CJ 720 Trauma & Crisis Intervention Blog
Treating vs. Curing
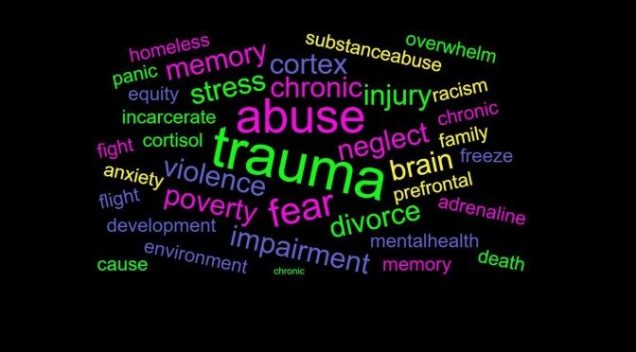
When trauma is commonly thought of most would expect that it results from war or other instances involving numerous encounters of overwhelming stress. Although these instances certainly pose a significant risk of trauma, trauma can be more easily obtained by numerous different types of events and is encountered frequently on a regular basis. About 6 out of every 10 males and 5 out of every 10 females will face trauma at least once some point in their lives (National Center for PTSD). In addition to that, about 7 to 8 percent of the population will have posttraumatic stress disorder (PTSD) at some point during their lives (National Center for PTSD). Trauma is defined as “an emotional response to a terrible event like an accident, rape or natural disaster.” (American Psychological Association). Due to the ability of trauma to affect so many people not only in the U.S. but worldwide it is important to understand neurobiology and the effects such events have on the brain. Understanding the neurobiology of trauma is a must for treating such trauma medically and will aid in teaching coping methods to those suffering from these traumatic events. With that being said, the developed understanding of the neurology seems to successfully identify the parts of the brain that are stimulated and associated to disorders relating to trauma yet medicine fails to permanently cure the issue and only keeps those under balance while on the medication. Considering that a lack of medicine can leave one defenseless if not taken or forgotten should medicine be an approved or considered a reliable form of treatment to trauma?
“When someone experiences a traumatic event or experiences extreme fear, brain chemistry is altered and the brain begins to function differently--this is called the "Fear Circuity" and it is a protective mechanism which we all have inside of us.” (University of Northern Colorado). Knowing that a traumatic event can alter the brains chemistry leaves an open door within neurobiology to examine and treat the lasting effects. “Sertraline and paroxetine are the only antidepressants approved by the FDA for the treatment of PTSD” (Alexander, 2012). To this date there is no known permanent treatment of PTSD by prescription drugs and all are needed to be taken regularly and prescribed a dosage. Medications work by altering neurotransmitter production and transmission (Rousseau, 2021). However, other methods like yoga “can help to redirect the firing of neurons, or even create new neurons through two processes, called neuroplasticity and neurogenesis.” (Rousseau, 2021). Suicide rates of those dealing with PTSD is as much as thirteen times as many as those not dealing with PTSD (Gradus, 2017). Since a medical form of treatment cannot be relied on if they are not obtainable at all times it poses a clear significant risk to those dealing with PTSD. As pointed out in the film “Healing a Soldier’s Heart” there have been over 110,000 suicides since the Vietnam war which is almost twice as many casualties during the war of 58,000 (Healing a Soldier’s Heart, 2013). With this in mind, unless a more sustainable one time treatment becomes an option, teaching coping techniques should be more of a recommended form of treatment.
Of course there are extreme cases where teaching coping methods are not sufficient enough and the use of medication is needed to support the healing process. The message here is not to discredit current medications but to raise the concerns on its reliability and support future alternative methods that provides more of a cure than a temporary fix.
Works Cited
Alexander, W. (2012, January). Pharmacotherapy for Post-traumatic Stress Disorder In Combat Veterans: Focus on Antidepressants and Atypical Antipsychotic Agents. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3278188/
Gradus, J. (2017). PTSD and Death from Suicide. Retrieved from https://www.ptsd.va.gov/publications/rq_docs/V28N4.pdf
Neurobiology of Trauma. (n.d.). Retrieved from https://www.unco.edu/assault-survivors-advocacy-program/learn_more/neurobiology_of_trauma.aspx
Olsson Stephen, & Cultural & Educational Media (Producers), & Stephen, O. (Director). (2013). Healing a Soldier's Heart. [Video/DVD] The Video Project. https://video.alexanderstreet.com/watch/healing-a-soldier-s-heart
Rousseau, D. (2021). CJ 720 Module 1. Boston University. https://learn.bu.edu/ultra/courses/_75565_1/cl/outline
Trauma and Shock. (n.d.). Retrieved from https://www.apa.org/topics/trauma
VA.gov: Veterans Affairs. (2018, September 13). Retrieved from https://www.ptsd.va.gov/understand/common/common_adults.asp
Restitution and Victims of Child Exploitation
Years ago, while working as an analyst processing evidence in child exploitation cases, I met a victim of one of the most widely circulated child pornography series to date. While the abuse occurred when the victim was ten and eleven, I met her right before she started college, after her fugitive father was arrested and finally prosecuted for his crimes. She recounted how the abuse was traumatizing enough, but later discovering her father traded images and videos of the abuse online was almost too much to bear. She also discussed the long-term implications from that knowledge, fearful that every person she encountered might recognize her from those images of the worst moments of her life. Knowing that so many individuals took pleasure in her pain was also something she couldn’t comprehend. Meeting her was surreal, as I viewed images of her abuse in nearly every case I examined, and I could not even fathom what she had experienced in her young life. This encounter was almost 15 years ago, and it still has a great impact on me, and I am devastated for her (and all victims of this sort of crime) that those images are probably still being circulated every day, with the victim never being able to escape the daily reminder of the abuse.
Although I am no longer certain if this is the norm, when I worked in that field, it was a requirement that the identified victim of child exploitation be notified every time their image appeared in a case, with some victims potentially notified multiple times a day, every day of the week, due to the frequency their images were traded. While I understand the intent behind this requirement, in reality, it meant the victim faced a constant reminder of the abuse, impeding their ability to move forward. Due to this reason, some of the victims assigned an intermediary to receive the notifications, as they could not handle the constant influx of notices.
Assisting victims of crime and trauma is a challenging situation, as there is no way to erase the impact of what happened to them. “Trauma impacts the individual, his or her relationship with family and friends, his or her ability to hold jobs, and the way he or she interact with the world around him or her. It can change life paths, alter personal abilities, and cause physical and neurological damage that may or may not be repaired” (Rousseau, 2021, p. 8). Every person handles trauma differently, and every case is different, with some offenders penalized to the maximum extent of the law, while others get no penalty. The concept of restitution continues to be brought up when discussing victims of crime, although there are advocates both for and against employing monetary compensation for crime victims. "Restitution means restoring someone to the position occupied before a particular event took place,” while the “purpose of restitution is to make a victim whole” (Boe, 2010, p. 210). Forcing an offender “to pay a monetary fine, often in addition to serving a prison sentence, forces an individual defendant to address the harm his crime has caused to the individual victims of his crime and to society. Victims, especially victims of child pornography, frequently suffer both financial and emotional losses because they have to seek counseling or medical services for the rest of their lives” (Boe, 2010, p. 211). While money will never make a crime victim “whole” again, and will never be able to “restore” them to the person they were prior to the traumatic event, monetary compensation can help alleviate some of the financial hurdles they may face with seeking treatment or account for some of the financial losses they may have incurred due to their trauma.
However, one challenge surrounding restitution is assigning a financial sum commensurate to the impact on the victim, which is seemingly impossible, as the full impact can never fully be accounted. “Knowing that thousands of individuals possess images and video of oneself being raped and sexually abused in humiliating fashion can inflict deep, life-lasting trauma that extends well beyond the initial sexual abuse. This emotional trauma results in economic burdens,” including psychological counseling costs and lost income (Cassell et al., 2013, p. 73). Additionally, “determining each victim's losses requires a careful analysis of how each victim's life is impacted by child pornography,” which includes economic, emotional and physical losses, with restitution payments providing “not only psychological counseling, but also vocational and educational training to move forward with their lives” (Cassell et al., 2013, p. 74).
While I don’t have any concrete ideas regarding a “just” way to compensate various victims of crime, I do think some sort of financial reimbursement is warranted to cover some of the long-term medical, legal and therapeutic expenses, which can accumulate quickly. An additional challenge also arises when trying to recoup money for the crime victim, especially if the offender has no financial means to repay the victim. A victims’ compensation fund has been discussed, as have many other ideas, but the practical enforcement of restitution might also impact a victim long-term, if they are additionally traumatized by the justice system. Overall, I find the idea of restitution a fascinating and relevant topic concerning crime victims and the impact of trauma, although there is no easy solution when figuring out how to implement it. For me, meeting the victim was a huge reminder that we never know what anyone else has gone through or is currently going through, as looking at her on the surface, no one would have ever guessed what she was battling under the surface. Overall, it reminded me that when discussing some of these issues regarding restitution, or punishment or rehabilitation, a real-life victim is on the other end, and the human impact element is always the one that needs top consideration.
References
Boe, A. B. (2010). Putting price on child porn: Requiring defendants who possess child pornography images to pay restitution to child pornography victims. North Dakota Law Review, 86(1), 205-230.
Cassell, P. G., Marsha, J. R., and Christiansen, J. M. (2013). The Case for Full Restitution for Child Pornography Victims. George Washington Law Review, 82(61), 61-110.
Rousseau, D. (2021). Module 1 Study Guide [Notes]. Boston University Metropolitan College.
Traumatic Experiences in Correctional Facilities: Who Has it Worse? Correctional Staff or Those who are Incarcerated
Traumatic Experiences in Correctional Facilities: Who Has it Worse? Correctional Staff or Those who are Incarcerated
When thinking of what it would be like to be incarcerated, the lay person can base their perception on any number of popular televisions shows or movies; abusive staff, gangs, stabbings, rapes and a pervasive culture of violence. While these things do occur, in some facilities much more than others, many short term, low custody sentences may not experience these things firsthand. However, the constant fear of the above referenced items coupled with poor (if not disgusting) food quality, strip searches, group showers, unsanitary conditions, lack of access to family/friends, lack of sleep due to keys, doors, and cell checks, and reduced/delayed access to medical and mental health may in fact lead to greater negative emotions and trauma. Any piece or combination thereof can lead to PTSD upon release back into society. In addition, “Other factors are interwoven into the pathogenesis of this condition, including the many risk factors that underlie the behavioral and thought patterns of many criminals. These include childhood traumas such as extreme poverty, child abuse by their parents or caregivers, experiences of neglect, physical and sexual abuse, as well as other forms of mistreatment” (Thomas, 2019).
According to various research projects:
- Even before entering a prison or jail, incarcerated people are more likely than those on the outside to have experiencedabuse and trauma (Thomas, L, 2019).
- An extensive 2014 studyfound that 30% to 60% of men in state prisons had post-traumatic stress disorder (PTSD), compared to 3% to 6% of the general male population (Wolff, N, et al, 2014).
- 7% of womenin state prisons experienced childhood abuse, compared to 12 to 17% of all adult women in the U.S.. (BJA, 1999).
The below chart is from the Prison Policy Initiative article titled No escape: The trauma of witnessing violence in Prison:
| Estimating the prevalence of violence in prisons and jails | ||||
| Reported incidents and estimates | ||||
| Indicator of violence | State prisons | Federal prisons | County jails | Source |
| Deaths by suicide in correctional facility | 255 deaths in 2016 | 333 deaths in 2016 | Mortality in State and Federal Prisons, 2001-2016; Mortality in Local Jails, 2000-2016 | |
| Deaths by homicide in correctional facility | 95 deaths in 2016 | 31 deaths in 2016 | ||
| “Intentionally injured” by staff or other incarcerated person since admission to prison | 14.8% of incarcerated people in 2004 | 8.3% of incarcerated people in 2004 | Survey of Inmates in State and Federal Correctional Facilities, 2004 | |
| “Staff-on-inmate assaults” | 21% of incarcerated men were assaulted by staff over 6 months in 2005 | Wolff & Shi, 2010 | ||
| “Inmate-on-inmate assaults” | 26,396 assaults in 2005 | Census of State and Federal Adult Correctional Facilities, 2005 | ||
| Incidents of sexual victimization of incarcerated people (perpetrated by staff and incarcerated people) | 16,940 reported incidents in 2015 | 740 reported incidents in 2015 | 5,809 reported incidents in 2015 | Survey of Sexual Victimization, 2015 |
| 1,473 substantiated incidents in state and federal prisons and local jails in 2015 | ||||
The above charts and studies, however, only examined the effects of correctional environments on those who were incarcerated inside by judicial order and did not consider those who work inside the facilities, often for long and mandated shifts. Not as many studies could be found on correctional staff related trauma. But trauma and stress amongst staff can easily be imagined: reviewing horrific case files; witnessing traumatic events; mandatory overtime; role ambiguity; and constant disrespect by the inmate population. “According to a 2015 article by the National Commission on Correctional Health Care, correctional employees experience higher rates of stress-related illnesses that contribute to low levels of job satisfaction, which has been linked to burnout and is thought to lead to compassion fatigue” (Pittaro, M., 2020).
In addition, a study conducted and published this year found that correctional officers self-reported significantly higher exposure to potentially psychologically traumatic events than other medical and wellness workers. Moreover, correctional staff also self-reported greater rates of symptoms of mental disorders, including PTSD, social anxiety, panic disorder, and depression, among others (Fusco, N., et al, 2021).
Based on the above referenced data and numerous additional uncited studies, it is evident from the research and probably obvious to the average law abiding civilian, that both correctional staff and inmates are exposed to the unimaginable and unfathomable behind the walls. Typically, opposing sides prevent the evolution and availability of growth for each of these populations: those who may believe that inmates deserve this and should not be afforded anything when being punished and those that may feel that correctional staff are tough and know what they sign up for. Acknowledging the equality in the two groups and making available trauma informed approaches to care for the inmate populations and programming for self-care for staff is critical to reduce these numbers and ensure smooth transitions for each in society. The truth is, that nearly all inmates will one day be released into society and, in addition, will be existing with us. Moreover, staff as well are living amongst us, on their often-limited time off, and should as well be able to ‘leave it at the gate’ in terms of their work stressors. To that note, similarly, one a sentence and work shift is complete, any individual should be, and we should want them to be, functioning, healthy and productive members of the society in which we all live.
References:
Bureau of Justice Assistance (BJA). 1999. Prior Abuse Reported by Inmates and Probationers. https://bjs.ojp.gov/content/pub/pdf/parip.pdf.
Fusco, N., Ricciardello, Jamshidi, Carleton, Barnim and Hilton. (February 15, 2021). When Our Work Hits Home: Trauma and Mental Disorders in Correctional Officers and Other Correctional Workers. National Institutes of Health. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7917131/.
Pittaro, Michael. March 24, 2020). Correctional Officers and Compassion Fatigue. Psychology Today. https://www.psychologytoday.com/au/blog/the-crime-and-justice-doctor/202003/correctional-officers-and-compassion-fatigue.
Thomas, Dr. Liji. (February 27, 2019). Prisoner Post Traumatic Stress. Medical Life Sciences News. https://www.news-medical.net/health/Prisoner-Post-Traumatic-Stress.aspx.
Widra, Emily. (December 2, 2020). No escape: The trauma of witnessing violence in Prison. Prison Policy Initiative. https://www.prisonpolicy.org/blog/2020/12/02/witnessing-prison-violence/#lf-fnref:1.
Trauma Informed Policing by Frederick Morse
In recent years perhaps no profession has received as much scrutiny as law enforcement. Americans are redefining social norms and expecting more professionalism and accountability from law enforcement. One of the areas in law enforcement that has been beneficial, yet not without growing pains, has been the proliferation of body-worn video cameras. An additional facet of American life that has also received a fair amount of attention is trauma and mental illness. Research has shown that early childhood trauma can result in hindered growth resulting in uncontrolled anger, inappropriate behavior, disregard for rules, and drug or alcohol abuse (Rousseau, 2021). These precursors often result in contacts with law enforcement.
In the United States, a growing number of service requests for law enforcement similarly involve police interaction with vulnerable individuals or those experiencing a psychologically based crisis. A recent study in Scotland revealed that approximately 80% of all calls for service for law enforcement were non-criminal in nature (Gillespie-Smith, 2020).
With this dynamic in mind, scholars in Scotland conducted research where they exposed police personnel to trauma informed practices. Specifically, the study chose one police division and showed them the documentary “Resilience: The Body of Stress and Science of Hope.” The documentary explained how chronic stress releases hormones within the body of children which then results in dysfunction in the minds and bodies of youth. After viewing the film, the police personnel were given an overview of the 1998 Adverse Childhood Experiences (ACE) study and scores. There was a panel of experts available for questions and to provide further context for the data.
Police personnel learned that in Wales, individuals with an ACE score of four or more were twenty times more likely to be incarcerated at some point in their life than the general public (Bellis, 2015). Similarly, the officers learned that approximately 89% of the prisoners in Wales reported at least one ACE (Gillespie-Smith, 2020). Police personnel who received the trauma informed training were then questioned as to their attitudes and understanding about suspects, witnesses, and victims. The researchers then compared the answers with answers from officers from another police division that did not receive the trauma informed policing training. The answers were not significantly different (Gillespie-Smith, 2020). Many of the officers who received the training expressed confusion about the ACE score research. The officers indicated that the trauma had occurred before their involvement and they failed to see how the new knowledge could benefit their current role. This was a common theme in the feedback from the participants (Gillespie-Smith, 2020).
On its face, the scholarly work in Scotland appeared to be unremarkable. However, if law enforcement agencies in the United States could build upon this trauma informed approach to policing and combine it with the technology of body worn video, real progress could be made. Law enforcement personnel have countless contacts and calls for service with individuals with mental health needs. A trauma informed approach to these calls for service could curtail any use of force and would result in decreasing further trauma to the individual in crisis or the officer.
Law enforcement administrators need to seek out strategies for improved professionalism and techniques for de-escalation. With the use of body worn video, contacts with individuals in crisis or mental health decompensation can be reviewed by law enforcement trainers and mental health professionals to improve officer responses and protocols. All contacts with citizens with mental health needs would be given a unique computerized clearance code making it easier to identify and retrieve the incidents for later review. The review of body worn video would be for educational purposes only, with the goal of improving trauma informed practices for law enforcement personnel. Police agencies could generate training videos from body worn video footage from actual interactions. The videos would include instructional narratives from mental health professionals and would be disseminated to other stations and personnel. A secondary objective would be to ensure that law enforcement personnel are getting the necessary and timely assistance from mental health agencies. If both agencies can work in a collaborative manner, individuals in crisis might receive professional intervention and proper care instead of a trip to the county jail.
Submitted by: Frederick Morse
Works Cited
Bellis, M. A. (2015). Adverse Childhood Experiences and their Impact on Health-Harming Behaviours in the Welsh Population. Wales: Cardiff: Public Health.
Gillespie-smith, K. B. (2020, August). Moving Towards Trauma-Informed Policing: An Exploration of Police Officer's Attitudes and Perceptions Toward Adverse Childhood Experinces (ACEs). Retrieved from https://www.research.ed.ac.uk/en/publications/moving-towards-trauma-informed-policing-an-exploration-of-police-#:~:text=In%202018%20Ayrshire%20Division%20of%20Police%20Scotland%20announced,perceptions%20and%20attitudes%20towards%20becoming%20a%20trauma-in
Rousseau, D. (2021). Trauma and Crisis Intervention. Module 2 Study Guide. Boston University.
Liquid Trauma Treatment and Law Enforcement
For most professionals, when colleagues ask to grab a few drinks after work, this is seen as a friendly gesture to build relationships at the workplace. For law enforcement this can be seen and used as a way to cope with the stress and trauma from the job or to self medicate for anxiety, depression or post-traumatic stress disorder. While the exact number is hard to calculate, it is estimated that approximately 23% of all police officers in the United States are alcoholics. To put that into perspective, there are an estimated 800,000 sworn officers in the United States which would mean approximately 184,000 officers are considered alcoholics. Some officer’s may have already been or will eventually become alcoholics, prior to being hired, due to genetic predisposition or the environment they were raised in. While this may be true, it is easy to see how the job and the lack of mental health resources available would lead to such troubling statistics.
The day I was hired and sworn in as a police officer, a family friend, who was an active duty police officer at the time, told me that I now had “a front row seat to the greatest show on earth.” Without knowing what the job entailed and the mental health issues that face police officers, I find it somewhat ironic that my family friend and I were drinking at the time. I saw the occasion as a celebration while he may have seen it as a way to self medicate to ease the pain of the demons he carried with him as a result of being a cop. The idea that I could sign up for a job where every day, every hour, and every minute was different sounded too good to be true. And at first, this was exactly what it was like for me every time I pulled that bullet proof vest over my head, buttoned up my uniform shirt, and shined my boots. Today, every time I put on that vest, I am quickly overcome with stress and anxiety of the unknown. The adventures of the job and the adrenaline filled incidents that I yearned for quickly became mundane and I felt as if I was becoming complacent which is a killer in this job. “The very nature of police work includes regular and ongoing exposure to confrontation, violence, and potential harm. Exposure to potentially traumatic experiences on a regular basis sets the stage for a series of mental health complications, including posttraumatic stress disorder (PTSD)” (Maguen et al., 2009, p. 754).
Perhaps it was because of the COVID lockdowns without much else to do, or perhaps it was me subconsciously self medicating from the stress of the job, but I soon found myself drinking almost every night. My fiancé recognized this and quickly made me realize that it was becoming a problem. I am extremely fortunate and grateful that my fiancé had the courage to speak up and confront me about my drinking habits. For many this resource is not available and they are left searching for help while fighting to stay anonymous. The search may continue long enough where officers feel they don't have any options and end up take their own lives. “Law enforcement suicide is real and is the number one killer of police officers,” occurring “1.5 times more frequently than suicide in the general population” (Rousseau, 2021, p. 7).
The stigma around mental health and its subsequent treatment is extremely prevalent in law enforcement but the more alarming issue is the lack of resources available to officers. This may be because of the stigma but leaders within the profession have a moral and ethical obligation to do better. I have heard from some classmates that their departments offer mandatory mental health services without questions asked and their colleagues are far better for it. This is an example of forward thinking leadership while combating the stigma that surrounds mental health. The country needs more leaders like this to step up and take care of their own. This will not only lead to healthier officers but it will also lead to better relationships with the public they serve.
Bibliography:
“How Common Is Alcoholism with Police Officers? - The Recovery Village.” The Recovery Village Drug and Alcohol Rehab, The Recovery Village Drug and Alcohol Rehab, 22 Dec. 2020, www.therecoveryvillage.com/alcohol-abuse/related-topics/facts-alcoholism-police-officers/.
Maguen, S., Metzler, T. J., McCaslin, S. E., Inslicht, S. S., Henn-Haase, C., Neylan, T. C., & Marmar, C. R. (2009). Routine Work Environment Stress and PTSD Symptoms in Police Officers. Journal of Nervous & Mental Disease, 197(10), 754–760. https://doi.org/10.1097/nmd.0b013e3181b975f8
Rousseau, D. (2021). Module 6 Study Guide [Notes]. Boston University Metropolitan College.
Self-Care and Trauma
People who experience trauma deserve to be free from the weight and pain that it bears upon them. Throughout this class, we have discussed multiple treatment methods that can work individually or that can be used together to find the best treatment plan for the individual. Not all treatments are as widely accepted as others and one that seems to walk on that fine line is self-care. Self-care however is an important part of healing from the trauma, but it should be started when the individual is ready for that experience. Trauma affects our entire body, mind, and our whole being. When all of these aspects are affected we have a harder time being present, connecting, and relating to others. By focusing on ourselves through self-care, our mind and body can work together again to create a healthy and happy lifestyle that may have not existed before.
Highland Springs Clinic mentions that on one’s journey to healing and recovering from a traumatic event, it is important to remember the practice of self-care. They also wrote that “self-care is not commonly the first method survivors think of when they are overcoming a traumatic experience, however, it is a critical part of healing”(Hood,2020). Before starting any kind of trauma therapy, it is important to understand what trauma is and how it may present itself in you. Knowing when to start self-care is dependent on the individual and they have to allow themselves to be ready. Self-care is not the same for everyone, but listening to your body and mind and what it needs is a first step for starting this journey. Our body usually recognizes what we need and will signal to us when the time for recovery is here. Highland Springs Clinic mentions some areas of self-care that are good to start with are get more rest, find someone to talk to, journal about it, use exercise as a tool, and find engaging hobbies (Hood, 2020). While this is only a shortlist of self-care options they are good places to start for people who are ready to treat their trauma by loving themselves.
Whitney Goodman LMFT, a licensed psychotherapist brings up a good point that self-care is supposed to make us better in the long-term and that it is not a quick fix. In society now, the term “self-care is officially a commodity, and people are buying it off the shelves to prove that they care about themselves”(Goodman, 2019). It is important that people who chose self-care to help them with their trauma understand that learning to love yourself and take time for yourself is not an easy process. Goodman stated “real self-care happens in the decisions you make every day and it requires practice, commitment and putting yourself first and getting in touch with what you really need, not just what you really want”(Goodman, 2019). Her short list of self-care is: get in touch with your feelings and actual needs, practice kindness, and ask yourself “what do I need at this moment”. One big point that Goodman and Highland Springs Clinics mentioned is staying away from drinking or using substances since it is not self-care. There are so many different kinds of self-care out there, that experimenting with them will help us find which ones work for us. It is important that people who have experienced trauma believe that they deserve self-care before starting to practice it.
Everyone that goes through a traumatic experience reacts differently emotionally, psychologically, and physically. Being able to accept and be ready for the step of self-care is important to accept the responsibility for yourself, your body, and your mind. Finding a positive self-care routine when ready to embark on the journey will help the overall healing process. It is important to remember that there is no right or wrong way to self-care, it is all about what helps that individual after trauma to become whole again. Dr. Bessel Van Der Kolk writes “the full story can be told only after those structures are repaired and after the groundwork has been laid: after no body becomes some body”(Van Der Kolk, 2015, p.249). Trauma is stressful, but acting on self-care can alleviate that stress. As well as realizing that the trauma needs to be dealt with in a positive way and wanting to deal with it will help accomplish the first step with the journey of self-care.
References
Goodman, W. (2019, July 12). When Self-Care Becomes a Weapon. Psychology Today. https://www.psychologytoday.com/us/blog/healing-together/201907/when-self-care-becomes-weapon.
Ph.D., D. Julia. Hood. (2020, January 27). The Importance of Self-Care After Trauma. Highland Springs. https://highlandspringsclinic.org/blog/the-importance-of-self-care-after-trauma/.
Ocrcc. (2020, October 12). self-care Archives. OCRCC. https://ocrcc.org/tag/self-care/.
Van Der Kolk, B. (2015). The Body keeps the score brain, mind, and body in the healing of trauma. Penguin Books.
Acupuncture as Trauma Therapy
Over the relatively short period of time that trauma treatment has been studied, there has been a myriad of different methods proven to help trauma victims in one way or another. Despite this, there is yet to be a cure-all that works completely for every individual and every trauma. To fully accept the reality of a trauma and be free from the weight it bears, multiple treatment methods working in tandem with one another is the best approach for healing.
One treatment method that is less often discussed but proven effective is acupuncture. Acupuncture is an ancient Chinese practice that utilizes small needles placed along pressure points on the body to help with energy flow and pain relief. Chinese documents dating as far back as 100 BCE describe the system of diagnosis and treatment that is now recognized as acupuncture (White & Ernst, 2004). The original idea of flowing meridians in the body has given way to modern neurology’s explanation that the needles stimulate nerve endings and brain function (White & Ernst, 2004). While the practice is centuries old and has been utilized in cultures across the globe, there is surprisingly little research on its effects.
Although there is little research on the subject, other forms of therapies have developed from its principles. Emotional Freedom Techniques is a more common method that, while self-administered, relies on the same bodily energy flows as acupuncture and has also been proven to cure the physical and psychological effects of trauma. In a survey following the September 11th attacks, the 225 individuals questioned said that acupuncture was the most effective method in helping them overcome the immediate trauma of being in the Towers (Van der Kolk, 2014). Acupuncture has also been found to be a “promising treatment option for anxiety, sleep disturbances, depression and chronic pain” as related to the trauma spectrum responses (Lee et al., 2012). While more research is needed to identify the mechanism of action between the needles and the actual relief, the success stories speak for themselves and make the practice a worthy contender for comorbid treatment.
The way acupuncture can aid in trauma recovery is by alleviating the symptoms either directly or residually caused by the event. For example, after a car accident, an individual might suffer pain in their neck and experience anxiety whenever they are in a car again. Acupuncture can help to relieve the neck pain that both hinders quality of life and acts as a constant reminder of the accident. Chronic pain is also a common side effect of adverse childhood experiences. When an adult comes in for therapy with a long history of repeat traumas, alleviating physical pain is a great starting point to begin recovery. This allows for a greater sense of control in one’s own body and opens doors for further therapeutic practices like yoga and exercise that would not have been possible with chronic pain. Acupuncture may not be the cure-all that therapists and researchers are looking for to help their patients overcome past traumas but its longstanding history and overwhelming success rate for non-trauma related pain demands more research be conducted on the practice’s effects on trauma.
References:
Lee, C., Crawford, C., Wallerstedt, D., York, A., Duncan, A., Smith, J., Sprengel, M., Welton, R., & Jonas, W. (2012). The Effectiveness of Acupuncture Research Across Components of the Trauma Spectrum Response (TSR): A Systematic Review of Reviews. Systematic Reviews, 1(1). https://doi.org/10.1186/2046-4053-1-46
Van der Kolk, B. A. (2014). The Body Keeps the Score. [VitalSource Bookshelf]. Retrieved from https://bookshelf.vitalsource.com/#/books/9781101608302/
White, A., & Ernst, E. (2004). A Brief History of Acupuncture. Rheumatology, 662–663. https://doi.org/10.1093/rheumatology/keg005.
Ambiguous Loss
"I intentionally hold the opposing ideas of absence and presence, because I have learned that most relationships are indeed both."
- Pauline Boss, Ph.D.
In the last 50 years, our understanding of the spectrum that grief encompasses has grown immensely. Yet, grief is still wildly misunderstood and unrecognized in our culture. For some, we grant specific labels to identify their grief in a concrete way: a widow, bereaved parent, or a sibling of a fallen soldier. Almost always, these labels tell us that someone’s grief is valid because they are grieving the death of a loved one. These labels tell us: “her husband died, you are free to bring a casserole to her door,” or “his sister died in the war, you may write on his Facebook wall that you are thinking about him on Memorial Day.” We know what to do with concrete loss. We know the social rules and instructions that come with each label that we have attached to concrete grievers.
But for many, loss and grief reaches beyond the concrete labels; beyond the dead; beyond a final resolution. This type of grief is now known as “ambiguous loss.” This type of loss carries great unknowns and no societal instructions in how to react. I was first hit with ambiguous loss when we had to hand back the baby girl who was literally minutes away from being our legally adopted daughter. Not only did we have a failed adoption, but she went to a family member that knowingly abused her and did not support any continued relationship with our family.
This little one will have no memory of being a part of our family, even though (in our eyes) she is nothing short of being our first daughter - the one who turned me into a mother and my husband into a father. Suddenly, my husband and I were caught in the thick of grieving our child who was still living. We grieved her future, tucked away her nursery, told our parents that they were no longer grandparents, and were completely heartbroken. We mourned the loss of a future with the daughter we would never see again. But, she is still alive. There was no funeral, memorial, title, or label that told others how they could react.
The first thing I did was turn to my community to look for support groups. But of course, there are no support groups for “childless parents with living children.” When people asked me if I had any children the answer “not yet!” seemed fake; it seemed to deny our baby girl’s existence. But the answer “yes,” did not work either. Yet, no one cutting your hair or chatting at the farmers’ market wants a detailed story of how your daughter is no longer your daughter. Not having anywhere to turn for support became extremely isolating. It made me feel as though my loss must not be real and that I needed to simply “be grateful” it was just a failed adoption, rather than something worse.
This kind of thinking took my mourning to a level of isolated depression. It was not until I started seeing a grief counselor that she explained to me there are many different types of losses. She introduced to me the term “ambiguous loss,” which is “grief without a resolution or without a death” (Boss, 2020). From there, I learned that there has actually been great amounts of research on the stinging pain of ambiguous loss. She shared with me that while we like “black and white” losses in our culture, most loss is ambiguous. When I began opening my world up to honoring all types of loss, no matter how unresolved my loss still was, I was able to truly begin healing.
So what do we call the loss of a father who is mourning his brain dead child that is still right in front of him? How do we honor the grief of the refugee in our neighborhood who does not know if their family members are still alive? At what point do we reach out to the mother of a child on death row? How do we recognize the loss of our friend whose parents are alive, but are lost deep within in the affects of dementia? Are we supposed to give flowers to the childless neighbor who has suffered 8 miscarriages? The way we recognize and make room for grief in our culture either helps heal or further traumatizes those who are suffering from ambiguous loss.
Psychologist Abby Maslin shares that “ambiguous loss is learning to live with a lot of uncertainty, never knowing if you will get an end result” (“Grieving the Living,” 2020). Because of this uncertainty, Dr. Boss explains that this type of loss often “erodes our sense of mastery and destroys our belief in the world as a fair, orderly, and manageable place” (Boss, 2020). Most people facing this kind of loss have faced the “well, at least the person you love is...” comments. This kind of attitude only further isolates the ambiguous griever.
Those who are suffering from ambiguous loss still work through the same grief cycle as someone who is suffering from concrete loss (“Ambiguous Grief,” 2020). Today, research suggests that the methods we use to remember the dead can be used in the same ways to honor ambiguous loss (Hugstad, 2017). Experts also share that “remembering [that] the present does not override the past” is a powerful way to honor what is missing in ambiguous grieving (“Ambiguous Grief,” 2020). While it is our immediate desire to make someone else’s loss concrete, we must understand that this is simply impossible with unresolved grief. Dr. Boss explains that “while such losses cannot be resolved, they can be acknowledged and supported” by professionals, family members, friends, and communities (Boss, 2020). When we make room for these types of losses we are offering our permission to connect with another’s pain rather than push them further into the darkness. Light and healing cannot enter where there is no room.
So how about we bring the casseroles, drop off the flowers, and bake the cookies for those that we see with unresolved grief? Will you look your ambiguously-grieving friend in the eyes and say “no matter how messy your pain is today, I am here for you?” How will you decide to recognize that all grief looks different even if there is painfully no resolution in sight? Will you wait for a concrete label to tell you how to support the grieving or will you pave your own path to honor whatever loss comes your way? One thing is certain when it comes to ambiguous losses: they are not going anywhere. Because of this, it is up to us to make room for this type of unique, yet common grief. Only then can true healing begin.
Sources:
- Ambiguous grief: Grieving someone who is still alive. (2020). Retrieved from https://whatsyourgrief.com/ambiguous-grief-grieving-someone-who-is-still-alive/
- Boss, P. (2020). About Ambiguous Loss. Retrieved June 20, 2020, from https://www.ambiguousloss.com/about/
- Grieving The Loss Of A Person Still Living. (2020). Retrieved from https://americanbrainsociety.org/grieving-the-loss-of-a-person-still-living/
- Hugstad, K. (2017, November 30). Grieving the living: When your “lost” loved one is still alive. Retrieved from https://whatsyourgrief.com/ambiguous-grief-grieving-someone-who-is-still-alive
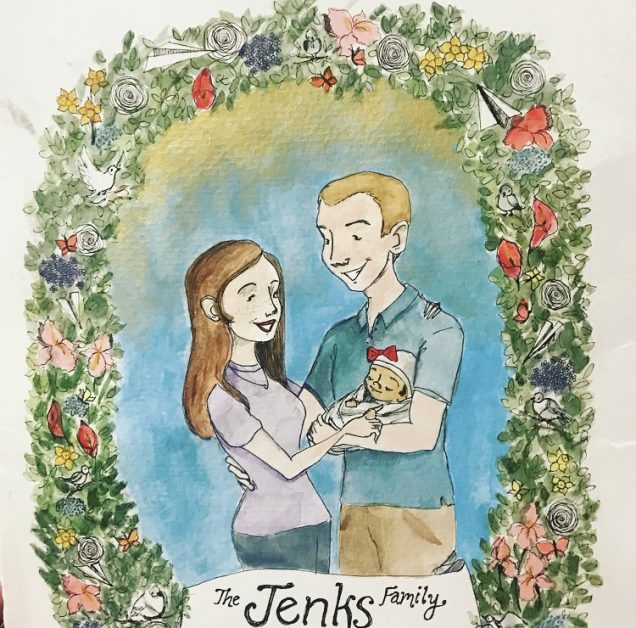
- This is a photo of a painting that my dear friend made to honor the daughter is no longer "ours." It was such an amazing feeling to have this loss recognized and to have this to keep forever!
From Prison to PhD: Post Traumatic Growth after Incarceration
Prison inspires a culture of its own. To be given a new name, rather a number, that you are to be called upon and to be stripped of your previous identity. To be stripped naked and given standardized attire to be worn day in and day out. To be surrounded by uniformed personnel with metal handcuffs and weapons around their belt. To be beaten, humiliated, degraded, pent up in the dark like an animal, and to constantly fear for your life with gruesome images that may linger in your mind for the rest of your life. How can anybody be expected to return from prison and released back into their community as if their life, their mind, and experience of the world has been unaltered? How can anyone expect to move forward and grow after what many may call to be a traumatic incarceration? Mika’il DeVeaux, a former incarcerated young man and current PhD student and director of nonprofit organization aimed to help explore the idea and meaning of success as defined by seventeen men who had three years to try and survive a post-incarceration life successfully. Among his interview with men, he explored the social support that allowed them to reach that success. “The most important you know [is] family.” Family allowed the formerly incarcerated men to be surrounded by a positive influence that created a sense of yearning of success while preventing them from gravitating to the former negative influences that may have led them to reincarceration. Charles, one of the participants in the study stated, “relationships play a key role…I am talking about support relationships…about making sure that we are accountable.” Keeping in touch with “professional change agents” were also attributed to post-prison success. Among all of the other variables that the men used to define their success such as housing, employment, education, and building a family, the theme that surrounded each individual’s concept of success incorporated the idea of a strength behind social support.
As Mika’il DeVeaux explained about his own life experience, “Prisons are institutions that have a life of their own, but the life is an abnormal one. It is a life filled with deprivations, with isolation, with fantasy and imagination, and with hanging on to what was, despite little preparation for what is to come…with little reason to ponder what life could be like after prison.” It is easy to become trapped in your own mind while your physical body is trapped in a cell. Having voices from loved ones to remind you that there is more than bars and concrete is overwhelmingly helpful for inmates.
Although not everybody experiences prison in the same way, it seems to be that it is beyond a coincidence that these men found success after prison with the aid of social supports from positive influences. “Upon my release, I was helped by the support network I maintained during my incarceration.” Mika’il explains that his family provided the support that he needed to imagine what life after prison might be like. Having maintained connections with people he knew from his previous life, such as his childhood friend, and persons that would introduce him to his new life such as his professors,e helped to establish a sense of a future and reintegration into society. A sense of hope, renewal, and growth after a traumatic experience has been strengthened by the social support that has allowed many men like Mika’il and those he welcomed into his study to come out stronger from the traumatic experience of incarceration.
References:
DeVeaux, M. (2013). The Trauma of the Incarceration Experience. Harvard Civil Rights – Civil Liberties Law Review, 48, 257-277. Retrieved from https://heinonline-org.ezproxy.bu.edu/HOL/Page?collection=newyork&handle=hein.journals/hcrcl48&id=261&men_tab=srchresults
DeVeaux, Mika'il, "Fitting-in: How Formerly Incarcerated New York City Black Men Define Success Post-Prison" (2017). CUNY Academic Works.
https://academicworks.cuny.edu/gc_etds/1822
Traumatic Divide
St. Louis city has a terrible reputation as being a dangerous city overrun by crime. Most of the crime is centered in two districts of northern St. Louis City. “There is this conception of the city as crime-ridden throughout,” says University of Missouri–St. Louis criminology professor Richard Rosenfeld. Looking at the homicide rate, which ranks at or near the top among U.S. cities each year, it appears that the violent crime risk is the same everywhere throughout the city. Rosenfeld’s research says otherwise: “It’s very high in a few neighborhoods on the north side, and in and around Dutchtown, and hardly anywhere else.” (Woytus, 2019).
Working for the Federal Public Defender’s Office in St. Louis, MO, I represent people accused of federal crimes. Most are young, African-American men, indigent, with at least one mental health diagnosis. Regardless of the type of crime they are accused of committing, their personal stories of trauma incurred as children, events they have witnessed, or violence they have committed to simply survive is a recurring theme. Many of them grew up in the aforementioned districts.
Delmar Boulevard is referred to as a “divide” in the city. South of this divide, you will find $500,000 homes and wine bars. This southern neighborhood, according to U.S. Census data, is 70 percent white. To the north of the divide: collapsing houses, gang signs spray painted on every corner, trash in the streets, and neglected infrastructure. The neighborhood is 99 percent black. “You have a division between the haves and have-nots,” explained Carol Camp Yeakey, founding director of the Center on Urban Research & Public Policy and Interdisciplinary Program in Urban Studies at Washington University in St. Louis. “People on one side are prospering, and the people on the other side are not” (Harlan, 2014). The north city has a poverty rate around 40%. Around 25% of residents have not finished high school. There are distinct socioeconomic, cultural, and public policy differences to the north and south of the divide.
According to Elijah Anderson, “The inclination to violence springs from the circumstances of life among the ghetto poor—the lack of jobs that pay a living wage, the stigma of race, the fallout from rampant drug use and drug trafficking, and the resulting alienation and lack of hope for the future” (Cullen, Agnew, & Wilcox, 2018). These conditions create a subculture of violence that can be found in these neighborhoods. In “The Code of the Streets,” Anderson describes the formation of the code among those who experience “a profound sense of alienation from mainstream society and its institutions, who see no positive place for themselves in dominant culture, yet sense a need for dignity on some grounds, some clear sense of personal ‘respect’” (Cullen, Agnew, & Wilcox, 2018).
Many researchers have focused their studies on biological and environmental causes of trauma. A cultural divide and lack of protective factors affect an individual’s response to trauma. A poor family environment, with social factors such as poverty and abuse, adversely affect a person’s natural state.
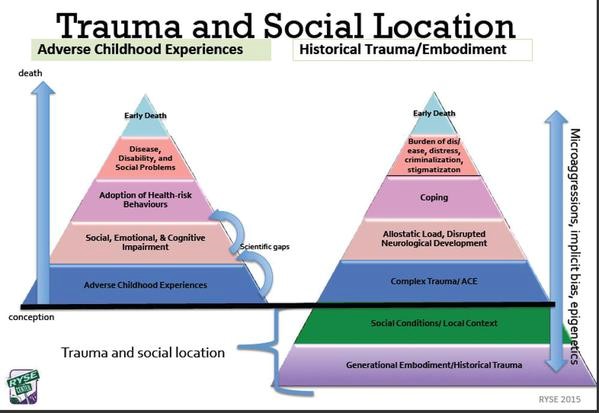
(Advocate, n.d.).
In comparison to Caucasians, ALANAS (African/Black Americans, Latina/Latino Americans, Asian/Pacific Islander Americans, and Native Americans) are more likely to develop PTSD after experiencing a traditionally defined traumatic event (Helms, Nicholas & Green, 2010). The men I work with describe seeing family members shot in the streets, friends gunned down in drive-by shootings, experienced sexual assaults by family members, and have no safe space to call home. Much like the veterans that Van Der Kolb spoke about, these men’s only support system are those that live the same life and have had experienced the same traumas.
I focus on this population of people to demonstrate how two different sets of life experiences, different skill sets, and how the lack of support systems contributes to PTSD. People fortunate enough to receive early intervention within a safe place are able to better understand the negative feelings they are having and how to put them into perspective. A trauma victim heals within strong family environments and positive peer relationships. The way a person makes sense of life events contributes to their recovery. Post traumatic growth occurs for those that are resilient and are able to gain an increased sense of personal strength and greater appreciation for life in general (Rousseau, 2020). It is imperative that mental health professionals and trauma researchers work toward developing more comprehensive understandings of the experiences of traumas for people growing up in poverty or unsafe neighborhood environments. In doing so, we can help trauma victims that do not have a safe place or positive support structures begin to heal and experience their own post traumatic growth.
References
Advocate. (n.d.). Retrieved from http://www.peace4gainesville.org/advocate.html.
Cullen, F. T., Agnew, R., & Wilcox, P. (2018). Criminological theory: Past to present: Essential readings. New York: Oxford University Press.
Harlan, C. (2014). In St. Louis, Delmar Boulevard is the line that divides a city by race and perspective. Retrieved from https://www.washingtonpost.com/national/in-st-louis-delmar-boulevard-is-the-line-that-divides-a-city-by-race-and-perspective/2014/08/22/de692962-a2ba-4f53-8bc3-54f88f848fdb_story.html?utm_term=.2bb00a09b6b1.
Helms, J., Nicolas, G., & Green, C. (January 01, 2010). Racism and Ethnoviolence as Trauma: Enhancing Professional Training. Traumatology, 16, 4, 53-62.
Rousseau, D. (2020). Module 1. Retrieved from https://learn.bu.edu/webapps/blackboard/execute/displayLearningUnit?course_id=_65989_1&content_id=_7783430_1&framesetWrapped=true.
Woytus, A. (2019). These are the St. Louis neighborhoods with the most crime-and this is what the police and residents are doing about it. Retrieved from https://www.stlmag.com/news/crime-data/.