Tagged: opioids
United States v. Safehouse: Could Philadelphia be the First State in the Nation to Implement a Supervised Drug Injection Site?
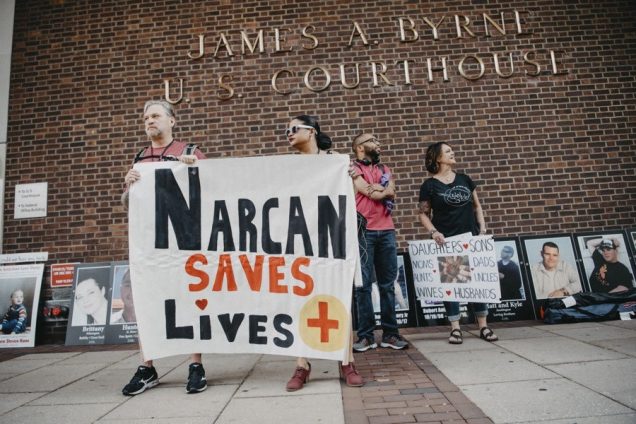
The opioid epidemic is one of the worst public health crises affecting the United States, and the rate of deaths resulting from opioid overdose has steadily increased. According to the Centers for Disease Control and Prevention, a record high of more than 70,000 people died of a drug overdose in the United States in 2017, and over 47,000 of those deaths were from opioid overdoses. As lawmakers attempt to address this epidemic through public health initiatives , health advocates increasingly recommend using supervised injection sites to curb overdose deaths. Though legal barriers to this in the US exist, a recent District Court ruling in United States v. Safehouse may have paved the way for implementation of the first site of this kind in the US.
Injection sites provide a space where those using intravenous drugs can inject under the supervision of a medical professional ready to intervene in the event of an overdose, instead of unsupervised use where an overdose is more likely to be deadly. Supervised injection sites, also called safe injection facilities or safe consumption spaces, are a tertiary preventative public health measure aimed at combating overdose deaths and decreasing public use. In these spaces, injection drug users can self-administer drugs they bring to the facility in a controlled, sanitary environment under medical supervision. The medical personnel on staff at the sites do not directly handle the drugs and are there purely to administer Naloxone, an overdose reversal drug, in case of an overdose.
Despite the growing global presence in Europe, Australia, and Canada, scientific support for safe injection sites, and the interest of several cities, including Philadelphia, Boston, New York, Seattle, and San Francisco it is not entirely certain they can be operated in the United States. The Controlled Substances Act § 856, which regulates the production, possession, and distribution of controlled substances, makes it a criminal offense to maintain a drug-involved premises. Most academics agree that this “Crack House” Statute forbids safe injection sites and the courts can not definitively decide if safe injection site violate federal law until one is operational.
However, recently these assumptions have been called into question. Safe injection site proponents in many states have been appealing to legislatures and public health officials for funding. This effort has been largely unsuccessful due to political opposition and the looming threat of a federal lawsuit. In Philadelphia, which has the highest overdose rate of any major US city, a poll found roughly half of Philadelphians support a proposed safe injection site. Safehouse is a Philadelphia nonprofit that seeks to build the first safe injection site in the nation. In January 2018, Philadelphia health officials gave Safehouse permission to move forward with only private funds—preventing the need for legislative backing and appropriations.
In February 2019, federal prosecutors launched a civil lawsuit asking the U.S. District Court to rule on the legality of the Safehouse supervised consumption site plan, rather than waiting for the site to be built and then bringing federal criminal charges. U.S. Attorney William McSwain, working with Pennsylvania-based prosecutors, is seeking a declaratory judgment that medically supervised consumption sites per se violate 21 U.S.C § 856(a)(2)— the federal “Crack House” statute.
In February 2020, the court issued United States v. Safehouse, ruling that Safehouse’s plan to build a site where people could bring previously obtained drugs and use them under medical supervision for the purpose of combating fatal overdoses does not violate the Controlled Substances Act. Judge McHugh, looking at Congressional intent, ruled that §856 “does not prohibit Safehouse’s proposed medically supervised consumption rooms because Safehouse does not plan to operate them ‘for the purpose of’ unlawful drug use within the meaning of the statute.” McHugh determines that at the time of enacting §856(a), Congress was focused on crack houses, not supervised drug injection sites. Even when amended in 2003, the focus was on “drug-fueled raves.” McHugh found that Congress neither expressly prohibited or authorized injection sites, so if §856(a) did not implicitly prohibit a consumption site, then implicit authorization naturally followed.
The question that the court addresses is whether the statute requires the defendant to know that third parties would enter their premises to consume illicit drugs, or rather that the defendant knowingly held their premises open for the purpose of facilitating illicit drug consumption. Judge McHugh concludes that the actor must “have acted for the proscribed purpose” to violate the statute. Therefore, the accused under a §856(a)(2) violation must have the purpose of facilitating illegal controlled substance use in the maintenance of a property.
Safehouse is planning “to make a place available for the purposes of reducing the harm of drug use, administering medical care, encouraging drug treatment, and connecting participants with social services.” The district court reasons that because of this, it could not conclude that Safehouse has, as a significant purpose, “the objective of facilitating drug use.”
In the wake of the ruling, U.S. Attorney McSwain announced that “this case is obviously far from over” and it is likely that the federal government will continue to litigate it. It is not unlikely that the Court that may hear this case on appeal disagrees with the District Court’s construction and strikes the legality of a supervised injection site based not on the intent of the person who controls the space, but the intent of the attendee of the site to use illicit drugs at that site, which has been the prevailing opinion up until the point of this ruling.
While the Safehouse case stands for an unexpected legal victory by way of the possibility of a supervised injection site to be opened in the United States, Philadelphia itself may not be the first state in the nation to implement one. The public sentiment in the wake of the decision was largely negative, with the local community being virulently opposed to the idea of a site being opened in the neighborhood from fear of what dangerous circumstances a site might attract. Plans to open the Safehouse site were put on indefinite hold. While proponents of Safehouse won the legal battle, winning over the community seems to be more of uphill battle than anticipated.
At this point in time, the legal position of supervised injection sites in the United States is tentatively positive. States who are looking to introduce this harm reduction initiative, and to be the first in the nation to do so, should take the opportunity to garner support from legislatures and local health care communities. While Philadelphia’s progression seems to be stymied, the District Court’s ruling provides significant legal precedent to ground encouragement for sites to be lobbied for in other states or cities that might not face the same type of community rejection that has prevented the opening of Safehouse.
 Zahraa Badat anticipates graduating from Boston University School of Law in May 2021.
Zahraa Badat anticipates graduating from Boston University School of Law in May 2021.
The Future of Supervised Injection Sites in Massachusetts and Beyond
With Massachusetts and the country facing a rising opioid overdose epidemic, lawmakers are looking to some controversial measures to curb overdose deaths. One of those measures being considered is supervised injection sites, also called safe injection sites or safe consumption spaces. Safe consumption spaces, of which there are 100 worldwide, are clean spaces where people can legally use pre-obtained drugs with supervision from healthcare professionals who aim to make injections as safe as possible while providing health care, counseling, and referral services to addicts. While safe injection sites have been successfully implemented in Canada, Australia, and Europe over the past 30 years, attempts to create such sites in San Francisco, Seattle, Boston, and more U.S. cities have not yet been successful. Beyond policy arguments as to whether these sites are effective, sites in the United States also face significant legal hurdles under federal law.
According to supporters of safe injection sites around the country and the world, the policy is an effective and relatively low-cost way to prevent overdose deaths and manage harm with no demonstrated consequences of increased drug use or increased crime. Opponents of safe injection sites, including Massachusetts Governor Charlie Baker, have pointed to increased opioid deaths in
recent years in Vancouver, which established its supervised consumption site Insite in 2003, to argue that safe injection sites are not actually effective in preventing overdose deaths. However, those arguments are misleading, as experts have stated that the increase in overdose deaths in Vancouver are due to the influx of fentanyl being added to drugs, and that Insite actually saw a 35% reduction in overdose deaths around the facility in the two years after it opened. While there are also studies questioning the efficacy of safe consumption sites—calling into question whether they have a significant impact on reducing deaths and reaching a significant amount of drug users—even the negative studies generally criticize safe consumption sites as being relatively ineffective as opposed to actively harmful. There are dozens of peer-reviewed scientific studies that have found that safe injection sites actually do significantly benefit those who are addicted to opioids and prevent opioid deaths. Notably, no death has ever been reported in an injection site, and a review of studies concluded that injection sites were associated with less outdoor drug use and did not appear to have any negative impacts on crime or drug use.
Despite the strong evidence backing the societal benefits of implementing and supporting safe injection sites, the policy faces significant legal and political obstacles in the United States. Perhaps the biggest hurdle that advocates of safe injection sites face is the potential legal liability of such sites under federal law and opposition from the Justice Department. The Controlled Substances Act makes it illegal to “knowingly open, lease, rent, use, or maintain any place, whether permanently or temporarily, for the purpose of manufacturing, distributing, or using any controlled substance,” as well as to knowingly manage such a place. The plain language of that law may render implementation of safe injection sites impossible without some change or exception carved out in federal law.
 However, advocates of safe injection sites do have a glimmer of hope that, once the first U.S. site is created, it will pass judicial muster through a creative legal argument proposed by law professor and drug policy expert Alex Kreit. In his paper, Kriet argues that a provision in the Controlled Substances Act providing immunity to state and local officials who commit drug crimes while enforcing local laws could protect safe injection sites from a crackdown by the federal government. Kreit has stated that the infrequently cited rule has previously been used in situations where authorities have seized marijuana and then returned it in states where marijuana has been legalized. Under this theory, those involved in safe injection sites would be protected so long as they were acting in accordance with a city ordinance or state law supporting safe injection sites. Other experts have expressed skepticism that such an argument would pass muster, however, with some stating that Kreit’s argument is a “stretch,” and that any path toward legality for safe injection sites lies in convincing the federal government not to target safe injection sites on public health grounds.
However, advocates of safe injection sites do have a glimmer of hope that, once the first U.S. site is created, it will pass judicial muster through a creative legal argument proposed by law professor and drug policy expert Alex Kreit. In his paper, Kriet argues that a provision in the Controlled Substances Act providing immunity to state and local officials who commit drug crimes while enforcing local laws could protect safe injection sites from a crackdown by the federal government. Kreit has stated that the infrequently cited rule has previously been used in situations where authorities have seized marijuana and then returned it in states where marijuana has been legalized. Under this theory, those involved in safe injection sites would be protected so long as they were acting in accordance with a city ordinance or state law supporting safe injection sites. Other experts have expressed skepticism that such an argument would pass muster, however, with some stating that Kreit’s argument is a “stretch,” and that any path toward legality for safe injection sites lies in convincing the federal government not to target safe injection sites on public health grounds.
If cities and states cannot find a legal workaround protecting those involved with the safe injection sites, advocates likely face an uphill battle in convincing their communities and the Justice Department to accept injection sites. Attempts at establishing sites have not been politically palatable, as demonstrated by efforts in San Francisco and Boston. California Governor Jerry Brown vetoed a bill that would have allowed supervised drug consumption sites in the state and went so far as to describe it as “enabling illegal drug use.” In Massachusetts, in addition to Governor Baker’s opposition to the idea of safe injection sites, the Senate ultimately stripped a provision authorizing safe injection sites from its comprehensive opioid bill this past legislative session, instead replacing the pilot program with a commission to study the feasibility of establishing such sites. In addition to opposition from state Governors and a lack of strong state government support, it seems highly unlikely that the current federal administration would turn a blind eye to safe injection sites on public health grounds. In addition to a statement from the Vermont U.S. Attorney’s Office criticizing the policy and affirming that the United States Attorney would impose ramifications under federal law, there have been multiple other instances indicating the administration’s hostility towards safe injection sites and similar policies. In August, Deputy Attorney General Rod Rosenstein wrote an op-ed in the New York Times opposing safe injection sites and emphasizing the fact that they violate federal law. The Justice Department also “promise[d] [a] crackdown” on supervised injection facilities on an NPR radio show.
While there is scientific and global community support for safe injection sites, their future in the United States is still unclear, especially under the current federal administration. Until there are more assurances that sites could operate without intervention from federal law enforcement, it seems that most cities and states that have been at the forefront of the push for safe injection sites do not have the political will or capital to open the country’s first site and become the guinea pig of the movement. Philadelphia, however, may be the one city willing to go first. In August, Philadelphia Health Commissioner Dr. Thomas Farley said that Rosenstein’s opposition and warnings from the Justice Department would not prevent Philadelphia officials from further exploring the idea. Currently, Philadelphia seems to be going forward with its plan to allow, but not publicly fund, a non-profit site called Safehouse, which could serve as a jumping off point for litigation determining the legality of the sites and potentially creating more certainty for other interested cities and states. As for Massachusetts, it seems unlikely that the Commonwealth will be establishing any safe injection sites in the near future, though the members of the commission created in last session’s opioid bill will no doubt keep a close eye on Philadelphia as its safe injection site plan comes to fruition.
Massachusetts’ “Death By Dealer” Bill is the Wrong Opioid Policy
On January 30, 2018, the Massachusetts Joint Committee on the Judiciary heard testimony on S. 2158, An Act Updating Laws Relating to Dangerous Drugs and Protecting Witnesses. Despite its relatively innocuous title, the bill, proposed by Governor Charlie Baker, represents a substantial scaling up of the War on Drugs in the Commonwealth.
Like many other states, Massachusetts is in the midst of a public health crisis. The opioid-related death rate in the state has surpassed the national average, with a nineteen percent increase in overdose deaths between 2015 and 2016. In addition, three-quarters of opioid-related deaths in 2016 involved fentanyl, a synthetic opioid that is roughly 50 times more potent than street heroin. As opioid overdoses decimate local communities, officials are understandably investigating ways to curb the epidemic, and one solution, to which legislatures are increasingly turning, entails drastically increasing punishment for drug crimes that result in death.
 For decades, federal prosecutors have been able to pursue stringent penalties in cases of “death by dealer.” Passed by Congress in 1988 in response to the highly publicized death of a University of Maryland basketball star who overdosed on cocaine just days after being drafted by the Boston Celtics, the so-called “Len Bias” law sets mandatory minimum sentences for selling drugs that lead to another person’s death. More recently, twenty states have adopted analogous laws, and several others have “McGyvered” existing homicide statutes—e.g., reckless homicide and felony murder—to prosecute the same offense. With Governor Baker’s bill, Massachusetts joins a number of additional states with pending legislation that would allow prosecutors to charge drug sellers with murder or manslaughter.
For decades, federal prosecutors have been able to pursue stringent penalties in cases of “death by dealer.” Passed by Congress in 1988 in response to the highly publicized death of a University of Maryland basketball star who overdosed on cocaine just days after being drafted by the Boston Celtics, the so-called “Len Bias” law sets mandatory minimum sentences for selling drugs that lead to another person’s death. More recently, twenty states have adopted analogous laws, and several others have “McGyvered” existing homicide statutes—e.g., reckless homicide and felony murder—to prosecute the same offense. With Governor Baker’s bill, Massachusetts joins a number of additional states with pending legislation that would allow prosecutors to charge drug sellers with murder or manslaughter.
While these laws may seem like a good idea at first—as a way to cripple the organized drug trade and to give prosecutors new tools to attack upper echelon drug traffickers—the criminalization of accidental overdose has a number of possible unintended consequences. Massachusetts legislators should carefully consider these effects that may backfire and exacerbate an already dire situation.
Although proponents argue that drug-induced homicide law will prevent future drug trafficking, there is broad consensus that harsh sentences have minimal, if any, deterrent effect. Contrary to conventional wisdom, studies have found that, among individuals facing drug-related charges, variations in prison and probation time have no impact on recidivism rates. The focus on supply reduction also seems misplaced: many studies suggest that market demand for drugs drives a continuous “replacement effect,” such that incarcerating drug dealers simply “open[s] the market for another seller.” Instead, such policies may inadvertently increase drug-related violence and lead to dangerous fluctuations in the contents of street drugs.
Drug-induced homicide laws also risk undermining Good Samaritan policies. As overdose deaths skyrocket, 37 states, including Massachusetts, have enacted laws to reduce the legal barriers to calling 911 in the event of an emergency. Most of the laws are limited to drug possession, however; they do not encompass drug selling or homicide. Although popular imagination places drug users and drug sellers in separate buckets, reality proves far blurrier: drug users frequently participate in the supply side of the market—whether by actively selling drugs or by helping in some way, such as acting as a lookout—in order to support their habits. Ostensibly intended to prosecute high-level drug suppliers, in practice, these statutes often ensnare family, friends, and acquaintances who supplied the drugs and who themselves may have a substance use disorder. In Wisconsin, an analysis of the 100 most recent drug-induced homicide prosecutions found that “nearly 90% of those charged were friends or relatives of the person who died, or people low in the supply chain who were often selling to support their own drug use.”
While prosecutors talk about “aggressively prosecuting those people that peddle the poison in our community,” users counter that “every drug-induced homicide charge that is made sends a ripple through the using community to not call 911 and might result in somebody else's death.” In fact, a recent study found that a majority of surveyed drug users feared calling 911 during an overdose due to concerns about criminal repercussions. Overall, then, treating overdose deaths as crime scenes and prosecuting overdose witnesses as perpetrators of murder or manslaughter limits the potential benefits of Good Samaritan legislation and other efforts to reduce overdose deaths.
Finally, punitive approaches, which place the blame for overdose deaths on drug sellers, focuses on the wrong problem. Criminal sanctions have the benefit of immediate visibility—they make it appear to constituents that policy makers are doing something. Public health approaches, on the other hand, are virtually invisible because, if successful, the harms that they target will never materialize. This “prevention paradox” often leads policy makers towards individualized, instantly tangible solutions to complex problems such as drug-induced homicide laws.
The opioid crisis is, fundamentally, a structural issue, rooted in poverty, lack of opportunity, and social isolation. Structural issues require structural solutions. Legislators are understandably grabbing at any and every straw to quell what seems like an intractable problem, but, at a time when much of the country seems poised to approach problematic substance use as a health issue, rather than a criminal one, it is critically important that Massachusetts policy makers carefully consider the ways in which S. 2158’s drug-induced homicide provision might backfire.
Rather than focusing on misguided “quick fixes” that further criminalize vulnerable populations, legislators should, instead, redirect their energies towards public health strategies with demonstrated effectiveness in reducing fatal overdoses. These include implementing comprehensive, evidence-based addiction prevention initiatives; increasing overdose education and naloxone access; promoting the use of medication-assisted treatment for opioid use disorders; and expanding and maintaining insurance coverage for addiction treatment. The United States has been trying to arrest its way out of substance use and addiction for decades, and today’s crisis attests to the futility of that approach. If our policy makers are serious about ending the opioid epidemic in the Commonwealth, they need to shift their focus from policing and prisons to people and public health.
 Alexandra Arnold anticipates graduating Boston University School of Law in May 2019.
Alexandra Arnold anticipates graduating Boston University School of Law in May 2019.
A Lackluster Response to the 64,000 Opioid Overdose Deaths Per Year
The Opioid Epidemic stands apart from past drug crises this country has experienced. Not only is this the deadliest drug crisis the country has experienced, this epidemic is a result of a “perfect storm.” A shift in the medical field to focusing on the treatment of pain changed opioid prescribing practices and encouraged an increase in marketing practices of opioid pharmaceutical companies, resulting in America being the world’s leader in opioid prescriptions. Congress, through the Bipartisan Task Force to Combat the Heroin Epidemic, made some progress addressing opioids during the Obama Administration, but with the change in administration the efforts seem stalled.
In 2015, doctors prescribed enough opioids to medicate every American around the clock for three weeks. Even as doctors started to prescribe fewer opioids, in 2016 enough opioids were prescribed to fill a bottle for every adult in America. The increase in opioid prescriptions came at the same time as there was a shortage of workers in addiction and recovery, allowing for only 10 percent of Americans with substance use disorder to receive the necessary treatment. This “perfect storm” created a massive swell in opioid addictions. As it became more difficult to obtain prescription opioids, addicts sought a stronger high and many turned to illegal opioids, such as heroin and fentanyl. Nearly 80 percent of Americans addicted to heroin started with misuse of prescription drugs.
The death of Philip Seymour Hoffman in 2014 from a heroin overdose put a spotlight on the crisis. Despite recognizing that there was a nation-wide epidemic, the country took a lackluster response and overdose deaths continued to spike. The National Center for Health Statistics, Centers for Disease Control and Prevention, and the National Institute on Drug Abuse have reported only an increase in the overdose deaths. The U.S. government estimated about 64,000 overdose deaths for 2016. With the epidemic claiming a record number of lives per day, all of the 2016 presidential candidates spoke about personal stories or plans of action for combatting the epidemic. Most of the candidates agreed that the federal government should provide resources to the states to help combat the epidemic with a focus on treatment. Some of the other candidates focused on stopping the flow of drugs coming across the border, including now President Donald Trump.
In March 2017, President Trump established the President’s Commission on Combating Drug Addiction and the Opioid Crisis. The Commission members include Former Governor Chris Christie of New Jersey, Governor Charlie Baker of Massachusetts, Governor Roy Cooper of North Carolina, Former Congressman Patrick Kennedy of Rhode Island, Professor Bertha Madras, and Florida Attorney General Pam Bondi. On November 1, 2017, the Commission issued a final report with more than 50 recommendations (see, page 7). They included increasing data sharing of state-based prescription drug monitoring programs, changing privacy regulations to allow healthcare providers easier access to information about patients with substance use disorder, equipping all law enforcement officers with naloxone, and enforcing the Mental Health Parity and Addiction Equity Act. In addition, the Commission recommended a national multi-media campaign to help fight the epidemic, more federal funding for the states, drug courts in every federal district court, and enhanced penalties for drug trafficking to reduce the supply of opioids.
Even prior to the issuance of the report, President Trump declared the Opioid Epidemic a public health emergency. The President stated “[t]he best way to prevent drug addiction and overdose is to prevent people from abusing drugs in the first place. If they don’t start, they won’t have a problem,” but until his 2019 budget proposal the President’s Administration failed to request funding to combat the epidemic. Congressman Patrick Kennedy, a vocal critic of the limited action taken by the President, explained, “[t]he emergency declaration has accomplished little because there’s no funding behind it. You can’t expect to stem the tide of a public health crisis that is claiming over 64,000 lives per year without putting your money where your mouth is.”
The President’s focus has been on increasing funding for law enforcement. On January 10, 2018, the President signed the INTERDICT Act which provides funding to U.S. Customs and Border Protection to assist with the detection and interception of illicit fentanyl. Increased enforcement may be part of the solution, but some Congressional leaders believe there is more than just one solution and have said the epidemic must be addressed on many fronts.
In 2015, Representatives Ann McLane Kuster and Frank Guinta from New Hampshire, a state that has the highest fentanyl overdose deaths per capita, created the Congressional Bipartisan Task Force to Combat the Heroin Epidemic. From its inception, the task force has gained members from both parties, and now has more than 100 members. The Task Force pushes a legislative agenda, as well as holds informational hearings. Under President Obama’s Administration, the Task Force was able to pass several pieces of legislation, including the 21st Century Cures Act, and the Comprehensive Addiction & Recovery Act (CARA). The CARA Act is currently the main source of funding for the opioid epidemic, but the funding will run out in 2018. In response to the “perfect storm” that created this epidemic, CARA has six pillars of response, including prevention, treatment, recovery, law enforcement, criminal justice reform, and overdose reversal.
On January 10, 2018, the Task Force released its 2018 legislative agenda. The agenda includes bills focusing on prevention, treatment, law enforcement, and prescribing practices. Several of the bills include federal funding and grants. After the Task Force called for an increase in funding to combat the epidemic, Congress passed $6 billion in the 2018 budget. Some have been critical of the amount of funds dedicated to the epidemic, and compared it to the $24 billion a year that was dedicated to addressing the HIV/AIDS crisis.
On February 9, 2018, Purdue Pharma, the maker of OxyContin, announced it had laid off employees whose job was direct promotion of the drug to doctors. Purdue Pharma is currently facing dozens of lawsuits for deceptive marketing practices. It is unclear if the company’s change in promotion practices will alter prescribing practices of doctors, who are already familiar with the drug. To make a significant impact on the epidemic, real change needs to happen outside of Purdue Pharma’s promoting practices.
The U.S. Surgeon General issued a public health advisory encouraging Americans to routinely carry naloxone on April 5, 2018, which is the first advisory issued since the 2005 warning against drinking alcohol while pregnant. Access to naloxone would come in part from the $6 billion in the 2018 budget which has allocated grants for naloxone so states can hand it out for free; however, there is also reliance on naloxone manufacturers keeping costs low. The Surgeon General explained that naloxone can be a “touch point that leads to recovery.” However, more in line with the Trump Administration, the Surgeon General believes that the involvement of law enforcement is necessary to solving the epidemic.
A tough-on-crime approach and focus on providing funding strictly for law enforcement, as President Trump has encouraged, is not the answer. The country responded to the crack cocaine drug crisis with a tough-on-crime approach and strict sentencing guidelines. That led to extraordinary incarceration rates, especially for African Americans, and failed to address the issue of addiction as a disease. The country should learn from its mistakes, take a more well-rounded approach, as suggested by the Surgeon General and the Bipartisan Task Force, and implement a long-term solution. Congress must not only provide funding for law enforcement, but should increase treatment and recovery for substance use disorder, implement better prescription drug monitoring programs, start country-wide drug court programs, and educate Americans and doctors about the disease of addiction and risk of opioids. People are dying every day in this country from opioid overdoses, and every time Congress delays we lose another life.
 Mikayla Foster anticipates graduating from Boston University School of Law in May 2019.
Mikayla Foster anticipates graduating from Boston University School of Law in May 2019.
Pharmacies Try Their Hand at Opioid Policy
The opioid crisis has continued to grab national attention, as total drug overdoses hit yet another historic high in 2016. One of the nation’s largest pharmacies, CVS, recently joined the debate by announcing a new national opioid policy.
In February 2018, CVS started capping new opioid prescriptions at a seven-day supply. Additionally, CVS is limiting daily doses to 90 morphine milligram equivalents (MME) and requires medical providers to prescribe immediate-release opioids before attempting extended-release versions. The policy itself is unremarkable. CVS is merely adopting the CDC’s prescribing guidelines. In fact, 17 states have done the same or equivalent, including Massachusetts. And while it may appear strange for a retailer like CVS to forcibly limit its own sales, both pharmacies and pharmaceutical companies have faced a growing threat of litigation in recent years over the marketing and sale of prescription opioids.
Medical providers, chronic pain patients, and some drug policy experts have lodged a number of concerns in response to CVS’s new policy. These concerns not only identify some of the closely held interests in the opioid debate but also demonstrate the challenges of developing effective policy against a crisis that is rapidly evolving.
The Costs
Opioid policies fall into three main categories: preventive, treatment, and punitive. The CVS policy aims to prevent the development of new opioid use disorders (OUDs). In an effort to minimize unintended consequences, the policy carves out two administrative exceptions: first, doctors may request exemptions for certain patients, and second, employers and insurers can opt out of the program altogether. The CVS policy also aligns itself with CDC guidelines in exempting patients who are in “active cancer treatment, palliative care, or hospice care.”
While this may reassure cancer patients, other patients with chronic pain have expressed cause for alarm. For one, their access to opioids is already subject to an ongoing and heated debate within the medical community. Limited data on long-term opioid use for chronic pain management has bisected medical experts’ opinions on the evidence base, ethics, and ramifications of prescribing decisions. In 2016, the CDC entered the fray. While its guidelines recommend heavily individualized opioid treatment decisions, the CDC director placed his thumb on the scale by declaring that “[m]anagement of chronic pain is an art and a science. The science of opioids for chronic pain is clear — for the vast majority of patients, the known, serious, and too-often fatal risks far outweigh the unproven and transient benefits.”
Chronic pain patients disagree that the data are so clear-cut. Moreover, they allege that the national opioid narrative is eliciting a fear-based response among medical providers at a negative cost to their treatment. Chronic pain patients report that their providers increasingly treat them like “addicts,” an inappropriately stigmatizing term that in these cases also ignores critical diagnostic differences between substance dependency and a substance use disorder. The result can be forced reductions to a patient’s opioid prescription without warning (known as involuntary tapering) or in extreme cases a blanket office policy against prescribing opioids altogether. It is early days—too early for clear data in fact—but reports of patient suicides in the wake of involuntary tapering have already surfaced.
 The CDC does not expressly require a physician to involuntarily taper a patient off of opioids. In fact, the CDC vests the authority for such individualized prescribing decisions in physicians. However, the DEA, which grants physicians’ prescribing licenses, admittedly muddled that message when it proposed broad cuts to opioid production: a 25% decrease in 2017 and a 20% decrease in 2018. Moreover, punitive DEA actions against physicians regarding opioid prescription conduct increased fivefold between 2011-2016. While the penalties are clear and steep (including loss of medical licensure and criminal charges), what conduct triggers those penalties is less clear. Thus, the combination of liabilities without a clear safe harbor incentivizes an overly strict interpretation of federal policies in ways that may harm patients.
The CDC does not expressly require a physician to involuntarily taper a patient off of opioids. In fact, the CDC vests the authority for such individualized prescribing decisions in physicians. However, the DEA, which grants physicians’ prescribing licenses, admittedly muddled that message when it proposed broad cuts to opioid production: a 25% decrease in 2017 and a 20% decrease in 2018. Moreover, punitive DEA actions against physicians regarding opioid prescription conduct increased fivefold between 2011-2016. While the penalties are clear and steep (including loss of medical licensure and criminal charges), what conduct triggers those penalties is less clear. Thus, the combination of liabilities without a clear safe harbor incentivizes an overly strict interpretation of federal policies in ways that may harm patients.
Beyond the legal liabilities, physicians have also voiced concerns over the increasing intrusion of third parties into treatment decisions. The CVS policy allows a doctor to request exemptions for certain patients, but does not specify its criteria for granting exemptions or if there are caps on the number of exemptions a doctor may request or receive. Some doctors worry the additional administrative requirements to apply for CVS exemptions will burden already overtaxed primary care physicians, leaving patients with delayed or insufficient care. For example, one study found that physicians already spend two hours on paperwork for every hour of treating patients. The CVS policy will increase that paperwork burden for physicians who choose to file for opioid patient exemptions.
Without further research on long-term opioid use, clear safe harbors for prescribing compliance, and a significant increase in the number of medical specialists trained in pain management, some patients and doctors share the concern that this prevention policy will come at unintentional costs to patients with chronic pain.
The Benefits
Much of policy derives from a cost-benefit analysis. If prescription opioids are the source of most new cases of OUDs, then some risk to patients with opioid dependencies (like those managing chronic pain) may arguably be worth strictly limiting their supply. Thus, the $78.5 billion question remains: are prescription opioids presently the main cause of new OUD cases?
A growing subset of drug policy experts say no. While prescription opioids undoubtedly contributed to the opioid epidemic in the past, recent data show that opioid prescriptions continuously decreased from 2010-2015. During that same time span however, opioid mortalities continuously increased. In fact, heroin increasingly represents the initiating opioid of use for new OUD cases, not oxycodone or other prescriptions. These data suggest that the over-prescription of opioids has been largely corrected and that new and stricter prescription limits moving forward may offer only marginal benefits.
The debate over CVS’s initiative mirrors many of the challenges of developing effective opioid policy at the state level. The opioid epidemic is rapidly evolving whereas drafting and passing legislation can take years to accomplish. In that same time span, the drop in prescription rates between 2010-2015 as well as the emergence of heroin as an initiating opioid have shifted the opioid epidemic, throwing into question just recently passed prescription-focused legislation. In short, the opioid crisis is both testing and demonstrating the limits of the legislative process.
Second, even if a legislature could sustain a multi-decade focus on continually revising opioid legislation, any attempt to do so effectively would require massive data gathering. Currently however, state medical examiners have already passed their breaking points, whether from running out of room, running out of money, or burnout. Yet these examiners play a crucial role in accurately identifying the cause of death for overdoses. Thus, even accurately tracking changes in cause of death alone would necessitate a massive influx of resources, in terms of additional personnel, time, and training for standardization. Beyond tracking overdoses, states would furthermore have to allocate additional resources to continuously monitor changes in initiating opioid use and to what extent supply limitations (like those currently placed on prescriptions) result in a substitute demand for more harmful illicit opioids like fentanyl.
Third and finally, the unintended effects of legislation matter just as much as the intended. A complex mesh of societal, punitive, and regulatory forces have created powerful disincentives for physicians to prescribe opioids or treat patients who need them. In particular, the stigmatization of chronic pain patients incentivizes withholding treatment for moralistic rather than medical reasons. The threat of criminal prosecution and loss of medical licensure incentivizes avoiding even relatively benign conduct for fear of triggering DEA or state investigation. Finally, the paperwork barriers formed by each new layer of regulatory compliance incentivize avoiding time-consuming patients, like those who require opioids. Thus, the exemptions that CVS and other state policies designed to safeguard individualized treatment decisions are likely insufficient to counterbalance the opposing disincentives. Effective policymaking requires a careful calculation of both direct and indirect incentives, far beyond the scope of a single prescription policy.
Going forward, CVS (and the states) should consider policy alternatives that expand provider choices rather than restrict them. For example, CVS could begin offering the abuse deterrent formulations (ADFs) of opioids. The FDA recommends ADFs as they offer the same pharmacological benefits as regular opioids but exist in a form that is harder to physically alter for off-label use. Currently, CVS does not cover any of the ten ADFs approved by the FDA. By offering a new prescriptive tool instead of restricting an existing one, this alternative might maintain some of the same intended preventive benefits without triggering an incentive to drop chronic pain patients.
Moreover, the addition of ADF coverage would allow for greater flexibility on a state level. Many states are in the process of or have recently completed crafting comprehensive legislative packages (including combinations of preventive, treatment, and punitive solutions). CVS’s uniform national policy may interfere with these efforts and make addressing unique state needs more challenging than necessary.
In summary, the benefits of CVS’s opioid policy are unlikely to outweigh its harms. The CVS policy provides no new guidance as it merely mimics the existing CDC policy, but it does add new layers of time-consuming compliance for providers pursuing medically-valid exemptions. Pharmacies and other retailers would do better to provide additional support to the existing state and federal opioid infrastructure than begin imposing new requirements upon it.
 Caitlin Scott anticipates graduating Boston University School of Law in May 2019 and plans to practice Health Law.
Caitlin Scott anticipates graduating Boston University School of Law in May 2019 and plans to practice Health Law.