feet and then escort her to her office where I was met by her friends who consoled her and care for her during that awful time for her.
While I understand that addiction is a very complex dilemma to be in and the problems that addiction alone presents can be quite traumatizing. According to the Massachusetts Department of Public Health heroin was listed as the primary drug of abuse in 50.3% of treatment admissions. Heroin is a highly addictive opiate that caused 2,000 overdoses in the state of Massachusetts in 2016. With the drug being so addictive and extremely difficult to break the habit which could be predicated by the fact of trauma that the victim is enduring. Not only is heroin and other opiate usage dangerous, but the circumstances and dangers of that lifestyle are traumatic as well. Addicts are susceptible to perilous situations including homelessness, dangerous environments, dangerous people, and some even resort to crime to pay for their habit.
The toll that living on the streets has shown to be traumatic for the body and mind as well. According to the Boston University School of Public Health homeless individuals are more susceptible to premature deaths that can be attributed to poor sleep, lacking hygiene, and an abundance of other complications that come from living out in the elements. With many addicts resorting to living on the streets there becomes only a few ways to acquire money for their addiction.
One way of sustaining their habit is prostitution. In one article by (Silbert, Pines, & Lynch, 1982) it was estimated that between 40-85 percent of prostitutes were suffering from some form of addiction. As stated before addicts are exposed to many dangerous and traumatic situations. Using prostitution to fuel the source of their addiction can lead to many emotional, psychological, and physical traumatic events. Having to live with what they have resorted to do for their addiction can be troubling, and depressing which drives them to feel the euphoric numbness of the opiate. One study by (Farley, 2018) noted that women who participate in prostitution have a 99% greater risk for physical violence than any other highly dangerous job.
Though the affects of drugs are severe and life threatening, we must also address traumatic events that can arise as a byproduct of addiction. Risk factors involved with drug addiction are very dangerous and present a complex and difficult lifestyle. Effects of these epidemics are not centralized to the user, but as stated above can be traumatic for family and friends as well.
Farley, M. (2018). Risks of Prostitution: When the Person Is the Product. Journal of the Association for Consumer Research, 3(1), 97–108. doi: 10.1086/695670
MA Heroin Treatment Stats. (n.d.). Retrieved from https://adcare.com/massachusetts/heroin/
McInnes, K. (n.d.). Homelessness, Its Consequences, and Its Causes: SPH: Boston University. Retrieved from https://www.bu.edu/sph/2016/02/28/homelessness-its-consequences-and-its-causes/
Silbert, M. H., Pines, A. M., & Lynch, T. (1982). Substance Abuse and Prostitution. Journal of Psychoactive Drugs, 14(3), 193–197. doi: 10.1080/02791072.1982.10471928