CJ 720 Trauma & Crisis Intervention Blog
Healthy Mind During Pandemic
The past 6 months have been a roller coaster between the death of Kobe Bryant which impacted me greatly since I grew up watching him. To the start of COVID-19 and being in quarantine for a little over 3 months. Now many would say, how do you keep your mind straight and not lose your mind while working from home all day to then logging into class on the same laptop you were just working on. My answer may vary from yours, it all depends on how you deal with stress. My escape from it is just getting into my car and aimlessly driving around town. Yours might be exercising or reading a book.
There are two components of self care and they are physical and mental. The Mayo Clinic Health System provides tips in how to practice physical healthy," eating healthy, sleep 7-8 hours a night, stretch, spend time outside." But the one that take more strength and determination in my opinion is mental health. They Mayo Clinic recommends "set and maintain a routine at home, focus on things you can control, maintain social connections with your loved ones" The one that sticks out the most is focusing on the things you can control. Many people love to be in control of their lives but a lot of what happens is out of our hands and it is important to not get lost in trying to figure out why things happen but instead learning how to control the things that are able to be tamed.
But I think it is important to highlight the importance the individuals who have been on the front lines during this pandemic who have experienced immense amounts of stress with little time to deal with it. According to the American Psychiatric Nurses Association a way to manage stress is to exercise self-compassion "almost everyone impacted by an emergency will experience psychological distress"... "It is easy to play up the importance of self-care to our patients while downplaying it to ourselves...give yourself permission to schedule even a few moments for self-care each day." This reminds of what Van Der Kolk states in The Body Keeps the Score "When chronically stressed, tension builds up within the body." ( pg.266) which is why nurses and people who work in public health should definitely not feel guilty for wanting some alone time to keep a healthy mind.
References:
Managing Stress & Self-Care During COVID-19: Information for Nurses. (n.d.). Retrieved June 22, 2020, from https://www.apna.org/m/pages.cfm?pageID=6685
Self-care tips during the COVID-19 pandemic. (n.d.). Retrieved June 22, 2020, from https://www.mayoclinichealthsystem.org/hometown-health/speaking-of-health/self-care-tips-during-the-covid-19-pandemic
Self-Care and Trauma
Many people do not realize the importance of self-care as it relates to trauma. van der Kolk states that, “Nobody can ‘treat’ a war, or abuse, rape, molestation, or any other horrendous event, for that matter; what has happened cannot be undone, but what can be dealt with are the imprints of the trauma on the body, mind, and soul” (2015, p. 205).
The effects that trauma has on our bodies can be mentally, emotionally and physically debilitating. It can cause a crushing sensation in your chest that you may label as anxiety or depression; a fear of losing control; always being on alert for danger or rejection; self-loathing; nightmares and flashbacks; a fog that keeps you from staying on task and from fully engaging in what you are doing; being unable to fully open your heart to another human being (van der Kolk, 2015, p. 205).
Trauma affects our entire being and affects how we relate and connect to others. When one suffers the effects of trauma, it is imperative to deal with the imprints it has left on our bodies, minds and souls to live a happy and healthy life.
Van der Kolk stated that, “the fundamental issue in resolving traumatic stress is to restore the proper balance between the rational and emotional brains, so that you can feel in charge of how you responds and how you conduct your life” (2015, p. 207). There are many methods one can use to deal with the effects of trauma.
Cognitive Behavioral Therapy (CBT) relies on the idea “that when patients are repeatedly exposed to the stimulus without bad things actually happening, they gradually will become less upset; the bad memories will have become associated with ’corrective’ information of being safe (van der Kolk, 2015, p. 222-223). It was originally used to treat phobias but has often been used to treat PTSD.
Van der Kolk explains that, “we may think we can control our grief, our terror, or our shame by remaining silent, but naming offers the possibility of a different kind of control” (2015, p. 234). Communication with one’s self is key to awareness. This communication can be writing, art, talking, music or dancing. Talking with yourself and sharing it with others makes one feel like a member of society again. Once a person begins to share, they are able to open themselves up to loved ones and begin to mend and strengthen those relationships as well.
Eye movement desensitization and reprocessing (EMDR) is yet another effective method to deal with trauma. In EMDR, one goes back to the trauma and brings to mind the images of it, the sounds and thoughts that went along with it. Then, they follow the therapist’s finger as it is moved slowly back and forth about twelve inches from the right eye, stopping every few minutes to take a deep breath and pay attention to what is on their mind; and repeating the process numerous times (van der Kolk, 2015, p. 251).
“One of the ways the memory of helplessness is stored is as muscle tension or feelings of disintegration in the affected body areas: head, back and limbs in accident victims, vagina and rectum in victims of sexual abuse” (van der Kolk, 2015, p. 267). Yoga is an especially effective method to combat the muscle tension and feelings of disintegration. Yoga is a series of movements that is posture-based. It is also a form of meditation to relax and reconnect with oneself. It allows the parasympathetic nervous system work in tandem with the sympathetic nervous system to balance the body.
Trauma can be stressful, but it doesn’t have to stay that way. The first step to recovery is realizing there is trauma that needs to be dealt with and the want to deal with it. As van der Kolk notes, “silence about trauma also leads to death – the death of the soul (2015, p.234)."
Van der Kolk, B. A. (2015). The Body Keeps the Score: Brain, Mind, and Body in the Healing of Trauma. New York: Penguin Books.
Modernization or Traumatic
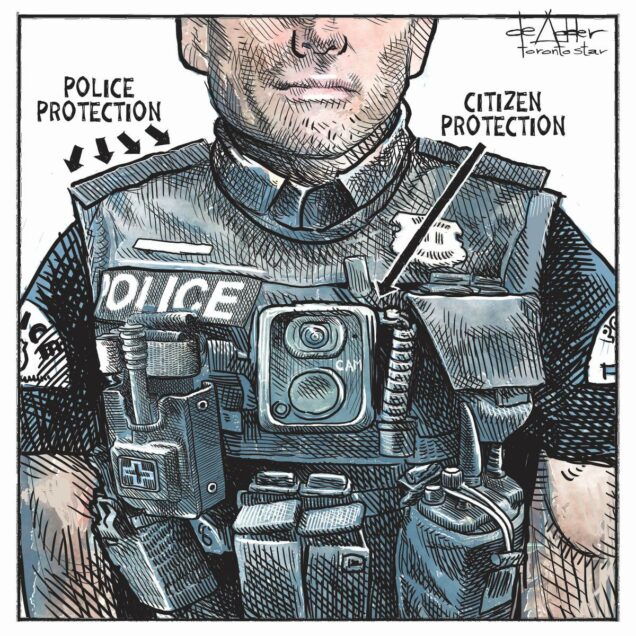
The image of the modern police officer has evolved over the years into a more modern and tactical appearance. The days of the thick wool or cotton long sleeve shirts, pants, and ties, garrison style hats, a leather duty belt with only a firearm and one set of handcuffs are a thing of the past. The look that many citizens in the United States have come accustom to over the years has been replaced with a more militaristic and practical approach to policing. This new image might be more realistic to the daily duties of law enforcement and appealing to the officer wearing the uniform, but how is it perceived by the public? Richard Johnson (2001) states police uniforms have a profound psychological impact on the public, and slight alterations to what the public is accustom to, may change the public’s perception of the police (Johnson, R., 2001, P27). A uniform change that is more comfortable, compatible, and reduces stress upon the officers who must don them, could inadvertently be displacing that stress onto the citizens they serve. Will society be able to adapt to this style of police uniform or will it create a greater divide among law enforcement and the community? The physical and mental health benefits of this modernized uniform could be a step in the right direction, taking care of those who care for us.
The traditional wool class A style uniforms that was previously predominately worn by law enforcement has become impractical for modernized policing. Today’s police are expected and or required to carry a greater number of tools on their person in preparation for every possible outcome. A firearm, extra magazines, hand cuffs, a flashlight, pepper spray, taser, baton, radio, body cameras, and tourniquets are a part of today’s standard policing attire. “Some police leaders dislike the tactical appearance of the loadbearing vests while others applaud their efficiency and potential for increasing comfort while decreasing injuries due to back strain” (Stockton, 2016, P.24). The demand for added equipment has caused greater amounts of weight to be placed on officer’s duty belts resulting in injuries. External carrier uniform vests take that added weight off of the officer’s duty belt and distributes it on the vest. This weight reduction from the duty belt has been a relief for officer’s who suffer from back related injury or pain. Having worn both styles of uniforms myself, I can attest to the added comfort and versatility that these external carriers provide. The change to the external carrier style uniform vests has provided an improvement in the health and wellbeing of officers particularly when stuck in the uniform for long hours. Police officers and some administrators are in favor of the modernization of the police uniform, but does public perception take precedent to the officer wellbeing?
If the modern uniform appears too militaristic in the eyes of the public, what consequences will result? Police agency around the country have focused great efforts in developing positive relationship building strategies within their communities. How does a police agency portray the added benefits both physical and mental these uniforms provide for their officer’s? How do police agencies help mitigate the added stress and fears of militarization of the police that these new styles of uniform create? With the current tensions building between police and citizens across the country, could the implementation of these new militaristic style uniforms have contributed to the unraveling relationships between the police and the communities they serve?
Michael Carrasquillo
Reference:
Johnson, R. (2001). The Psychological Influence of The Police Uniform. FBI Law Enforcement Bulletin. 27-32.
Stockton, D. (2016). What Every Police Leader Should Know About Body Armor. Tactical Response; Vol. 14. 22-25.
Yoga as Trauma Treatment for Children
Though difficult to know exactly how many cases of child abuse and neglect there are every year in the United States, about 3 million reports are made to Child Protective Services that represent 5 million children. Even those high numbers are thought to be underestimates because when adults are asked about childhood abuse or neglect, 30% report physical abuse in childhood, 20% report sexual abuse in childhood, and 15% reports some type of psychological abuse (Trauma & Dissociation in Children, 2007). And these numbers just continue to go up. In 2018, 4.3 million cases were reported to CPS effecting 7.8 million children (U.S. Department of Health & Human Services, Administration for Children and Families, Administration on Children, Youth and Families, Children’s Bureau, 2018). Either more abuse is occurring to children (along with more under-reporting) or there is no drastic increase at all, yet more of those children who did not report are reporting or CPS is being afforded more resources to handle more intake. I would like to think it is the ladder answer, but we will never truly know. Child abuse and trauma can be hard to detect and/or prove and is grossly under-reported. As Dr. Van der Kolk said, “We know that child abuse and neglect is the single largest public health issue facing our nation, the most expensive and devastating (Trauma & Dissociation in Children, 2007).
If this problem has been and still is this extensive, why is there not more diligent coverage on it in the media to raise awareness to the masses and a more extensive push for programs and procedures within daycare, schools, and the medical field? There are most certainly some great advocates and programs in place nation-wide, like the CDC and what they support on a yearly basis. The CDC works extensively to promote communities, practitioners, and teachers continued knowledge on the topic and supports prevention of adverse childhood experiences (ACEs) across the nation. They facilitate many states in collecting ACE-specific data that aids in future resource targeting and facilitate releasing evidence-based strategies for the consumption and use by local health departments, schools, and communities (CDC, 2019).
Seeing that childhood trauma and abuse does not seem to be decreasing and the under-reporting is still prevalent, I think it is dyer that this nation put into place more efforts to detecting and the treatment of trauma and abuse with children. A treatment and potential stimulation for more disclosures of trauma or abuse is yoga. It may sound rather silly at first but when one reads up on the positive outcomes of yoga on adults and children who have experienced extensive trauma either as an adult or as far back as childhood, it is hard to find a reason not to support the idea. There is limited empirical data on the positive effects yoga has on traumatized children, but one great example was the study conducted on children in Haiti who survived an earthquake and were ultimately left orphaned. Many of these children lost one or two parents and experienced hunger and violence. They were given yoga for 8 weeks, consisting of breathing techniques, postures, and meditation, with positive results: the children who received yoga saw reductions in trauma-related symptoms (Culver & Whetten & Boyd & O’Donnell, 2015).
Yoga is a program that typically consists of a combination of breath practices, stretches or postures, and meditation. Bessel Van der Kolk who wrote the book The Body Keeps the Score: Brain, Mind, and Body in the Healing of Trauma was a huge advocate for yoga as a treatment for trauma. He treated many, many patients who he had participate in routine yoga – specifically focusing on breath and postures to become more in tune with themselves– and many of these patients, as a result of yoga, were able to come to terms with what traumatized them and the realization that they were not at fault. He also conducted actual studies on the physiological affects yoga had on trauma patients. He found that yoga significantly improved arousal problems in PTSD patients and drastically improved their relationships to their own bodies (2015). This is huge in the realm of trauma because being able to recognize how and why you react to certain triggers allows you to begin the healing process and control how you react moving forward. Since trauma effects one’s entire nervous system, it is critical for treatment to engage the entire organism, body, mind, and brain, which yoga can do (Van der Kolk, 2015).
Yoga is something that could be implemented in daycare and schools at a relatively low cost. The potential results that teaching yoga to children could accomplish would be well worth any of the resources it took to mandate it. Now, there would most likely be a minimum age requirement since incredibly young children would not have the attention span to participate. Through more thorough research that could be addressed. The Haiti study mentioned herein started with a 7-year age group, so that could be a starting point. I just see the opportunity for this small step to bring children more in tune with their bodies and minds and therefore could lead to them to reporting more often then what we are seeing now.
References:
(2007). Trauma & Dissociation in Children [Video file]. Cavalcade Productions. Retrieved May 31, 2020, from Kanopy.
Centers for Disease Control and Prevention. (2019). Identifying, Preventing, and Treating Childhood Trauma. Retrieved from https://www.cdc.gov/washington/testimony/2019/t20190711.htm.
Kathryn A. Culver, Kathryn Whetten, David L. Boyd, and Karen O'Donnell.The Journal of Alternative and Complementary Medicine.Sep 2015.539-545.http://doi.org.ezproxy.bu.edu/10.1089/acm.2015.0017
U.S. Department of Health & Human Services, Administration for Children and Families, Administration on Children, Youth and Families, Children’s Bureau. (2020). Child Maltreatment 2018. Available from https://www.acf.hhs.gov/cb/research-data-technology /statistics-research/child-maltreatment.
Van der Kolk, B., (2015). The Body Keeps the Score, Brain, Mind, and Body in the Healing of Trauma. Penguin Books.
The Horror of the Holocaust
While the Holocaust may be decades in the past, the trauma and pain it brought about are still very real even today. Back in 2018 I got to travel to Israel through a spring break program at my university. As part of this trip we visited many historical and religious sites across the country, but by far the most memorable was the Holocaust museum. Our tour guide, an Israeli Jew walked us to the gates of the museum, but declined to go with us. For him the museum was a reminder of the family members he had lost during the Holocaust, and was too painful.
One of the parts of that museum that will forever be engrained into my mind is the memorial to the children lost during the Holocaust. You enter a dark tunnel, with soft somber music echoing throughout. There are hundreds of mirrors set to reflect the light of a single candle millions of times around you. Each reflection of the candle represented the life of a child whos flame was extinguished far too soon during the genocide. Many of us including myself left the tunnel in tears. The atrocities committed during the Holocaust were unspeakable, millions of innocent people killed for their beliefs.
The trauma inflicted by the Nazis continued even after their reign of power came to and end. After the war there were countless children who had lost their families or experienced trauma. As we learned in unit 2 adverse childhood experiences can lead to problems later in life such as depression and other health issues (Rosseau 2020). The number of children who experienced trauma throughout the holocaust and had such issues later in life is incalculable. Wiesel writes about being herded into railroad cars, threatened with death, starved and dehydrated being sent off to camps. Some families were separated, and would never see each-other again (Night 2006). These types of experiences would severely traumatize anyone. Even after the terror stopped, the damage was still continuing. In studies conducted on Holocaust survivors years later 45-55% were found to be suffering from PTSD, and many ranked the Holocaust as the most significant stressor in their lives even decades later (Barak 2000). While the genocide may have ended decades ago, its effects are still felt today. Trauma never really goes away, as the memories will always be there.
References:
Barak, Y., & Szor, H. (2000). Lifelong posttraumatic stress disorder: evidence from aging Holocaust survivors. Dialogues in clinical neuroscience, 2(1), 57–62.
Rousseau, D. (2020). Module 2. Retrieved from https://onlinecampus.bu.edu/bbcswebdav/pid-7783368-dt-content-rid-37966231_1/courses/20sum1metcj720so1/course/module2/allpages.htm
Wiesel, E., & Wiesel, M. (2006). Night. New York, NY: Hill and Wang.
A Double Pandemic: Covid-19 and Domestic Violence
A Double Pandemic: Covid-19 and Domestic Violence
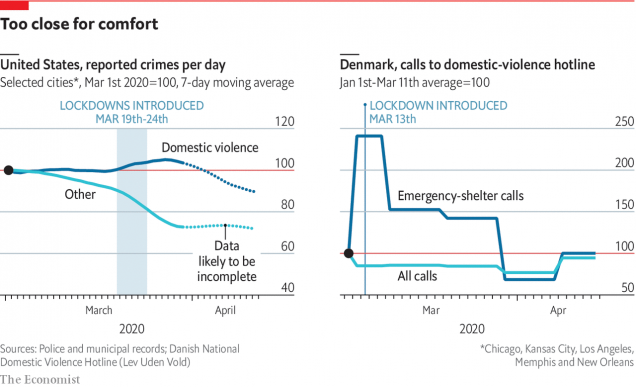
COVID-19 has impacted the world greatly with strict restrictions on stay at home orders, especially throughout the United States. While the shelter in place has been shown to help decrease the number in cases for the coronavirus, domestic violence cases seem to be on the rise. In a home with domestic violence, it is crucial for the victim to be away from the home as much as possible to avoid any altercations with the perpetrator. “Many victims find themselves isolated in violent homes, without access to resources or friend and family networks” (ICISF 2020). The heightened increase in domestic violence could be for several reasons. For the victims, now that shelter in place has been enacted, there is a higher chance for them to not be able to seek the help and resources that they need. “One out of three women in the world experience physical or sexual violence in their lifetime, according to the World Health Organization, making it the most widespread but among the least reported human rights abuses” (Godin, 2020).
During these lockdown restrictions, victims are more exposed to abuse in their households. These are stressful times and the known financial circumstances especially, can cause a lot of tension. More often than not, perpetrators take out their anger and stress on the victims. In France has indicated a 30 % increase in domestic violence reports, Brazil estimates domestic violence reports have jumped 40–50 %, and Italy has also indicated reports of domestic violence are on the rise (Campbell 2020). It is crucial, now more than ever, that welfare checks are being done.
References
Bettinger-Lopez, C. (2020, May 13). A Double Pandemic: Domestic Violence in the Age of COVID-19. Retrieved June 22, 2020, from https://www.cfr.org/in-brief/double-pandemic-domestic-violence-age-covid-19
Campbell A. M. (2020). An increasing risk of family violence during the Covid-19 pandemic: Strengthening community collaborations to save lives. Forensic Science International: Reports, 2, 100089. https://doi.org/10.1016/j.fsir.2020.100089
Godin, M. (2020, March 18). How Coronavirus Is Affecting Victims of Domestic Violence. Retrieved June 19, 2020, from https://time.com/5803887/coronavirus-domestic-violence-victims/
Trauma Associated with Female Imprisonment
Within the United States more than 200,00 women are imprisoned, most of which are for non-violent crimes. As opposed to their male counterparts, female incarceration generally exists due to illegal actions associated with petty crime either stemming from drug use, or a need to provide for their children. The United States has the highest number of incarcerated women worldwide and much of this is a result of trauma related experiences within their lives prior to incarceration.
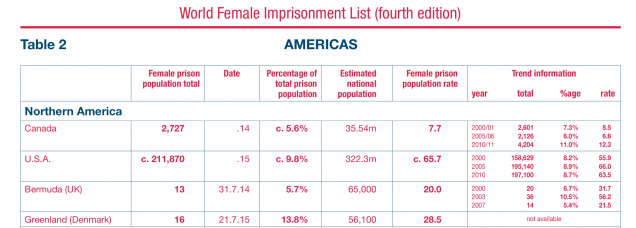
Unfortunately our prison system is based on a male model and doesn’t take into consideration the sensitive nature of women who have been traumatized. Many women have experienced long term physical or sexual abuse and therefore are further subjected within the prison system. “Imprisonment itself can have serious mental health effects, particularly for women with children and a history of victimization. The prison experience is not an isolated encounter. Rather, it may serve to exacerbate women's trauma while, equally, the trauma may exacerbate the prison experience for women.” (Moloney, Bergh, Moller) Trauma and prison are many times intertwined as women enter incarceration with a multitude of past trauma and do not receive trauma related care within the system, which not only exacerbates their difficulties but leads to repeat offenses. Oftentimes women are held for longer periods of time within their local jails as female offenders generally have less income than males and are unable to post bail or seek the legal representation they may need. The notable income disparity between men and women within the criminal justice system further exemplifies the need for gender specific approaches.
Youth offenders also make up a large population of those within the prison system, if these young women are not assisted with their healing they are likely to reoffend and spend many years of their lives within the criminal justice system. “A gender-responsive approach comprehensively addresses the unique and specific needs of girls, creates an environment that reflects the realities of girls’ lives, and acknowledges their unique developmental experiences and pathways to problem behaviors. “ (Harris, Fitton) Programs that help promote healing, self esteem, financial independence, and control over ones own body can help women both young and old develop tools to heal and move forward with better coping mechanisms.

We as a society need to take into consideration the role that trauma plays in incarceration rates. If we hope to make the public safer, we must implement ways to help the incarcerated process and attempt to recover from their trauma. Simply locking a woman up for prostitution or drug use, doesn’t confront the underlying issues as to why they are involved in illegal activity. We need a more comprehensive analysis of the data associated with women who are incarcerated, the way in which they are held Prison vs. Local Jail, the reasons for their crimes, and how they are being treated within the system. Women inmates have different needs than their male counterparts and our criminal justice system needs to implement more gender responsive approaches to help women combat their trauma while incarcerated.
Sources:
R. Walmsley, (2006) World female imprisonment list. International Centre for Prison Studies, London. Sourced From: http://fileserver.idpc.net/library/world_female_prison_4th_edn_v4_web.pdf
K.P. Moloney,B.J. van den Bergh,L.F. Moller (2009) Women in prison: The central issues of gender characteristics and trauma history. Published by Elsevier.
Danielle Arlanda Harris, PhD 1, (2010) Yoga Therapy in Practice The Art of Yoga Project: A Gender-Responsive Yoga and Creative Arts Curriculum for Girls in the California Juvenile Justice System Published in: INTERNATIONAL JOURNAL OF YOGA THERAPY
Self-Care During a Pandemic
Long-term activation of the body’s fight or flight stress response can lead to health issues. The body’s stress hormone, cortisol, is beneficial in small doses, but can become detrimental when levels remain elevated (Mayo Clinic, 2019). During the coronavirus pandemic, many of us are experiencing a lost sense of “agency” – the feeling of being in control of your life (van der Kolk, p. 95). This chronic stress of feeling out of control and on-guard can lead to autoimmune disorders, skeletal and muscular problems, and issues with emotional regulation if left untreated (van der Kolk, p. 86). Less severe consequences include digestive issues, headaches, and sleep issues (Mayo Clinic, 2019). To overcome the effects of chronic stress, we must find a way to calm the body’s fight or flight response. Remaining calm and focused when introduced to stressful situations in our daily lives is imperative for our health (van der Kolk, p. 203).
Take action! Regain that sense of agency. Making an active effort to deal with traumatic or stressful situations is beneficial to your health, so put your adrenaline to good use (van der Kolk, p. 217). If the coronavirus has you feeling on edge, follow a YouTube tutorial and make masks for you and your loved ones. If you have all the supplies you need, check in on a neighbor and see if they need anything. Do what you can to help feel in control.
Get physical! We face disruptive physical reactions to stress (van der Kolk, p. 204). When chronically stressed, tension builds up within the body (van der Kolk, p. 266). Yoga is proven to have incredible results for calming the body and undoing these harmful reactions. Yoga focuses on regulating breath – regulated breathing helps create a steady heart rate, which contributes to overall health and well-being. This helps us stay calm and react in a more composed manner when faced with daily stressors (van der Kolk, p. 266). If yoga is not for you, even just going for a walk around your neighborhood daily can help to clear your mind and keep your physical body healthy.
References:
Mayo Clinic. (2019, March 19). Chronic stress puts your health at risk. https://www.mayoclinic.org/healthy-lifestyle/stress-management/in-depth/stress/art-20046037
van der Kolk, B. A. (2015). The Body Keeps the Score: Brain, Mind, and Body in the Healing of Trauma. New York: Penguin Books.
Police Brutality has traumatized us all
On May 25, 2020 Minneapolis Police received a call of a possible fraud that had just occurred at a local business. Officers arrived on scene, and arrested George Floyd, a 46 year old black man, for providing counterfeit money to buy cigarettes. Mr. Floyd was passively resisting which led to a brief struggle between him and the four officers on site. Once on the ground, Officer Derek Chauvin, was on top of Mr. Floyd’s neck for 8 minutes and 46 seconds. Causing the victim George Floyd to die from asphyxiation. Chaos ensued afterwards. Protests across the world began and are still ongoing. Demands for justice, police reforms, defunding of departments, and even abolishment of police can be heard around the world. The one thing that’s not talked about is because of Derek Chauvin’s action, we have all been traumatized by police brutality.
For example, in Atlanta while protests were happening, six Atlanta Police Officers were arrested, 5 of them for aggravated assault, for their use of tasers of two black people. The District Attorney of Fulton County, Paul Howard, came out in a press conference and stated that “Under Georgia Law a taser is considered a deadly weapon.” A week later, this statement was put to the test unfortunately, as Atlanta PD officers were involved in the shooting and killing of Rayshard Brooks. APD was called on scene for a man passed out in the middle of a Wendy’s drive thru. When they arrived on scene, officers had Mr. Brooks step out of the vehicle and conducted a field sobriety test. After the test was over, a breathalyzer was used to determine Mr. Brooks intoxicated level. He blew a .108 percent, which is higher than the legal limit of .08. Officers began to arrest Mr. Brooks for Driving Under the Influence (DUI), when he began to resist arrest. He assaulted both officers, he was tased, to not avail, and he grabbed the officer’s taser and began to take off running. A short foot pursuit ensued, where Mr. Brooks turned around and deployed the taser to the officers. Fearing for their lives, because according to the Fulton County DA “Under Georgia Law a taser is considered a deadly weapon”, one officer drew his service weapon and shot Mr. Brooks 3 times, striking him twice, ultimately leading to his death. Within a week, chaos had occurred again. The officer who fired his weapon was fired, by the mayor because the chief of police refused to do as such. The second officer was placed on administrative leave. Both officers were charged in the death of Rayshard Brook, because according to the Fulton County DA, “tasers are non-lethal weapons.” This is I say we’ve all been traumatized.
Just a week ago tasers were lethal when used on citizens, but when a citizen attempts to use it on an officer, it is no longer lethal? Where is the fairness and justice this country is all about? I believe the DA felt tremendous amount of pressure to bring chargers to the officers, even though the chargers do not fit the crime. Mr. Brooks was out on parole for his previous conviction of, False Imprisonment, Simple Battery/Family, Battery Simple and Felony Cruelty/Cruelty to Children. This was not an innocent man that had made the mistake of drinking and driving. This was a man that was out on parole, was out drinking and driving, luckily did not cause an accident, and resisted arrest because he knew if arrested, he would be going back to prison. Because of the movements around the world, these officers were charged for a crime they did not commit. They followed department’s procedures and policies, and acted accordingly. But due to the world wanting to see the police burn down, the DA is out to make an example of them when is it not warranted.
After the DA announcing of the charges, Atlanta PD officers began to call out of work sick, and what is known as the “blue flu”. Officers fearing for their lives, have not shown up to work at the night shifts in Atlanta. About 30 or so officers called out, because they are scared that they’ll receive a call, follow procedure and still be prosecuted for it. They’re afraid that the department, the city, and the justice system is failing them for doing the right thing. Police brutality traumatized us all to the point where police officers are afraid to their jobs. Across the country officers are leaving the force because they don’t want to be in a situation where following procedure gets them arrested and sentenced. They are scared, and they cannot be blamed for it. Unfortunately, the citizens will feel the backlash of these actions. Less officers will be available to respond to 911 calls, meaning higher chances of criminals getting away with committing crimes.
Police officers aren’t the only ones traumatized by police brutality, citizens, especially those of colors, are more than ever afraid of police. This became very real, and sadly true when I saw a specific video. In this video, out Trumbull Connecticut, there’s a young teenager, dribbling a basketball outside his house. The kid is by himself, he’s dribbling minding his own business. When suddenly, he stops and begins to hide by a white SUV that is parked on the driveway. At this point we can’t see why he is hiding. After a few more seconds, a police cruiser comes into the frame, and just drives on by. The officer appeared to be just cruising around. However, the kid was hiding from the officer. This was very heartbreaking, a young boy playing basketball has to hide from the police because of the actions of other officers. He has to hide because he is scared that he will be attacked or worst, if the cop sees him.
It is beyond saddening seeing this around the country. People are afraid of the police, and the police are afraid to do their job. This is because the actions of the bad officers that unfortunately exists in our country. Officers, the good ones, the ones out there on the streets trying to make positive change, all their hard work. All of their struggles, and fights to make the streets a lot of safer, and to build a strong community relationship, everything is tinted by the action of others. This career, this passion that some of us have, we’re judged not by we do, but by others do. This is the only career, where an officer, no, a criminal disguised as an officer in Minnesota can kill an innocent victim because he has no heart and soul, and have the backslash of it be felt by an officer in Massachusetts, that had nothing to do with the situation. Now more than ever a strong community policing needs to put in place, departments across the country need to start healing that bond, and making it stronger with the community. Showing them they’re support in their movement and passion, but at the same time demonstrating that they are out to do the good work.
References
Hill, E., Tiefenthaler, A., Triebert, C., Jordan, D., Willis, H., & Stein, R. (2020, May 31). How George Floyd Was Killed in Police Custody. The New York Times. Retrieved June 21, 2020, from https://www.nytimes.com/2020/05/31/us/george-floyd-investigation.html
Waldrop, T., Gallagher, D., & Kirkland, P. (2020, June 4). 6 Atlanta police officers booked on charges after alleged use of excessive force during protest. CNN. Retrieved June 21, 2020, from https://www.cnn.com/2020/06/03/us/atlanta-police-booked-felony-charges-protest/index.html.
Young, R., Levenson, E., Almasy, S., & Maxouris, C. (2020, June 17). Ex-Atlanta Police officer who killed Rayshard Brooks charged with felony murder. CNN. Retrieved June 21, 2020, from https://www.cnn.com/2020/06/17/us/rayshard-brooks-atlanta-shooting-wednesday/index.html.
O'Leary, F. (2020, June 17). Did Rayshard Brooks have a criminal history and was he on probation the night he was shot? The U.S. Sun. Retrieved June 21, 2020, from https://www.the-sun.com/news/998770/rayshard-brooks-criminal-history-probation-atlanta/.
Spocchia, G. (2020, June 17). Ten-year-old boy seen hiding from passing police car ‘because they killed George Floyd'. Independent. Retrieved June 21, 2020, from https://www.independent.co.uk/news/world/americas/george-floyd-killing-boy-hiding-police-car-footage-a9569986.html.
Ambiguous Loss
"I intentionally hold the opposing ideas of absence and presence, because I have learned that most relationships are indeed both."
- Pauline Boss, Ph.D.
In the last 50 years, our understanding of the spectrum that grief encompasses has grown immensely. Yet, grief is still wildly misunderstood and underrecognized in our culture. For some, we grant specific labels to identify their grief in a concrete way: a widow, bereaved parent, or a sibling of a fallen soldier. Almost always, these labels tell us that someone’s grief is valid because they are grieving the death of a loved one. These labels tell us: “her husband died, you are free to bring a casserole to her door,” or “his sister died in the war, you may write on his Facebook wall that you are thinking about him on Memorial Day.” We know what to do with concrete loss. We know the social rules and instructions that come with each label that we have attached to concrete grievers.
But for many, loss and grief reaches beyond the concrete labels; beyond the dead; beyond a final resolution. This type of grief is now known as “ambiguous loss.” This type of loss carries great unknowns and no societal instructions in how to react. I was first hit with ambiguous loss when we had to hand back the baby girl who was literally minutes away from being our legally adopted daughter. Not only did we have a failed adoption, but she went to a family member that knowingly abused her and did not support any continued relationship with our family.
This little one will have no memory of being a part of our family, even though (in our eyes) she is nothing short of being our first daughter - the one who turned me into a mother and my husband into a father. Suddenly, my husband and I were caught in the thick of grieving our child who was still living. We grieved her future, tucked away her nursery, told our parents that they were no longer grandparents, and were completely heartbroken. We mourned the loss of a future with the daughter we would never see again. But, she is still alive. There was no funeral, memorial, title, or label that told others how they could react.
The first thing I did was turn to my community to look for support groups. But of course, there are no support groups for “childless parents with living children.” When people asked me if I had any children the answer “not yet!” seemed fake; it seemed to deny our baby girl’s existence. But the answer “yes,” did not work either. Yet, no one cutting your hair or chatting at the farmers’ market wants a detailed story of how your daughter is no longer your daughter. Not having anywhere to turn for support became extremely isolating. It made me feel as though my loss must not be real and that I needed to simply “be grateful” it was just a failed adoption, rather than something worse.
This kind of thinking took my mourning to a level of isolated depression. It was not until I started seeing a grief counselor that she explained to me there are many different types of losses. She introduced to me the term “ambiguous loss,” which is “grief without a resolution or without a death” (Boss, 2020). From there, I learned that there has actually been great amounts of research on the stinging pain of ambiguous loss. She shared with me that while we like “black and white” losses in our culture, most loss is ambiguous. When I began opening my world up to honoring all types of loss, no matter how unresolved my loss still was, I was able to truly begin healing.
So what do we call the loss of a father who is mourning his brain dead child that is still right in front of him? How do we honor the grief of the refugee in our neighborhood who does not know if their family members are still alive? At what point do we reach out to the mother of a child on death row? How do we recognize the loss of our friend whose parents are alive, but are lost deep within in the affects of dementia? Are we supposed to give flowers to the childless neighbor who has suffered 8 miscarriages? The way we recognize and make room for grief in our culture either helps heal or further traumatizes those who are suffering from ambiguous loss.
Psychologist Abby Maslin shares that “ambiguous loss is learning to live with a lot of uncertainty, never knowing if you will get an end result” (“Grieving the Living,” 2020). Because of this uncertainty, Dr. Boss explains that this type of loss often “erodes our sense of mastery and destroys our belief in the world as a fair, orderly, and manageable place” (Boss, 2020). Most people facing this kind of loss have faced the “well, at least the person you love is...” comments. This kind of attitude only further isolates the ambiguous griever.
Those who are suffering from ambiguous loss still work through the same grief cycle as someone who is suffering from concrete loss (“Ambiguous Grief,” 2020). Today, research suggests that the methods we use to remember the dead can be used in the same ways to honor ambiguous loss (Hugstad, 2017). Experts also share that “remembering [that] the present does not override the past” is a powerful way to honor what is missing in ambiguous grieving (“Ambiguous Grief,” 2020). While it is our immediate desire to make someone else’s loss concrete, we must understand that this is simply impossible with unresolved grief. Dr. Boss explains that “while such losses cannot be resolved, they can be acknowledged and supported” by professionals, family members, friends, and communities (Boss, 2020). When we make room for these types of losses we are offering our permission to connect with another’s pain rather than push them further into the darkness. Light and healing cannot enter where there is no room.
So how about we bring the casseroles, drop off the flowers, and bake the cookies for those that we see with unresolved grief? Will you look your ambiguously-grieving friend in the eyes and say “no matter how messy your pain is today, I am here for you?” How will you decide to recognize that all grief looks different even if there is painfully no resolution in sight? Will you wait for a concrete label to tell you how to support the grieving or will you pave your own path to honor whatever loss comes your way? One thing is certain when it comes to ambiguous losses: they are not going anywhere. Because of this, it is up to us to make room for this type of unique, yet common grief. Only then can true healing begin.
Sources:
Ambiguous grief: Grieving someone who is still alive. (2020). Retrieved from https://whatsyourgrief.com/ambiguous-grief-grieving-someone-who-is-still-alive/
Boss, P. (2020). About Ambiguous Loss. Retrieved June 20, 2020, from https://www.ambiguousloss.com/about/
Grieving The Loss Of A Person Still Living. (2020). Retrieved from https://americanbrainsociety.org/grieving-the-loss-of-a-person-still-living/
Hugstad, K. (2017, November 30). Grieving the living: When your “lost” loved one is still alive.
Retrieved from https://whatsyourgrief.com/ambiguous-grief-grieving-someone-who-is-still-alive/
By Sadie Jenks - CJ 720 2020 Summer 1